2. 上海交通大学医学院附属仁济医院脊柱外科, 上海 200120
2. Department of Spinal Surgery, Renji Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai 200120, China
急性外伤性硬脑膜外血肿(acute traumatic epidural hematoma,ATEDH)是一种常见的神经外科急症,占外伤性颅内血肿的30%,在创伤性颅脑损伤患者中其发生率为1%~2%,有较高的致死、致残率[1]。绝大多数ATEDH与颅骨骨折有关,骨折导致的位于骨沟的脑膜中动脉(middle meningeal artery,MMA)或静脉窦活动性出血,以及骨折线累及的板障出血都会导致ATEDH形成和进展,其中颅骨骨折引起的MMA撕裂最常见[2]。如果ATEDH无明显的占位效应,可以保守治疗并密切观察,但是有5.5%~65%的患者在保守治疗过程中出现血肿体积急性增大[3]。对于进展形成占位效应的ATEDH,传统治疗方法以全身麻醉下开颅血肿清除术为主,该术式疗效较好,但创伤较严重,患者可能发生麻醉意外、出血、感染等并发症[4]。脑血管造影后介入栓塞可用于治疗ATEDH,不仅可以避免侵入性手术的一系列并发症,还能有效降低血肿体积急性增大的风险[5-6]。在MMA栓塞术消除血肿进展或再出血的风险后,可根据血肿体积行保守治疗或选择性在局部麻醉下进行有或无尿激酶注入的钻孔引流手术[7-8]。本研究回顾性分析2010年1月至2020年1月在海军军医大学(第二军医大学)长海医院脑血管病中心接受MMA栓塞治疗的40例ATEDH患者资料,总结ATEDH的MMA栓塞治疗经验。
1 资料和方法 1.1 病例资料研究对象为2010年1月至2020年1月在海军军医大学(第二军医大学)长海医院脑血管病中心住院接受MMA栓塞治疗的ATEDH患者。纳入标准:(1)年龄≥18岁;(2)既往改良Rankin量表(modified Rankin scale,mRS)评分≤2分;(3)有明确头部外伤病史,且发病至到达急诊时间≤24 h;(4)术前格拉斯哥昏迷量表(Glasgow coma scale,GCS)评分>8分;(5)CT检查示血肿位于颞部、额颞部、颞顶部,中线移位≤15 mm。排除标准:(1)脑疝;(2)双侧急性硬脑膜外血肿;(3)CT检查示存在需要手术干预的硬脑膜下血肿或脑内血肿;(4)因疾病或药物导致的凝血功能异常;(5)存在脑血管介入治疗禁忌证(碘化造影剂过敏、肾功能不全等);(6)CT或既往MRI检查提示颅内占位性病变。
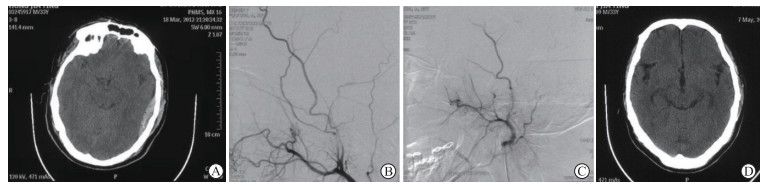
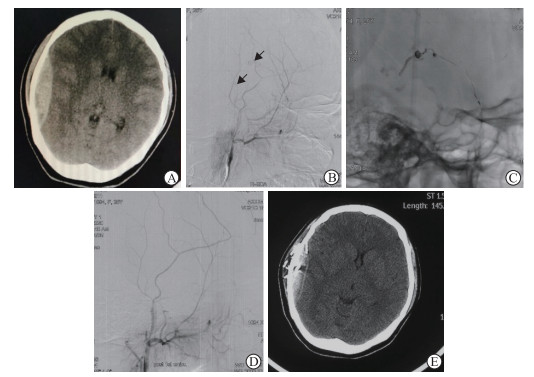
1.2 治疗与随访所有患者急诊入院后完善头颅CT平扫检查,然后在发病24 h内于局部麻醉下行数字减影血管造影(digital subtraction angiography,DSA)+MMA栓塞术。先于右侧腹股沟处置入股动脉鞘,再置入6 F导引导管至病变侧的颈外动脉。在进行脑血管造影后,用微导管对病变侧的MMA进行超选择性血管造影,并尽可能使微导管在MMA中深入,到达明显可识别的造影剂外渗、假性动脉瘤或可见的动脉撕裂处前停止。之后以明胶海绵颗粒(图 1)或液体栓塞材料如Onyx-18胶(图 2)对MMA进行栓塞,直至造影剂外渗停止,或MMA远端主干不显影,或观察到微导管反流。在撤除微导管后,通过导引导管进行脑血管造影复查,所有病变血管结构均不显影后结束手术。
|
图 1 1例左侧急性外伤性硬脑膜外血肿患者明胶海绵颗粒栓塞MMA前后的影像学表现 Fig 1 Imaging findings of a patient with left acute traumatic epidural hematoma before and after MMA embolization with gelatin sponge particles Male, 33 years old, 3 h after falling, diagnosed as having acute epidural hematoma on the left, conscious at admission, GCS scored 15. A: CT examination at admission showed a fusiform high-density shadow in the left temporal region; B: DSA showed the MMA bleeding lesion; C: DSA showed the bleeding stopped after MMA embolization with gelfoam; D: CT examination showed the hematoma completely disappeared 6 months after operation. MMA: Middle meningeal artery; GCS: Glasgow coma scale; CT: Computed tomography; DSA: Digital subtraction angiography. |
|
图 2 1例右侧急性外伤性硬脑膜外血肿患者Onyx-18胶栓塞MMA前后的影像学表现 Fig 2 Imaging findings of a patient with right acute traumatic epidural hematoma before and after MMA embolization with Onyx-18 glue Female, 26 years old, 3 h after accident, diagnosed as having acute epidural hematoma on the right, somnolence at admission, GCS scored 14. A: CT examination showed a fusiform high-density shadow in the right temporal region; B: DSA showed contrast agent extravasation (arrows) in the MMA; C: The MMA was embolized with Onyx-18 glue; D: DSA showed that the bleeding stopped after MMA embolization; E: CT examination showed the hematoma was absorbed 1 month after operation. MMA: Middle meningeal artery; GCS: Glasgow coma scale; CT: Computed tomography; DSA: Digital subtraction angiography. |
介入栓塞术后,若患者GCS评分无降低,无局部神经压迫症状,复查头颅CT提示最大血肿面积层面上的血肿厚度≤10 mm,并根据多田公式[9]计算得血肿体积≤10 mL,予药物保守治疗,并严密观察;若患者在行介入栓塞术后,硬脑膜外血肿仍有明显占位效应,血肿体积>10 mL或血肿厚度>10 mm,予局部麻醉下钻孔引流结合注射尿激酶溶解血凝块,消除占位效应;若患者病情进展,颅内血肿增大,则急诊行开颅血肿清除术。
随访至术后6个月。随访时复查头颅CT,并记录患者扩展的格拉斯哥结局量表(Glasgow outcome scale-extended,GOSE)评分,以及与手术相关的感染、缺血性脑卒中、神经功能障碍等并发症的发生情况。
1.3 统计学处理应用SPSS 22.0软件进行数据处理,计量资料以x±s表示,计数资料以例数表示。
2 结果入组ATEDH患者共40例,男21例、女19例;年龄为16~68岁,平均年龄为(38.4±4.6)岁。入院时GCS评分为13~15分者25例,9~12分者15例,主要临床症状为头痛和呕吐。入院时急诊行头颅CT检查示硬脑膜外血肿位于额颞部18例,位于颞顶部8例,单纯位于颞部14例。利用头颅CT平扫图像,根据多田公式计算得到的血肿体积为4~28 mL,平均体积为(21.1±5.6)mL;中线移位<10 mm的患者26例,中线移位10~15 mm的患者14例。
40例ATEDH患者DSA检查均见MMA存在假性动脉瘤或造影剂外渗,即MMA为出血源,在介入栓塞MMA后出血立即停止,且无并发症发生。8例患者为单纯MMA栓塞治疗,术前血肿平均体积为(9.6±5.2)mL。32例患者MMA栓塞术后行钻孔引流,术前血肿平均体积为(23.2±5.1)mL。无患者因病情进展接受开颅血肿清除术。
出院时40例ATEDH患者的GCS评分均为15分,硬脑膜外血肿相关临床症状(如头痛、恶心、呕吐等)与入院时相比均明显好转。术后6个月随访时,40例患者CT检查均未见血肿进展或复发,GOSE评分均为8分。术后随访过程中,40例患者均未发生手术相关的感染、缺血性脑卒中、神经功能障碍等并发症。
3 讨论ATEDH是一种有高致死、致残率的神经外科急症,传统药物保守治疗往往伴随血肿进展,造成占位效应。开颅血肿清除术作为一种传统治疗方式,适用于神经功能缺损症状明显、血肿体积>30 mL、血肿厚度>15 mm的患者,尤其是对于伴脑疝的ATEDH患者,可以有效解除血肿占位效应,并且能在直视下处理活动性出血点,有效预防患者死亡和发生神经功能障碍。但是传统的开颅血肿清除术存在麻醉和手术操作时间长、术中出血量大等不足,尤其是对于体弱者创伤更严重,手术适应范围较小。
研究指出,可以用局部麻醉下颅骨钻孔引流术联合注射尿激酶治疗ATEDH,钻孔引流术具备出血少、创伤小、术后恢复快等优点,尤其适用于高龄或不能耐受全身麻醉手术的患者[7-8]。钻孔引流术虽然可以在创伤较小的条件下解除血肿的占位效应,但是并不能有效预防血肿进展和再出血,所以钻孔引流术并不适合血肿不稳定的患者。
在ATEDH中,最常见的原因是MMA损伤引起的动脉性出血。研究报道,急诊行DSA和MMA栓塞可及时发现ATEDH患者的出血点并止血,能有效避免患者接受进一步的开颅血肿清除手术。因此,对于ATEDH患者早期进行介入栓塞治疗可以有效止血,消除血肿进展风险,必要时再进行注射尿激酶的钻孔引流术以充分解除血肿的占位效应。从理论上讲,这是一种安全、有效的ATEDH治疗方法,本组病例资料也证实了这一点。本组40例ATEDH均累及颞部,包括额颞部、颞顶部、单纯颞部,术前头颅CT检查提示45%(18/40)的患者硬脑膜外血肿位于额颞部。术中DSA见MMA存在假性动脉瘤结构或造影剂外渗,证明MMA损伤是ATEDH的主要出血原因。40例患者均在MMA栓塞后出血停止,术后6个月复查均未见血肿进展或复发。
患者接受MMA栓塞术后硬脑膜外血肿一般需要4~12周[1]才能自行吸收,在此期间,体积较大的血肿存在占位效应,在进行介入栓塞治疗后,如有必要可行钻孔引流术并注射尿激酶解除占位效应。本研究中,32例患者在MMA栓塞术后接受局部麻醉下钻孔引流术,术后6个月复查患者均未出现血肿复发和手术并发症。
综上所述,对于MMA出血导致的ATEDH,早期进行MMA栓塞可以防止持续出血导致的血肿增大,能有效避免患者进一步接受创伤较大的外科侵入性治疗,并且具有较好的有效性和安全性。
| [1] |
WINN H R, YOUMANS J R. Youmans neurological surgery[M]. Philadelphia, PA: Saunders, 2004: 52935294.
|
| [2] |
KIM D H, LEE J Y, JEON H J, CHO B M, PARK S H, OH S M. Intraoperative endovascular embolization of middle meningeal artery and a pseudoaneurysm by using N-butyl 2-cyanoacrylate for hemostasis during operation of acute epidural hemorrhage[J]. Korean J Neurotrauma, 2015, 11: 167-169. DOI:10.13004/kjnt.2015.11.2.167 |
| [3] |
LAMMY S, MCCONNELL R, KAMEL M, RENNIE I, AL-HADDAD S. Extradural haemorrhage: is there a role for endovascular treatment?[J]. Br J Neurosurg, 2013, 27: 383-385. DOI:10.3109/02688697.2012.717981 |
| [4] |
ROSS I B. Embolization of the middle meningeal artery for the treatment of epidural hematoma[J]. J Neurosurg, 2009, 110: 1247-1249. DOI:10.3171/2008.7.JNS0883 |
| [5] |
SIRH S, PARK H R, PARK S Q. Usefulness of middle meningeal embolization to prevent recurrent spontaneous chronic subdural hemorrhage[J]. J Cerebrovasc Endovasc Neurosurg, 2018, 20: 40-46. DOI:10.7461/jcen.2018.20.1.40 |
| [6] |
ZUSSMAN B M, GOLDSCHMIDT E, FARAJI A H, SALVETTI D J, JANKOWITZ B T. Middle meningeal artery embolization for the treatment of an expanding epidural hematoma[J]. World Neurosurg, 2019, 128: 284-286. DOI:10.1016/j.wneu.2019.05.084 |
| [7] |
LIU J T, TYAN Y S, LEE Y K, WANG J T. Emergency management of epidural haematoma through burr hole evacuation and drainage. a preliminary report[J]. Acta Neurochir (Wien), 2006, 148: 313-317. DOI:10.1007/s00701-005-0723-z |
| [8] |
LIU W, MA L, WEN L, SHEN F, SHENG H, ZHOU B, et al. Drilling skull plus injection of urokinase in the treatment of epidural haematoma: a preliminary study[J]. Brain Inj, 2008, 22: 199-204. DOI:10.1080/02699050801895407 |
| [9] |
闫乐卡, 刘怀军, 李剑颖, 曹会志, 闫春明, 冯平勇, 等. CT血肿体积测量软件与多田公式对比及应用[J]. 河北医药, 2010, 32: 2149-2150. DOI:10.3969/j.issn.1002-7386.2010.16.001 |
 2021, Vol. 42
2021, Vol. 42


