自2020年12月新型冠状病毒肺炎(coronavirus disease 2019, COVID-19)疫情暴发以来, 我国公共卫生安全受到严重威胁[1]。其病原体严重急性呼吸综合征冠状病毒2(severe acute respiratory syndrome coronavirus 2, SARS-CoV-2)易侵犯人体肺组织引起肺部损害, 部分病例病情进展迅速, 可由轻型及普通型快速发展为重型及危重型, 并出现低氧血症、急性呼吸窘迫综合征(acute respiratory distress syndrome, ARDS)及多器官功能障碍综合征(multiple organ dysfunction syndrome, MODS), 严重威胁患者生命[1-2], 因此重型及危重型COVID-19病例的救治是降低病死率的关键。随着我国COVID-19疫情防治策略的有效实施, 轻型及普通型患者均能得到很好的治愈, 但重型及危重型患者的临床救治仍是医务人员面临的重点及难点问题。本研究分析在我院治愈出院与未治愈(包括死亡)重型及危重型COVID-19患者的临床及胸部CT资料, 并基于CT影像定量技术评估肺部病灶的变化特点, 为重型及危重型COVID-19病例的救治提供经验。
1 资料和方法 1.1 临床资料收集2020年1月23日至2020年3月5日上海市公共卫生临床中心(上海市COVID-19定点收治医院)收治的25例重型及危重型COVID-19病例资料。COVID-19诊断标准及重型、危重型COVID-19患者出院标准参照《新型冠状病毒肺炎诊疗方案(试行第六版)》[1], 其中诊断时间节点为研究结束时(2020年3月5日)的回顾性诊断。本研究中进展期指轻型或普通型转为重型或危重型至重型或危重型转为轻型或普通型的时间段;恢复期指重型或危重型转为轻型或普通型至治愈出院的时间段。25例患者整体临床特征中实验室检查数据所取时间节点为进展早期, 即患者由轻型或普通型转为重型或危重型时的数据(如果患者入院时即为重型或危重型, 则取入院时基线数据), 治愈出院患者中恢复期数据选取重型或危重型转为轻型或普通型时的数据。
1.2 胸部CT检查及影像学分析方法CT检查采用64排多层螺旋CT仪(型号:Scenaria, 日本Hitachi公司), 扫描参数:管电压120 kV, 自动毫安(180~400 mA), 层厚5 mm, 准直0.625 mm, 螺距1.5;扫描范围取胸廓入口至肺底。标准肺窗:窗位600 HU, 窗宽1 200 HU;纵隔窗:窗位40 HU, 窗宽350 HU。分析胸部CT影像基本表现, 同时采用基于CT影像的智能化肺炎病灶定量分析软件(依图医疗, 版本5.4-WUHAN-VIRUS-v4)定量评估肺部病灶(包括磨玻璃影及实变影)体积占全肺体积的百分比。
1.3 统计学处理应用Stata/SE 10.1软件进行统计学分析。呈正态分布的计量资料以x±s表示, 两组间比较采用独立样本t检验;呈偏态分布的计量资料以中位数(下四分位数, 上四分位数)表示, 两组间比较采用Wilcoxon秩和检验;治愈出院患者进展期与恢复期数据的比较采用配对t检验或配对符号秩检验;不同时期CT定量病灶体积百分比数据的比较采用t检验。计数资料以例数和百分数表示, 组间比较采用Fisher确切概率法。采用多因素logistic回归分析重型或危重型患者治愈出院的影响因素。检验水准(α)为0.05。
2 结果 2.1 患者临床资料分析25例(包括3例死亡)患者中男19例、女6例, 年龄为65(63, 75)岁, BMI为25.60(23.51, 28.65)kg/m2, 发病至进展为重型或危重型的时间为10.0(5.5, 13.5)d。9例患者有武汉地区居住史, 5例武汉地区旅行史, 7例有确诊病例接触史, 1例欧洲旅行史, 3例无明确流行病学史。首发症状以发热(22例)、咳嗽(14例)最常见, 其他症状包括咳痰、胸闷气促、乏力纳差、恶心呕吐、肌肉酸痛等。18例患者合并基础疾病, 包括高血压(10例)、冠心病(5例)、心律失常(4例)、缺血性脑卒中(1例)、糖尿病(5例)、慢性阻塞性肺疾病(1例)、慢性病毒性肝炎(2例)等。25例进展早期实验室检查结果示:白细胞计数正常14例(56%), 中性粒细胞绝对值正常19例(76%), 淋巴细胞绝对值降低21例(84%), CRP水平增高25例(100%), CD4+ T淋巴细胞计数降低21例(84%), 红细胞沉降率(erythrocyte sedimentation rate, ESR)增高25例(100%), 降钙素原水平增高25例(100%)。
25例患者中12例治愈出院(中位住院时间为25.5 d)、13例未治愈(死亡3例、住院时间>25 d且病情未缓解者10例)。治愈出院患者中危重型2例、重型10例, 未治愈患者均为危重型。12例治愈出院患者总住院时间为25.5(21.5, 30.0)d, 进展期住院时间为13.0(9.5, 17.0)d, 恢复期住院时间为11.5(10.5, 13.5)d。见表 1, 与未治愈患者相比, 治愈出院患者的BMI较低、从发病至进展为重型或危重型的时间较长、CD4+ T淋巴细胞计数较高, 差异均有统计学意义(t=-2.213、t=2.153、Z=2.720, P均<0.05)。见表 2, 多因素logistic回归分析结果显示, CD4+ T淋巴细胞计数高是重型及危重型COVID-19患者治愈出院的独立保护因素(P=0.031)。
|
|
表 1 治愈出院与未治愈COVID-19患者临床资料比较 Tab 1 Comparison of clinical data between cured and uncured COVID-19 patients |
|
|
表 2 COVID-19患者治愈出院影响因素的多因素logistic回归分析结果 Tab 2 Multivariate logistic regression analysis of influencing factors of cure and discharge of COVID-19 patients |
2.2 治愈出院患者进展期及恢复期实验室检查结果比较
见表 3, 分析12例治愈出院患者进展期及恢复期的实验室检查资料, 结果显示, 恢复期淋巴细胞绝对值、CD4+ T淋巴细胞计数均高于进展期, CRP水平、ESR、降钙素原水平均低于进展期, 差异均有统计学意义(t=-3.481、Z=3.059、t=5.914、t=4.068、Z=-2.936, P均<0.01)。
|
|
表 3 治愈出院COVID-19患者进展期与恢复期实验室检查结果比较 Tab 3 Comparison of laboratory examination results of cured COVID-19 patients between progressive stage and recovery stage |
2.3 胸部CT表现 2.3.1 基本表现
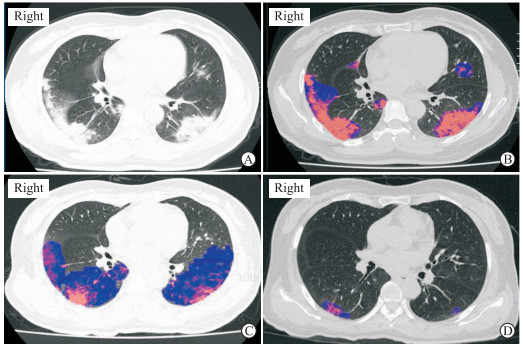
(1) 进展期(图 1A~1C):21例患者于进展期行胸部CT检查, 均表现为双肺多发病灶。其中20例呈斑片状或大片状磨玻璃影, 伴局部实变影;1例以实变为主, 病灶密度不均匀, 可见支气管充气征。随着病情进展, 病灶累及范围进一步扩大, 多沿支气管血管束、肺外周带、背侧胸膜下分布, 内部见血管增粗及小叶间隔增厚, 可见“铺路石”征。20例存在胸膜增厚, 9例有双侧少量胸腔积液, 8例可见纵隔淋巴结肿大。
|
图 1 1例COVID-19患者胸部CT表现及定量分析结果 Fig 1 Chest CT manifestations and quantitative analysis results of a COVID-19 patient A: Multiple consolidation and ground-glass opacity lesions were found in the lower lobe and subpleural periphery of both lungs, involving the pleura; B, C: Quantitative analysis suggested that the percentage of lesion volume progressed from 14.07% (B) at admission to a peak of 34.21% (C); D: Most of the lesions were absorbed at discharge, and the percentage of lesion volume was 1.66%. COVID-19: Coronavirus disease 2019; CT: Computed tomography |
(2) 恢复期(图 1D):12例治愈出院患者恢复期均复查胸部CT, 均表现为肺部磨玻璃影及实变影不同程度吸收, 并出现不同程度的小叶间隔增厚, 部分形成纤维网格影、不规则条索影, 病灶边界较前清楚;12例胸膜增厚及5例双侧少量胸腔积液均有不同程度吸收。出院前12例肺部病灶均有不同程度的纤维条索状残余灶, 其中1例出院前肺部局部存在蜂窝状改变及肺大疱, 1例肺部病灶大部分吸收后仅残留少许纤维条索灶。
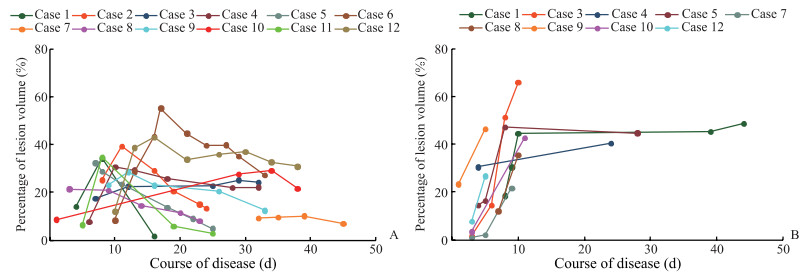
2.3.2 定量分析采用基于CT影像的智能化肺炎病灶定量分析软件计算入院时和进展期病灶体积百分比, 并进行比较, 结果显示, 入院时(21例患者入院时行CT检查)病灶体积百分比平均值为(14.76±9.15)%;进展期(20例复查CT)的峰值病灶体积百分比平均值为(37.42±11.48)%, 较入院时增高, 差异有统计学意义(t=-7.002, P<0.01);出院时(12例复查CT)病灶体积百分比平均值为(14.63±10.15)%, 较进展期峰值相比降低, 差异有统计学意义(t=5.664, P<0.01)。绘制病灶体积百分比随病程演变的曲线图可见, 12例治愈出院COVID-19患者病灶体积百分比在进展期明显增高, 吸收期降低, 呈倒V形(图 2A);未治愈患者病灶体积百分比在进展期(≥2次CT检查者9例)呈快速上升型(图 2B)。
|
图 2 COVID-19患者病灶体积百分比随病程演变的CT定量分析曲线 Fig 2 CT quantitative analysis curves of lesion volume percentage with disease course in COVID-19 patients A: The curves of the percentage of lesion volume with the course of disease in 12 cured COVID-19 patients; B: The curves of the percentage of lesion volume with the course of disease in nine uncured COVID-19 patients receiving CT examination for two or more times. COVID-19: Coronavirus disease 2019; CT: Computed tomography |
3 讨论
2019年底暴发流行的COVID-19由SARS-CoV-2感染所致, 备受全球各国家高度关注。SARS-CoV-2主要传播途径是经呼吸道飞沫和接触传播, 多数感染者症状轻微, 部分患者会出现肺炎、低氧血症, 甚至快速进展为ARDS、MODS等而死亡[1-5]。目前全球多个国家仍处于COVID-19流行高峰, 我国始终面临输入性病例的威胁, 本研究总结上海地区重型及危重型COVID-19患者的临床特征、实验室检查及胸部CT表现, 旨在为尽早控制疫情提供参考。
本组25例重型及危重型COVID-19患者的特点为年龄大、BMI高, 绝大多数病例有明确流行病学史, 并以发热、咳嗽为首发症状, 合并基础疾病常见;相比未治愈患者, 治愈出院患者的BMI较低、从发病至进展为重型或危重型的时间长、CD4+ T淋巴细胞计数高, 表明肥胖程度、疾病进展速度、免疫状态与COVID-19转归相关。进一步多因素logistic回归分析结果显示, CD4+ T淋巴细胞计数高为重型及危重型COVID-19患者治愈出院的独立保护因素, 可见免疫状态对疾病恢复具有重要作用。另外, 本研究比较了治愈出院患者进展期与恢复期的实验室检查数据发现, 经积极对症、支持治疗进入恢复期后淋巴细胞绝对值、CD4+ T淋巴细胞计数均回升, CRP水平、ESR及降钙素原水平均回降。上述结果与既往文献[1-5]报道相符, 说明重型及危重型COVID-19患者多为年龄较大、BMI偏高、合并基础疾病的人群, 淋巴细胞绝对值、CD4+ T淋巴细胞计数、CRP、ESR及降钙素原可作为重型及危重型COVID-19诊治及转归预测、病情监测的重要指标。
我国学者报告了COVID-19死亡病例的病理结果, 双肺存在弥漫性肺泡损伤伴细胞纤维黏液样渗出、透明膜形成, 肺间质可见以淋巴细胞为主的炎症细胞浸润, 肺泡腔内存在多核巨细胞及非典型性肥大肺泡上皮细胞[6]。上述病理结果提示, COVID-19患者肺部改变以弥漫性肺间质和肺泡损伤为主, 表现在CT图像上主要为多个肺段、肺叶斑片状和大片融合状磨玻璃影合并实变影。本组患者CT基本表现与既往报道[7-10]相似, 肺部磨玻璃影及实变影以双肺外周带及背侧分布为主, 但前期鲜有报道对治愈出院的重型及危重型COVID-19患者的胸部CT影像学特点进行研究。本研究不仅分析了重型及危重型COVID-19在进展期和恢复期的CT基本表现, 而且采用基于CT影像的智能化肺炎病灶定量分析软件定量分析病变进展及吸收过程的特点。本组病例进展期CT表现为肺部病变累及广泛, 肺实质及肺间质受累均存在, 主要为多肺段、肺叶渗出灶, 以外周带及背侧分布为主, 与其他重症病毒性肺炎表现[8, 11-16]相似;然而大部分重型及危重型COVID-19患者病灶累及胸膜, 表现为胸膜增厚及双侧少量胸腔积液, 这与H1N1、H7N9病毒性肺炎有所不同[11-12, 16-17], 分析原因可能与SARS-CoV-2致病性更强有关。经积极治疗, 本组12例治愈出院患者的呼吸道症状逐步改善, 肺部病灶不同区域均有不同程度的吸收好转, 且出现不同程度的小叶间隔增厚, 同时肺部因炎症反应机化形成不同程度网格状、不规则条索状高密度的慢性纤维化病灶。基于CT影像的智能化肺炎病灶定量分析在COVID-19的应用是目前研究的热点[18], 本研究通过定量分析获得的病灶体积百分比随病情变化曲线图, 定量、直观地显示了肺部炎症随病程的演变特点。
综上所述, 上海地区重型及危重型COVID-19患者多年龄较大、BMI偏高、合并基础疾病;重型及危重型COVID-19患者BMI低、病情进展慢、CD4+ T淋巴细胞计数高有利于其病情恢复;淋巴细胞绝对值、CRP、CD4+ T淋巴细胞计数、ESR和降钙素原等实验室指标及胸部CT影像学检查在COVID-19的诊断、病情监测及预后判断中有重要作用;另外, 基于CT影像的病灶定量分析有利于快速、客观、精准反映病灶进展或吸收趋势, 从而更精确地评估疗效。但通过CT影像学确诊COVID-19还缺乏特异性, 仍需依靠病原学检测结果确诊[1, 19]。
本研究存在以下不足:(1)样本量较小;(2)部分病例因病情危重未规律复查CT。加强对重型及危重型COVID-19患者的临床特征、CT基本表现及病灶定量评估分析, 提高对该病的认识, 有助于提高重型及危重型COVID-19患者的救治成功率。
| [1] |
中华人民共和国国家卫生健康委员会.新型冠状病毒肺炎诊疗方案(试行第六版)[EB/OL].(2020-02-18)[2020-02-26].http://www.nhc.gov.cn/yzygj/s7653p/202002/8334a8326dd94d329df351d7da8aefc2/files/b218cfeb1bc54639af227f922bf6b817.pdf.
|
| [2] |
CHEN N, ZHOU M, DONG X, QU J, GONG F, HAN Y, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study[J]. Lancet, 2020, 395: 507-513. DOI:10.1016/S0140-6736(20)30211-7 |
| [3] |
WANG D, HU B, HU C, ZHU F, LIU X, ZHANG J, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China[J]. JAMA, 2020, 323: 1061-1069. DOI:10.1001/jama.2020.1585 |
| [4] |
GUAN W J, NI Z Y, HU Y, LIANG W H, OU C Q, HE J X, et al. Clinical characteristics of coronavirus disease 2019 in China[J]. N Engl J Med, 2020, 382: 1708-1720. DOI:10.1056/NEJMoa2002032 |
| [5] |
HUANG C, WANG Y, LI X, REN L, ZHAO J, HU Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China[J]. Lancet, 2020, 395: 497-506. DOI:10.1016/S0140-6736(20)30183-5 |
| [6] |
XU Z, SHI L, WANG Y, ZHANG J, HUANG L, ZHANG C, et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome[J]. Lancet Respir Med, 2020, 8: 420-422. DOI:10.1016/S2213-2600(20)30076-X |
| [7] |
FANG Y, ZHANG H, XU Y, XIE J, PANG P, JI W. CT manifestations of two cases of 2019 novel coronavirus (2019-nCoV) pneumonia[J]. Radiology, 2020, 295: 208-209. DOI:10.1148/radiol.2020200280 |
| [8] |
SONG F, SHI N, SHAN F, ZHANG Z, SHEN J, LU H, et al. Emerging 2019 novel coronavirus (2019-nCoV) pneumonia[J]. Radiology, 2020, 295: 210-217. DOI:10.1148/radiol.2020200274 |
| [9] |
LEI J, LI J, LI X, QI X. CT imaging of the 2019 novel coronavirus (2019-nCoV) pneumonia[J/OL]. Radiology, 2020, 295: 18. doi: 10.1148/radiol.2020200236.
|
| [10] |
QIAN L, YU J, SHI H. Severe acute respiratory disease in a huanan seafood market worker: images of an early casualty[J/OL]. Radiol Cardiothorac Imaging, 2020, 2: e200033. doi: 10.1148/ryct.2020200033.
|
| [11] |
陆普选, 曾政, 郑斐群, 郑广平, 臧建, 王明星, 等. 人感染H7N9禽流感病毒性重症肺炎的影像学表现及动态变化特点[J]. 放射学实践, 2014, 29: 740-744. |
| [12] |
施裕新, 黎淑娟, 周粟, 施锁娣, 张志勇. 甲型H1N1流感胸部高分辨率CT表现[J]. 中华放射学杂志, 2010, 44: 127-129. DOI:10.3760/cma.j.issn.1005-1201.2010.02.005 |
| [13] |
周粟, 张志勇, 施裕新, 袁敏, 李涛, 尹化斌. 人感染H7N9禽流感重症死亡病例的临床与胸部影像表现[J]. 中华放射学杂志, 2013, 47: 832-833. DOI:10.3760/cma.j.issn.1005-1201.2013.09.018 |
| [14] |
黎淑娟, 张志勇, 施裕新, 张贵江, 张洁, 施锁娣, 等. 重症甲型H1N1流行性感冒肺炎高分辨率计算机X线断层扫描表现的动态变化[J]. 中华传染病杂志, 2011, 29: 615-618. DOI:10.3760/cma.j.issn.1000-6680.2011.10.014 |
| [15] |
马倩, 张志勇, 袁敏, 冯峰, 朱莹, 王青乐, 等. 人感染H7N9禽流感与H1N1重症病毒性肺炎的CT影像比较[J]. 中华放射学杂志, 2013, 47: 830-831. DOI:10.3760/cma.j.issn.1005-1201.2013.09.017 |
| [16] |
WANG Q, ZHANG Z, SHI Y, JIANG Y. Emerging H7N9 influenza A (novel reassortant avian-origin) pneumonia: radiologic findings[J]. Radiology, 2013, 268: 882-889. DOI:10.1148/radiol.13130988 |
| [17] |
梁德雄, 蒙光国, 罗文峰, 黎之利, 潘绍芳, 陆普选. 31例重症和危重症甲型H1N1流感患者的临床与影像学表现特点[J]. 放射学实践, 2010, 25: 961-964. DOI:10.3969/j.issn.1000-0313.2010.09.006 |
| [18] |
LIU F, ZHANG Q, HUANG C, SHI C, WANG L, SHI N, et al. CT quantification of pneumonia lesions in early days predicts progression to severe illness in a cohort of COVID-19 patients[J]. Theranostics, 2020, 12: 5613-5622. |
| [19] |
FANG Y, ZHANG H, XIE J, LIN M, YING L, PANG P, et al. Sensitivity of chest CT for COVID-19: comparison to RT-PCR[J/OL]. Radiology, 2020: 200432. doi: 10.1148/radiol.2020200432.
|
 2020, Vol. 41
2020, Vol. 41


