异位妊娠的治疗分为保守治疗(观察及药物治疗)和手术治疗。随着超声技术的发展及血清人绒毛膜促性腺激素(human chorionic gonadotropin,hCG)检查的普及,近年来异位妊娠在妊娠较早期即可诊断,提高了保守治疗成功率,减少了手术及麻醉的风险。甲氨蝶呤(methotrexate,MTX)是保守治疗异位妊娠的首选药物,单次肌内注射效果较好,且不良反应发生率低。一项meta分析显示,MTX单次注射治疗异位妊娠的成功率可达88.1%[1]。治疗前的初始血清β-hCG水平是临床医师选择治疗方案的重要依据,有研究发现治疗前hCG水平在2 000~5 000 mIU/mL范围内者MTX单次注射治疗的成功率高[2-4]。然而,药物保守治疗随访周期较长,血清hCG预测保守治疗疗效的阈值尚无统一标准。本研究回顾性分析了2010年1月1日至2018年12月31日于我院接受MTX单次注射治疗的96例异位妊娠患者资料,评估治疗后血清β-hCG水平变化对疗效的预测价值,现报告如下。
1 资料和方法 1.1 病例资料回顾性纳入2010年1月1日至2018年12月31日于我院接受MTX单次注射治疗的96例异位妊娠患者资料。异位妊娠诊断标准:(1)超声下见附件区包块;(2)血清β-hCG>2 000 mIU/mL时阴道超声未发现宫内妊娠囊。纳入研究的96例异位妊娠女性年龄为20~45岁,平均(30.0±6.7)岁。治疗前血清β-hCG水平为47~5 052 mIU/mL,中位数(下四分位数,上四分位数)为452(229,904)mIU/mL。其中84例(87.5%)患者入院前阴道超声可见附件区包块,长径为6~63 mm,平均(22.0±11.0)mm;其余12例(12.5%)患者入院前阴道超声下未见明确附件区包块,但有明显的腹痛及血清β-hCG进行性上升,入院后复查超声可见附件区包块。
1.2 MTX治疗指征(1) 无腹腔活动性出血;(2)血清β-hCG<5 000 mIU/mL;(3)超声下未见宫外心管搏动;(4)宫外包块长径<40 mm;(5)肝功能正常;(6)无MTX过敏史;(7)血流动力学稳定;(8)充分知情同意。92例患者符合保守治疗指征,4例附件区包块长径>40 mm及1例治疗前血清β-hCG>5 000 mIU/mL者被充分告知病情及治疗风险后签字要求先行药物保守治疗。
1.3 治疗方法患者均采用MTX 50 mg/m2单次肌内注射方案,治疗期间减少活动,保持大便通畅,禁止性生活。保守治疗过程中观察并记录患者的血压、脉搏,观察腹痛及阴道流血情况,定期检测血清β-hCG水平。
1.4 MTX单次注射治疗成功标准及分组患者诊断为异位妊娠后即接受MTX单次注射治疗,接受MTX单次注射治疗后随访β-hCG降至正常2次且未再接受第2次MTX治疗或手术治疗者判断为治疗成功。根据治疗结局分为治疗成功组和治疗失败组,比较2组治疗前血清β-hCG水平。根据治疗前血清β-hCG水平分为<1 000、1 000~1 999、2 000~2 999、≥3 000 mIU/mL组,比较各组间MTX单次注射治疗成功率。
1.5 统计学处理采用SPSS 12.0软件进行统计学分析。呈正态分布的计量资料以x±s表示,两组间比较采用独立样本t检验;不满足正态分布的计量资料以中位数(下四分位数,上四分位数)表示,组间比较采用Mann-Whitney U检验。计数资料以例数和百分数表示,组间比较采用χ2检验或Fisher确切概率法。通过ROC曲线评估β-hCG水平对MTX单次注射治疗结局的预测价值。检验水准(α)为0.05。
2 结果 2.1 治疗成功组与失败组一般资料及治疗前血清β-hCG水平比较96例异位妊娠患者中,57例(59.4%)经MTX单次注射治疗成功,39例(40.6%)失败。由表 1可见,治疗成功组及失败组年龄、停经时间、治疗前附件区包块长径差异均无统计学意义(P均>0.05),但治疗成功组治疗前血清β-hCG水平低于失败组,差异有统计学意义(P=0.007)。96例患者中,32例(33.3%)治疗后4 d血清β-hCG水平较治疗前上升,其中10例(10.4%)血清β-hCG水平上升>50%。57例治疗成功组患者中,9例(15.8%)治疗后4 d血清β-hCG较治疗前上升,其中1例(1.8%)血清β-hCG上升>50%;29例(50.9%)治疗后4 d血清β-hCG水平较治疗前下降≥20%。39例治疗失败组患者中,3例患者在接受MTX单次注射治疗后4 d内出现手术指征并接受手术治疗;余36例患者MTX单次注射治疗后复查超声提示包块增大且β-hCG下降不明显或上升,告知病情后患者要求手术。此36例患者中,23例(63.9%)治疗后4 d血清β-hCG较治疗前上升,其中9例(25.0%)血清β-hCG上升>50%;6例(16.7%)治疗后4 d血清β-hCG水平较治疗前下降≥20%。
|
|
表 1 MTX单次注射治疗成功组及失败组异位妊娠患者一般资料及治疗前血清β-hCG水平比较 Tab 1 Comparison of general information and serum β-hCG levels before treatment between treatment success and failure groups of ectopic pregnancy patients |
2.2 按治疗前血清β-hCG水平分组的患者治疗结局
根据治疗前血清β-hCG水平进行分组,β-hCG<1 000 mIU/mL组治疗成功率最高(66.2%,49/74),随着治疗前β-hCG水平上升,治疗成功率下降,β-hCG≥3 000 mIU/mL组治疗均失败(表 2)。统计学分析表明,当治疗前血清β-hCG<3 000 mIU/mL时(β-hCG≥3 000 mIU/mL组仅2例,未纳入分析),各亚组的治疗成功率差异并无统计学意义(P>0.05)。
|
|
表 2 按治疗前血清β-hCG水平分组的患者MTX单次注射治疗结局 Tab 2 Outcome of MTX single-dose injection in subgroups with different serum β-hCG levels before treatment |
2.3 血清β-hCG预测MTX单次注射治疗结局的价值
ROC曲线分析结果(图 1)显示,治疗后4 d血清β-hCG预测MTX单次注射治疗结局的AUC为0.80(95% CI 0.70~0.88,P<0.001),阈值为650 mIU/mL,灵敏度为91.2%,特异度为66.7%,阳性预测值为81.2%,阴性预测值为82.8%;治疗后7 d血清β-hCG预测MTX单次注射治疗结局的AUC为0.71(95% CI 0.58~0.82,P<0.001),阈值为103 mIU/mL,灵敏度为42.9%,特异度为100.0%,阳性预测值为100.0%,阴性预测值为16.7%。
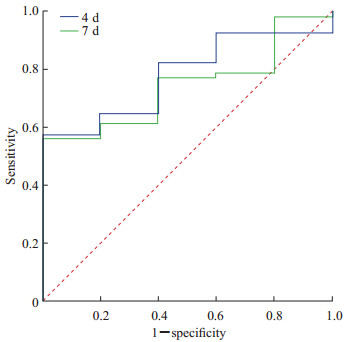
|
图 1 治疗后4、7 d血清β-hCG预测MTX单次注射治疗结局的ROC曲线 Fig 1 ROC curves of serum β-hCG 4 d and 7 d after treatment in predicting outcome of single-dose injection of MTX β-hCG: β-human chorionic gonadotropin; MTX: Methotrexate; ROC: Receiver operating characteristic. |
以ROC曲线得出的治疗后4 d和7 d血清β-hCG阈值作为依据分组后进行预后比较,结果(表 3)显示治疗后4 d血清β-hCG≤650 mIU/mL组的治疗成功率较>650 mIU/mL组高,差异有统计学意义(χ2=34.464,P<0.001);治疗后7 d血清β-hCG≤103 mIU/mL组与>103 mIU/mL组治疗成功率差异无统计学意义(P=0.146)。
|
|
表 3 根据治疗后4 d和7 d血清β-hCG阈值分组后MTX单次注射治疗结局比较 Tab 3 Comparison of outcome of MTX single-dose injection between groups divided by cut-off value of serum β-hCG 4 d and 7 d after treatment |
3 讨论
MTX治疗异位妊娠由Tanaka等[5]首次报道,随后因不良反应发生率低、对卵巢功能影响较小而被广泛应用于临床。既往研究显示血清β-hCG>5 000 mIU/mL、宫外有心管搏动、病灶直径>40 mm者易出现MTX治疗失败[6]。MTX治疗过程中,临床上通过监测治疗后4、7、14 d的血清β-hCG水平评估治疗效果,之后可每周1次直至降至正常。但目前为止,对于预测MTX单次注射治疗失败的治疗后4 d血清hCG阈值没有统一的标准。
既往已有文献报道预测MTX治疗失败的初始hCG阈值为2 000~5 000 mIU/mL[4, 7-8],最新美国异位妊娠治疗指南推荐MTX的治疗适用于β-hCG水平较低的患者及β-hCG水平处于不再进行性上升的平台期患者[9]。因此,本研究纳入的病例中仅有2例患者治疗前β-hCG≥3 000 mIU/mL,且用药前已充分告知患者保守治疗相关风险。本研究中MTX单次注射治疗成功率为59.4%(57/96),低于既往文献报道成功率(65%~100%)[10-12]。治疗失败组39例患者中9例(23.1%)治疗后4 d血清β-hCG较治疗前上升>50%,低于Mashiach等[13]的研究结果(69%)。由于治疗过程中出现的腹痛症状和腔镜手术的普及,部分患者在治疗期间出现腹痛加重或β-hCG下降不明显时会要求行手术治疗,这可能是本研究MTX单次注射治疗成功率和治疗失败组治疗后4 d β-hCG较治疗前上升>50%的患者比例较低的原因。
Brady等[14]在体外受精人群中的研究结果发现,MTX单次注射治疗成功组与失败组阴道超声提示的附件区包块长径存在差异。但本研究中两组附件区包块长径差异无统计学意义,与Helmy等[15]的研究结果一致。这可能与研究样本量较小有关。另外,接受体外受精的受孕人群经历促排卵、取卵过程,可能因卵巢组织受损、修复而存在炎性及非炎性增大,造成超声测量误差。
2007年,Agostini等[16]提出hCG指数的概念,hCG指数计算公式为(治疗后4 d hCG水平-治疗前hCG水平)/治疗前hCG水平,hCG指数的阈值为0.2时可较好地预测MTX单次注射治疗结局。Levin等[17]的回顾性研究中建议将治疗后4 d血清hCG较治疗后1 d下降≥22%作为预测MTX单次注射治疗成功的阈值。本研究MTX单次注射治疗成功组中有29例(50.9%)患者治疗后4 d血清β-hCG水平较治疗前下降≥20%,失败组中(剔除3例于治疗后4 d内接受手术的患者)仅有6例(16.7%)治疗后4 d血清β-hCG水平较治疗前下降≥20%。因此,本研究结果也支持0.2可作为hCG指数阈值预测MTX单次注射治疗结局。
有学者认为随访过程中可以不监测治疗后4 d hCG水平,而是将治疗后7 d hCG下降>50%单独作为MTX单次注射治疗成功的预测指标[18]。但由于异位妊娠病灶破裂出血易危及生命,且考虑经济成本效益,我们依然建议监测治疗后4 d和7 d hCG水平。本研究中经ROC曲线得出预测MTX单次注射治疗结局的治疗后4 d和7 d血清β-hCG阈值分别为650 mIU/mL和103 mIU/mL,且以治疗后4 d血清β-hCG阈值分组后两组的治疗成功率差异有统计学意义,而以治疗后7 d血清β-hCG阈值分组后两组的治疗成功率差异并无统计学意义,因此,我们认为治疗后4 d血清β-hCG≤650 mIU/mL作为预测MTX单次注射治疗成功的临床意义更大。
综上所述,MTX单次注射治疗后4 d及7 d的血清β-hCG变化及hCG指数有助于预测治疗效果,为后续治疗随访方案的选择提供参考,并且治疗后4 d的血清β-hCG较7 d β-hCG可能在临床实际工作中更有指导意义。但本研究样本量较小,个别患者的治疗方案受患者意愿等因素影响,存在一定的选择性偏倚,今后仍需要开展大样本的研究进一步证实。
| [1] |
BACHMAN E A, BARNHART K. Medical management of ectopic pregnancy: a comparison of regimens[J]. Clin Obstet Gynecol, 2012, 55: 440-447. DOI:10.1097/GRF.0b013e3182510a73 |
| [2] |
USTUNYURT E, DURAN M, COSKUN E, USTUNYURT Ö B, SIMŞEK H. Role of initial and day 4 human chorionic gonadotropin levels in predicting the outcome of single-dose methotrexate treatment in women with tubal ectopic pregnancy[J]. Arch Gynecol Obstet, 2013, 288: 1149-1152. DOI:10.1007/s00404-013-2879-8 |
| [3] |
TAWFIQ A, AGAMEYA A F, CLAMAN P. Predictors of treatment failure for ectopic pregnancy treated with single-dose methotrexate[J]. Fertil Steril, 2000, 74: 877-880. DOI:10.1016/S0015-0282(00)01547-8 |
| [4] |
MENON S, COLINS J, BARNHART K T. Establishing a human chorionic gonadotropin cutoff to guide methotrexate treatment of ectopic pregnancy: a systematic review[J]. Fertil Steril, 2007, 87: 481-484. DOI:10.1016/j.fertnstert.2006.10.007 |
| [5] |
TANAKA T, HAYASHI H, KUTSUZAWA T, FUJIMOTO S, ICHINOE K. Treatment of interstitial ectopic pregnancy with methotrexate: report of a successful case[J]. Fertil Steril, 1982, 37: 851-852. DOI:10.1016/S0015-0282(16)46349-1 |
| [6] |
Practice Committee of American Society for Reproductive Medicine. Medical treatment of ectopic pregnancy[J]. Fertil Steril, 2008, 90(5 Suppl): S206-S212. |
| [7] |
BARNHART K T, GOSMAN G, ASHBY R, SAMMEL M. The medical management of ectopic pregnancy: a meta-analysis comparing "single dose" and "multidose" regimens[J]. Obstet Gynecol, 2003, 101: 778-784. |
| [8] |
HELMY S, BADER Y, PABLIK E, TIRINGER D, PILS S, LAML T, et al. Cut-off value of initial serum β-hCG level predicting a successful MTX therapy in tubal ectopic pregnancy: a retrospective cohort study[J]. Eur J Obstet Gynecol Reprod Biol, 2014, 179: 175-180. DOI:10.1016/j.ejogrb.2014.05.033 |
| [9] |
American College of Obstetricians and Gynecologists' Committee on Practice Bulletins-Gynecology. ACOG Practice Bulletin No. 193: Tubal Ectopic Pregnancy[J/OL]. Obstet Gynecol, 2018, 131: e91-e103. DOI: 10.1097/AOG.0000000000002560.
|
| [10] |
ERDEM M, ERDEM A, ARSLAN M, OÇ A, BIBEROĞLU K, GÜRSOY R. Single-dose methotrexate for the treatment of unruptured ectopic pregnancy[J]. Arch Gynecol Obstet, 2004, 270: 201-204. DOI:10.1007/s00404-003-0543-4 |
| [11] |
NGUYEN Q, KAPITZ M, DOWNES K, SILVA C. Are early human chorionic gonadotropin levels after methotrexate therapy a predictor of response in ectopic pregnancy?[J/OL]. Am J Obstet Gynecol, 2010, 202: 630. e1-5. DOI: 10.1016/j.ajog.2010.03.022.
|
| [12] |
BIXBY S, TELLO R, KULIGOWSKA E. Presence of a yolk sac on transvaginal sonography is the most reliable predictor of single-dose methotrexate treatment failure in ectopic pregnancy[J]. J Ultrasound Med, 2005, 24: 591-598. DOI:10.7863/jum.2005.24.5.591 |
| [13] |
MASHIACH R, KISLEV I, GILBOA D, MAZAKI-TOVI S, SEIDMAN D S, GOLDENBERG M, et al. Significant increase in serum hCG levels following methotrexate therapy is associated with lower treatment success rates in ectopic pregnancy patients[J]. Eur J Obstet Gynecol Reprod Biol, 2018, 231: 188-191. DOI:10.1016/j.ejogrb.2018.10.046 |
| [14] |
BRADY P C, MISSMER S A, FARLAND L V, GINSBURG E S. Clinical predictors of failing one dose of methotrexate for ectopic pregnancy after in vitro fertilization[J]. J Assist Reprod Genet, 2017, 34: 349-356. DOI:10.1007/s10815-016-0861-7 |
| [15] |
HELMY S, KOCH M, KÖLBL H, GROHMANN-IZAY B, SOLOMAYER E, BADER Y. Correlation of the volume of ectopic pregnancy and MTX therapy outcome: a retrospective cohort study[J]. Eur J Obstet Gynecol Reprod Biol, 2015, 184: 108-111. DOI:10.1016/j.ejogrb.2014.09.038 |
| [16] |
AGOSTINI A, BLANC K, RONDA I, ROMAIN F, CAPELLE M, BLANC B. Prognostic value of human chorionic gonadotropin changes after methotrexate injection for ectopic pregnancy[J]. Fertil Steril, 2007, 88: 504-506. DOI:10.1016/j.fertnstert.2006.11.138 |
| [17] |
LEVIN G, DIOR U, SHUSHAN A, GILAD R, BENSHUSHAN A, ROTTENSTREICH A. Early prediction of the success of methotrexate treatment success by 24-hour pretreatment increment in hCG and day 1-4 change in hCG[J]. Reprod Biomed Online, 2019, 39: 149-154. DOI:10.1016/j.rbmo.2019.02.005 |
| [18] |
THURMAN A R, CORNELIUS M, KORTE J E, FYLSTRA D L. An alternative monitoring protocol for single-dose methotrexate therapy in ectopic pregnancy[J/OL]. Am J Obstet Gynecol, 2010, 202: 139. e1-6. DOI: 10.1016/j.ajog.2009.09.031.
|
 2021, Vol. 42
2021, Vol. 42


