口腔颌面外科手术对上呼吸道解剖结构影响大,为预防及改善上呼吸道梗阻症状,术后需留置人工气道,其引起的物理及化学性刺激远超过其他种类手术,易诱发恶心呕吐[1]、咽部疼痛[2-6]及呛咳等[5-7]不良反应,患者对治疗过程体验感差,严重时可危及围手术期安全。利多卡因为酰胺类局部麻醉用药,有良好的黏膜穿透性,表面麻醉效果强,经静脉注射后对中枢神经系统有兴奋和抑制双相作用,且其作用效果及毒性随剂量增加而增强。已有研究证实利多卡因可减轻气管插管后出现的咳嗽、咽喉疼痛等症状,缓解全身麻醉患者术后苏醒期间的不适[8-9]。本研究对口腔颌面手术后留置经鼻气管插管患者使用利多卡因静脉持续泵注及气道表面麻醉的方案,观察利多卡因在提高口腔颌面术后留置人工气道患者舒适性方面的作用。
1 对象和方法 1.1 研究对象选择上海交通大学医学院附属第九人民医院2020年4-6月拟接受择期全身麻醉下口腔颌面外科手术的患者176例。纳入标准:(1)留置经鼻气管插管≥12 h;(2)美国麻醉医师学会(American Society of Anesthesiologists,ASA)分级为Ⅰ或Ⅱ级。排除标准:(1)经口气管插管和气管切开的患者;(2)需药物镇静的患者;(3)合并严重心脑血管疾病或肝、肾等重要脏器异常者;(4)合并慢性呼吸道疾病,如慢性阻塞性肺疾病或支气管哮喘等;(5)术前已存在呼吸系统感染者;(6)对酰胺类局部麻醉药物过敏者;(7)对试验药物有不良反应者;(8)不愿意完成试验流程或不能理解试验者。本研究通过上海交通大学医学院附属第九人民医院伦理委员会审批(2016-192-T136),所有参与试验者均签署书面知情同意书。
1.2 药物盐酸利多卡因注射液为山东华鲁制药有限公司产品(规格:0.1 g/5 mL;生产批号:国药准字H37022147);利多卡因气雾剂为广州市香雪制药股份有限公司产品(规格:每罐内容物50 g,内含利多卡因1.5 g;生产批号:国药准字H20031189)。
1.3 分组和给药方法本研究为随机、单盲、平行对照临床试验。根据计算机生成的随机数,将口腔颌面手术后患者随机分为3组:利多卡因静脉泵注组(35例)、利多卡因表面麻醉组(35例)、对照组(36例)。
入选病例手术结束后转入麻醉复苏室苏醒,待Steward苏醒评分达4分以上时转入外科重症监护室(surgical intensive care unit,SICU)。利多卡因静脉泵注组患者给予1.5 mg/kg(20 mg/mL)负荷剂量盐酸利多卡因注射液静脉推注,然后以1.5 mg•kg-1•h-1(使用生理盐水稀释至10 mg/mL)持续泵注12 h。利多卡因表面麻醉组患者从转入SICU开始,每隔2 h通过人工气道喷注利多卡因气雾剂2次,每次间隔2 min,每次2喷(每喷含利多卡因约16 mg)。对照组患者静脉推注0.075 mL/kg的生理盐水作为负荷剂量,之后以0.15 mL•kg-1•h-1持续泵注12 h。各组患者均在SICU给予相同的抗感染、化痰、消肿等治疗,常规监测出入量,根据患者病情适当补液及对症支持治疗。每隔2 h定时清理患者口腔及气道分泌物,若患者有需求则随时清理。每隔4 h放松人工气道套囊5 min,然后再注入空气,维持套囊压力在1.96 kPa左右[10]。
1.4 观察指标记录患者的人口学特征(年龄、性别、体重、身高、BMI)及ASA分级、术前血常规、术前凝血功能、手术时间、麻醉时间、术中出血量、输血量、补液量、尿量等临床资料。从转入SICU即刻开始,每小时记录1次收缩压(systolic blood pressure,SBP)、舒张压(diastolic blood pressure,DBP)、平均动脉压(mean arterial pressure,MAP)、心率、呼吸频率、切口疼痛视觉模拟量表(visual analogue scale,VAS)评分、咽喉疼痛VAS评分,以及每小时内恶心呕吐和呛咳的发生频次。观察并记录患者主诉及心律失常和局部麻醉药毒性反应的发生情况。
1.5 统计学处理采用SPSS 25.0软件进行统计学分析。符合正态分布且方差齐的计量资料以x±s表示,转入SICU后1~12 h各指标总体组间比较及各组随时间变化趋势的比较采用单因素方差分析;不符合正态分布的计量资料以中位数(下四分位数,上四分位数)表示,转入SICU后1~12 h各指标总体组间比较及各组随时间变化趋势的比较采用Kruskal-Wallis H检验,同时使用Mood中位数检验及Jonckheere-Terpstra检验验证统计结果。计数资料以例数表示,组间比较采用χ2检验。检验水准(α)为0.05。
2 结果 2.1 各组患者基本特征本研究共纳入106例口腔颌面手术后留置经鼻气管插管患者,年龄为18~62岁,男57例、女49例,ASAⅠ级25例、Ⅱ级81例。利多卡因静脉泵注组和利多卡因表面麻醉组各35例,对照组36例,3组患者的年龄、性别、体重、身高、BMI、ASA分级、术前血常规(血红蛋白、血小板计数、白蛋白)、术前凝血功能(凝血酶原时间、活化部分凝血活酶时间、纤维蛋白原)、手术时间、麻醉时间、术中出血量、输血量、补液量、尿量差异均无统计学意义(P均>0.05),见表 1。
|
|
表 1 口腔颌面手术后留置经鼻气管插管患者的基本特征 Tab 1 Basic characteristics of patients with transnasal endotracheal intubation after oral and maxillofacial surgery |
2.2 各组间患者手术结束后转入SICU后1~12 h总体生命体征及舒适度的比较
与对照组相比,利多卡因静脉泵注及表面麻醉不会对口腔颌面手术后留置经鼻气管插管患者的SBP、DBP、MAP和心率造成影响(P均>0.05),但两组患者的呼吸频率均降低(P均<0.05)。利多卡因静脉泵注组与利多卡因表面麻醉组患者的SBP、DBP、MAP、心率和呼吸频率差异均无统计学意义(P均>0.05)。与对照组相比,利多卡因静脉泵注能有效提高患者的舒适度,表现为切口疼痛及咽喉疼痛VAS评分均降低(P均<0.05),恶心呕吐及呛咳的发生频次均减少(P均<0.05);利多卡因表面麻醉也能改善患者的舒适度,咽喉疼痛VAS评分、恶心呕吐发生频次及呛咳发生频次均减少(P均<0.05),但不能缓解手术切口疼痛,切口疼痛VAS评分与对照组相比差异无统计学意义(P>0.05)。与利多卡因表面麻醉相比,利多卡因静脉泵注提高患者舒适度的效果更优,表现为切口疼痛及咽喉疼痛VAS评分均更低(P均<0.05),呛咳发生频次更少(P<0.05)。见表 2。
|
|
表 2 各组口腔颌面手术后留置经鼻气管插管患者转入SICU后1~12 h的总体生命体征及舒适度 Tab 2 Vital signs and comfort of patients with transnasal endotracheal intubation after oral and maxillofacial surgery in each group during 1-12 h in SICU |
2.3 各组患者的生命体征及舒适度随时间的变化趋势
在手术结束后转入SICU后1~12 h,利多卡因静脉泵注组患者的SBP、DBP和MAP均逐渐降低(P均<0.05),心率和呼吸频率均无明显变化(P均>0.05,图 1A);利多卡因表面麻醉组患者的SBP、MAP均逐渐降低(P<0.05),DBP、心率和呼吸频率均无明显变化(P均>0.05,图 1B);对照组患者的生命体征变化无明显变化(P均>0.05,图 1C)。在手术结束后转入SICU后1~12 h,利多卡因静脉泵注组、利多卡因表面麻醉组及对照组患者的切口疼痛和咽喉疼痛VAS评分均无明显变化(P均>0.05,图 2);而3组患者的恶心呕吐发生频次和呛咳发生频次均呈降低趋势(P均<0.05,图 3)。
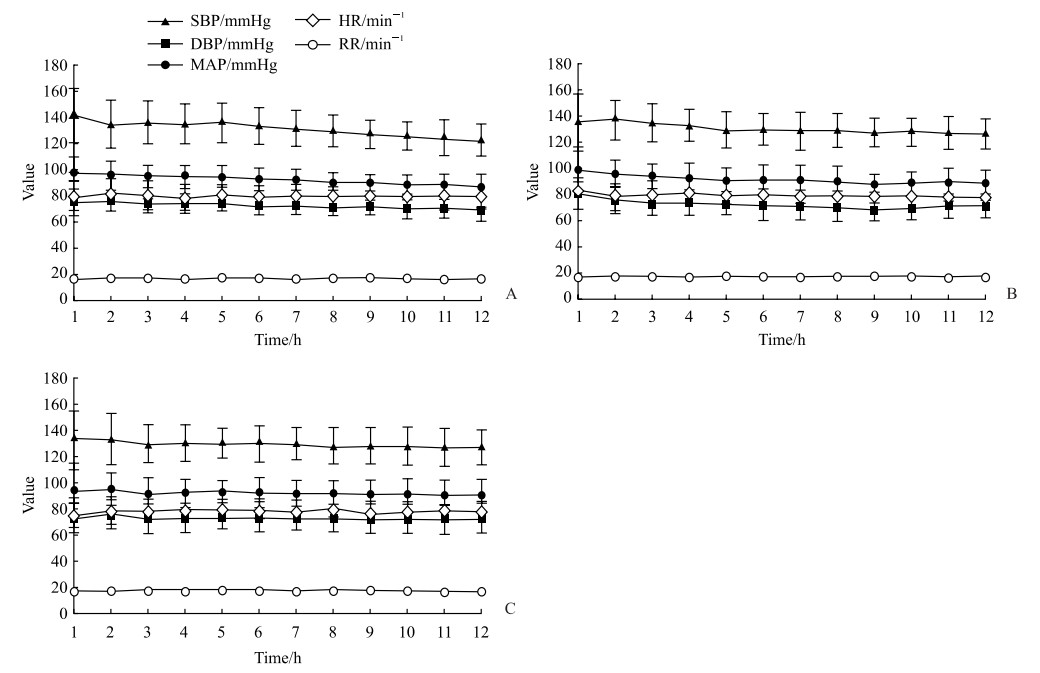
|
图 1 各组口腔颌面手术后留置经鼻气管插管患者转入SICU后1~12 h生命体征的变化趋势 Fig 1 Trends of vital signs of patients with transnasal endotracheal intubation after oral and maxillofacial surgery in each group during 1-12 h in SICU A: In the lidocaine pumping group (n=35), the SBP, DBP and MAP significantly decreased over time (all P < 0.05), while the HR and RR had no significant change; B: In the lidocaine spray group (n=35), the SBP and MAP were significantly decreased over time (both P < 0.05), while the DBP, HR and RR had no significant change; C: In the control group (n=36), none of the vital signs were significantly changed. 1 mmHg=0.133 kPa. x±s. SICU: Surgical intensive care unit; SBP: Systolic blood pressure; DBP: Diastolic blood pressure; MAP: Mean arterial pressure; HR: Heart rate; RR: Respiratory rate. |

|
图 2 各组口腔颌面手术后留置经鼻气管插管患者转入SICU后1~12 h切口疼痛和咽喉疼痛VAS评分的变化趋势 Fig 2 Trends of incision pain and sore throat VAS scores of patients with transnasal endotracheal intubation after oral and maxillofacial surgery in each group during 1-12 h in SICU A: The incision pain VAS score; B: The postoperative sore throat VAS score. x±s. SICU: Surgical intensive care unit; VAS: Visual analogue scale. |

|
图 3 各组所有口腔颌面手术后留置经鼻气管插管患者转入SICU后1~12 h发生恶心呕吐和呛咳的总频次变化趋势 Fig 3 Trends of total frequencies of nausea/vomiting and cough of all patients with transnasal endotracheal intubation after oral and maxillofacial surgery in each group during 1-12 h in SICU A: Total frequency of nausea/vomiting significantly decreased over time in the 3 groups (all P<0.05); B: Total frequency of cough significantly decreased over time in the 3 groups (all P<0.05). SICU: Surgical intensive care unit. |
2.4 各组患者不良反应发生情况
利多卡因静脉泵注组1例、利多卡因表面麻醉组2例患者有胸闷主诉,生命体征均无明显变化,且在10 min内自行缓解。利多卡因静脉泵注组2例患者发生皮疹,判断非利多卡因诱发,未进行特殊处理,自行缓解。所有患者均未发生呼吸异常、血压异常、心律失常及局部麻醉药毒性等严重不良反应。
3 讨论留置人工气道可诱发恶心呕吐(发生率约为20%[1])、咽喉疼痛(发生率为21%~72%[2-6])及呛咳(发生率为15%~94%[5-7])等不良反应,影响患者舒适度,严重时甚至危及患者生命安全。临床上可采取多种措施减少气道并发症,如深麻醉下拔管[11]、阿片类药物静脉使用[12]、局部麻醉[13]及气管插管套囊内注射局部麻醉药[8-9, 14]等。但部分行口腔颌面手术的患者(如行单侧颈内动脉结扎术的患者)需留置人工气道以预防上呼吸道梗阻,并要求患者保持清醒以便随时评估神志变化,还需维持生命体征稳定以防发生不良后果。对于这些患者,上述处理方案均有局限性,不能满足所需,本研究采用的利多卡因静脉持续泵注或气道内表面麻醉方案降低了口腔颌面手术后人工气道诱发的恶心呕吐、咽喉疼痛、呛咳等不良反应的发生率,维持了血压、心率及呼吸等生命体征的稳定性,提高了患者围手术期舒适度。
术后疼痛合并存在炎性及神经性疼痛,临床研究表明静脉注射利多卡因能促进手术切口愈合、镇痛、改善凝血等[15],是围手术期镇痛治疗的安全替代方案,能够有效提高患者围手术期舒适度[16-17]。本研究结果显示静脉注射利多卡因能有效抑制手术切口疼痛,气道内表面麻醉则不能,与相关研究结果[16]一致。利多卡因静脉泵注及气道内表面麻醉均能改善咽喉疼痛,且静脉泵注的改善效果优于气道内表面麻醉。此外,利多卡因静脉泵注及气道内表面麻醉均能改善恶心呕吐和呛咳症状,两组改善恶心呕吐症状的效果无明显差异,但利多卡因静脉泵注对呛咳症状的缓解效果优于气道内表面麻醉。利多卡因静脉泵注及气道内表面麻醉不会对口腔颌面手术后留置经鼻气管插管患者的SBP、DBP、MAP和心率造成影响,但呼吸频率均降低。这可能是因为患者接受利多卡因干预后,恶心呕吐及呛咳的发生频次减少、咽喉疼痛改善使舒适度提升,易于入睡,出现生理性的呼吸频率下降;同时患者留置经鼻气管插管,生理无效腔减少,变相增加潮气量,呼吸频率相应下降。
在手术结束后转入SICU 1~12 h,各组患者的恶心呕吐及呛咳发生频次均随时间延长而逐渐减少。利多卡因静脉泵注组和利多卡因表面麻醉组出现这一现象可能是因为利多卡因的作用及患者对经鼻气管插管的耐受性增强,而对照组仅归因于患者耐受性增强。口腔颌面部手术的切口疼痛刺激较轻,切口疼痛VAS评分也偏低,少量利多卡因即可有效抑制术区疼痛,故利多卡因对切口疼痛的抑制效果不会随药物浓度的增加而增强,也不随时间发生变化。利多卡因表面麻醉组及对照组患者的切口疼痛VAS评分差异无统计学意义,也不随时间变化。本研究中,利多卡因静脉泵注组药物使用量较小,若增大利多卡因用量,提升血药浓度,可能会进一步缓解经鼻气管插管所致的咽喉疼痛,但药物副作用的发生风险也将随之升高;利多卡因表面麻醉组间断2 h给药,若缩短间隔时间,增加利多卡因给药频率,或更换为其他作用时间更长的表面麻醉药物,咽喉疼痛可能随时间改善。利多卡因的最佳使用剂量和给药方式还需进一步探讨。
已有多项研究证明了利多卡因静脉注射的安全性[18-19]。在本研究中,利多卡因静脉泵注组有1例患者主诉胸闷,2例患者发生皮疹;利多卡因表面麻醉组有2例患者主诉胸闷,以上5例患者症状发生时生命体征均无明显变化,未予特殊处理均自行缓解。试验结束后(转入SICU 12 h后)再次询问主诉胸闷的3例患者,均对胸闷主诉无记忆。整个试验流程中所有患者均未发生呼吸异常、血压异常、心律失常及局部麻醉药毒性等严重不良反应。
本研究结果显示利多卡因静脉泵注及气道内表面麻醉能有效改善口腔颌面手术后留置经鼻气管插管患者的咽喉疼痛症状、减少恶心呕吐和呛咳发生频次,且无明显不良反应;利多卡因静脉泵注改善咽喉疼痛和抑制呛咳的效果更佳,并可缓解切口疼痛。由于利多卡因有神经及心血管方面的作用并且肝脏首剂效应明显,本研究在样本选择时剔除了神经系统、心血管系统及肝肾功能异常的病例,排除了ASA Ⅲ级及以上的择期手术患者,因此本研究结论是否适用于基础疾病复杂的患者有待进一步研究。
| [1] |
PORHOMAYON J, FARID S D, EL-SOLH A A, ADLPARVAR G, NADER N D. The impact of endotracheal tube vs. laryngeal mask airway on the incidence of postoperative nausea and vomiting: a systemic review and meta-analysis[J]. Middle East J Anaesthesiol, 2015, 23: 9-16. |
| [2] |
CLAYTON-SMITH A, BENNETT K, ALSTON R P, ADAMS G, BROWN G, HAWTHORNE T, et al. A comparison of the efficacy and adverse effects of double-lumen endobronchial tubes and bronchial blockers in thoracic surgery: a systematic review and meta-analysis of randomized controlled trials[J]. J Cardiothorac Vasc Anesth, 2015, 29: 955-66. DOI:10.1053/j.jvca.2014.11.017 |
| [3] |
CHANG J E, KIM H, HAN S H, LEE J M, JI S, HWANG J Y. Effect of endotracheal tube cuff shape on postoperative sore throat after endotracheal intubation[J]. Anesth Analg, 2017, 125: 1240-1245. DOI:10.1213/ANE.0000000000001933 |
| [4] |
TANAKA Y, NAKAYAMA T, NISHIMORI M, TSUJIMURA Y, KAWAGUCHI M, SATO Y. Lidocaine for preventing postoperative sore throat[J/OL]. Cochrane Database Syst Rev, 2015: CD004081. DOI: 10.1002/14651858.CD004081.pub3.
|
| [5] |
BANIHASHEM N, ALIJANPOUR E, HASANNASAB B, ZAREI A. Prophylactic effects of lidocaine or beclomethasone spray on post-operative sore throat and cough after orotracheal intubation[J]. Iran J Otorhinolaryngol, 2015, 27: 179-184. |
| [6] |
GEMECHU B M, GEBREMEDHN E G, MELKIE T B. Risk factors for postoperative throat pain after general anaesthesia with endotracheal intubation at the University of Gondar Teaching Hospital, Northwest Ethiopia, 2014[J/OL]. Pan Afr Med J, 2017, 27: 127. DOI: 10.11604/pamj.2017.27.127.10566.
|
| [7] |
ATKINSON C J, RANGASAMI J. Uvula necrosis—an unusual cause of severe postoperative sore throat[J]. Br J Anaesth, 2006, 97: 426-427. |
| [8] |
NATH P, WILLIAMS S, HERRERA MÉNDEZ L F, MASSICOTTE N, GIRARD F, RUEL M. Alkalinized lidocaine preloaded endotracheal tube cuffs reduce emergence cough after brief surgery: a prospective randomized trial[J]. Anesth Analg, 2018, 126: 615-620. DOI:10.1213/ANE.0000000000002647 |
| [9] |
LAM F, LIN Y C, TSAI H C, CHEN T L, TAM K W, CHEN C Y. Effect of intracuff lidocaine on postoperative sore throat and the emergence phenomenon: a systematic review and meta-analysis of randomized controlled trials[J/OL]. PLoS One, 2015, 10: e0136184. DOI: 10.1371/journal.pone.0136184.
|
| [10] |
GENG G, HU J, HUANG S. The effect of endotracheal tube cuff pressure change during gynecological laparoscopic surgery on postoperative sore throat: a control study[J]. J Clin Monit Comput, 2015, 29: 141-144. DOI:10.1007/s10877-014-9578-2 |
| [11] |
NEELAKANTA G, MILLER J. Minimum alveolar concentration of isoflurane for tracheal extubation in deeply anesthetized children[J]. Anesthesiology, 1994, 80: 811-813. DOI:10.1097/00000542-199404000-00013 |
| [12] |
KIM H Y, KIM J Y, AHN S H, LEE S Y, PARK H Y, KWAK H J. Predicting effective remifentanil concentration in 95% of patients to prevent emergence cough after laryngomicroscopic surgery[J/OL]. Medicine (Baltimore), 2018, 97: e11258. DOI: 10.1097/MD.0000000000011258.
|
| [13] |
CRERAR C, WELDON E, SALAZAR J, GANN K, KELLY J A, PELLEGRINI J E. Comparison of 2 laryngeal tracheal anesthesia techniques in reducing emergence phenomena[J]. AANA J, 2008, 76: 425-431. |
| [14] |
SOARES S M, ARANTES V M, MÓDOLO M P, DOS SANTOS V J, VANE L A, NAVARRO E LIMA L H, et al. The effects of tracheal tube cuffs filled with air, saline or alkalinised lidocaine on haemodynamic changes and laryngotracheal morbidity in children: a randomised, controlled trial[J]. Anaesthesia, 2017, 72: 496-503. DOI:10.1111/anae.13764 |
| [15] |
KESICI S, DEMIRCI M, KESICI U. Antibacterial effects of lidocaine and adrenaline[J]. Int Wound J, 2019, 16: 1190-1194. DOI:10.1111/iwj.13182 |
| [16] |
WEIBEL S, JOKINEN J, PACE N L, SCHNABEL A, HOLLMANN M W, HAHNENKAMP K, et al. Efficacy and safety of intravenous lidocaine for postoperative analgesia and recovery after surgery: a systematic review with trial sequential analysis[J]. Br J Anaesth, 2016, 116: 770-783. DOI:10.1093/bja/aew101 |
| [17] |
LEE H M, CHOI K W, BYON H J, LEE J M, LEE J R. Systemic lidocaine infusion for post-operative analgesia in children undergoing laparoscopic inguinal hernia repair: a randomized double-blind controlled trial[J/OL]. J Clin Med, 2019, 8: 2014. DOI: 10.3390/jcm8112014.
|
| [18] |
HU S H, LI Y H, WANG S B, XU S Q, JU X, MA L. Effects of intravenous infusion of lidocaine and dexmedetomidine on inhibiting cough during the tracheal extubation period after thyroid surgery[J/OL]. BMC Anesthesiol, 2019, 19: 66. DOI: 10.1186/s12871-019-0739-1.
|
| [19] |
GAUR P, UBALE P, KHADANGA P. Efficacy and safety of using air versus alkalinized 2% lignocaine for inflating endotracheal tube cuff and its pressure effects on incidence of postoperative coughing and sore throat[J]. Anesth Essays Res, 2017, 11: 1057-1063. DOI:10.4103/aer.AER_85_17 |
 2021, Vol. 42
2021, Vol. 42


