2. 解放军海军971医院中医科, 青岛 266071;
3. 海军军医大学(第二军医大学)东方肝胆外科医院中西医结合科, 上海 200438;
4. 空军军医大学第一附属医院中医科, 西安 710016;
5. 解放军 96604部队医院中医科, 兰州 730030;
6. 解放军南部战区空军医院中医科, 广州 510600;
7. 湖北省妇幼保健院光谷院区医务部, 武汉 430073;
8. 湖北省妇幼保健院光谷院区感染七科, 武汉 430073;
9. 解放军海军971医院保健三科, 青岛 266071;
10. 海军军医大学(第二军医大学)长征医院中医科, 上海 200003
2. Department of Traditional Chinese Medicine, No 971 Hospital of the PLA Navy, Qingdao 266071, Shandong, China;
3. Department of Integrative Medicine, Eastern Hepatobiliary Surgery Hospital, Naval Medical University(Second Military Medical University), Shanghai 200438, China;
4. Department of Traditional Chinese Medicine, the First Affiliated Hospital of Air Force Medical University, Xi'an 710016, Shaanxi, China;
5. Department of Traditional Chinese Medicine, No 96604 Troop Hospital of PLA, Lanzhou 730030, Gansu, China;
6. Department of Traditional Chinese Medicine, Air Force Hospital of Southern Theater Command of PLA, Guangzhou 510600, Guangdong, China;
7. Department of Medical Service, Guanggu Branch of Maternity and Child Healthcare Hospital of Hubei Province, Wuhan 430073, Hubei, China;
8. Department of Infectious Diseases(Ⅶ), Guanggu Branch of Maternity and Child Healthcare Hospital of Hubei Province, Wuhan 430073, Hubei, China;
9. Department of Healthcare(Ⅲ), No 971 Hospital of the PLA Navy, Qingdao 266071, Shandong, China;
10. Department of Traditional Chinese Medicine, Changzheng Hospital, Naval Medical University(Second Military Medical University), Shanghai 200003, China
新型冠状病毒肺炎(coronavirus disease 2019,COVID-19)特指感受新型冠状病毒而引起的一种急性疫病,其发病迅速、传染性强,危害较大[1-2]。疫病病因明确,与其他疾病相比,其临床突出特点是病程演变的规律性,表现为前驱期、进展期及恢复期等不同阶段。本文拟在横断面调查资料的基础上,按疾病阶段探讨COVID-19患者的证候特点,以期为其临床辨证用药提供参考。
1 资料和方法 1.1 研究对象湖北省妇幼保健院光谷院区2020年3月2日确诊为COVID-19的在院患者。纳入标准:符合《新型冠状病毒肺炎诊疗方案(试行第六版)》中制定的COVID-19确诊病例诊断标准[3]:(1)有流行病学史(武汉地区患者流行病学史均成立)。(2)符合COVID-19临床表现中的任意2条:①有发热和(或)呼吸道症状;②具有COVID-19影像学特征;③发病早期白细胞总数正常或降低,淋巴细胞计数减少。(3)有以下病原学证据之一:①qRT-PCR检测严重急性呼吸综合征冠状病毒2(severe acute respiratory syndrome coronavirus 2,SARS-CoV-2)核酸阳性;②病毒基因测序与已知SARS-CoV-2高度同源。另外,血清SARS-CoV-2特异性IgM和IgG阳性者[4]亦作为确诊患者纳入本研究。排除标准:(1)合并有心、肝、肾等严重慢性基础疾病且主要临床症状与COVID-19无关者;(2)患有中枢神经系统疾病或精神疾患等无法交流,不能配合完成中医四诊信息采集者;(3)无证可辨者。
1.2 研究方法采用横断面调查的方法,由湖北省妇幼保健院光谷院区中医诊疗专家组6名中医专家当日运用中医四诊信息采集表收集患者刻下中医临床资料,问诊了解其疾病发病时症状,所有数据由双人对照录入Excel数据表,数据校验率不低于10%。诊疗过程中因感染控制要求需戴3层手套,指感较差,因此未将脉象作为主要辨证依据。按照症状采集时间点,将患者起病症状定义为早期症状群,病程在7~30 d的患者症状纳入中期症状群,病程>30 d的患者症状纳入晚期症状群。
1.3 统计学处理应用SPSS 18.0软件进行统计学分析,患者年龄、病程为偏态分布资料,以中位数(下四分位数,上四分位数)表示;计数资料以例数和百分数表示。按不同病程阶段用频数法统计患者主要症状发生率,对高频症状(出现率>5.0%)运用层次聚类法进行聚类分析,结合专家经验总结其证候规律。
2 结果 2.1 一般资料共调查COVID-19患者804例,在排除48例(17例患者根据现有临床资料未能明确诊断,为疑似病例;22例患者有沟通障碍,无法获取全面四诊信息;9例患者无证可辨)无效病例后,最终756例患者纳入本研究。其中男313例、女443例;年龄为6~96岁,中位年龄为63(51,70)岁;病程为7~74 d,中位病程为30(18,39)d;轻型2例(0.26%),普通型610例(80.68%),重型122例(16.14%),危重型22例(2.91%)。临床症状以发热(52.25%,395/756)、苔腻(48.54%,367/756)、咳嗽(43.25%,327/756)、舌红(32.94%,249/756)、乏力(27.25%,206/756)、胸闷(26.72%,202/756)、大便不爽(22.62%,171/756)、口干(19.58%,148/756)、纳差(19.44%,147/756)、虚汗(17.59%,133/756)、失眠(11.38%,86/756)、便秘(10.58%,80/756)最为常见。
2.2 早期四诊信息及聚类分析756例COVID-19患者早期症状以发热、咳嗽、乏力、胸闷、气喘及咯痰最为常见,分别占52.25%(395例)、43.25%(327例)、27.25%(206例)、26.72%(202例)、17.59%(133例)和5.03%(38例),少见症状还有咽痛(2.51%,19例)、纳差(2.25%,17例)、恶寒(1.85%,14例)、心悸(1.32%,10例)、呕恶(1.19%,9例)等,另有18.12%(137例)的患者发病早期无任何症状,因社区普查而入院。
对6种出现频次较高(>5.0%)的症状进行层次聚类,除咯痰外其余5个最常见症状聚为一类(图 1),提示其在发病上具有高度相关性。结合中医病机分析,发热为邪气袭表、邪正交争所致;疫邪自口鼻而入,犯肺则咳嗽;乏力为湿邪外袭、困阻肌肉所致;胸闷、气喘一方面系肺系受邪,呼吸不利,一方面为湿困上焦所致的脘痞。综合分析,COVID-19患者早期基本病因病机为疫邪夹湿、袭表犯肺,总以湿遏肺卫为主。

|
图 1 COVID-19患者早期主要症状聚类分析树状图 COVID-19:新型冠状病毒肺炎 |
2.3 中期四诊信息及聚类分析
383例处于病程7~30 d COVID-19患者的症状以苔腻(64.49%,247例)、苔黄(43.86%,168例)、苔厚(40.21%,154例)、咳嗽(34.73%,133例)、舌红(32.38%,124例)、大便不畅(25.85%,99例)、气喘(25.33%,97例)、乏力(25.07%,96例)、纳差(23.76%,91例)、口苦(14.36%,55例)、苔燥(12.01%,46例)、舌紫(12.01%,46例)、虚汗(11.49%,44例)、便秘(10.18%,39例)、白痰(8.62%,33例)、失眠(7.31%,28例)、恶心(7.05%,27例)、腹泻(6.79%,26例)和黄痰(6.27%,24例)最为常见。少见症状还有肌肉酸痛(4.96%,19例)、腹泻(4.18%,16例)、发热(3.66%,14例)、黄痰(3.66%,14例)、苔少(3.66%,14例)、咽痛(3.66%,11例)等。
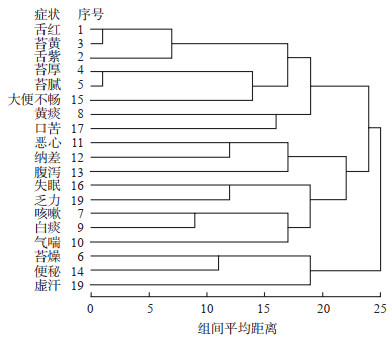
对上述常见症状进行层次聚类,19个变量聚为3类:舌紫、红,苔黄、厚、腻,大便不畅,黄痰和口苦8个变量为一类;恶心、纳差、腹泻、乏力、失眠、咳嗽、白痰和气喘8个变量归为一类;苔燥、便秘、虚汗3个变量归为另一类(图 2)。结合中医病机分析,口苦、大便不畅,舌红而紫、苔黄厚腻提示湿热内蕴,吐黄痰为痰热阻肺,总属湿热为患;恶心、纳差、乏力、腹泻为湿邪困脾、纳化失职,咳嗽、白痰为痰浊阻肺,失眠为脾虚不荣,心失所养,总属湿阻肺脾;便秘、虚汗、苔燥为邪入阳明化燥征象,提示湿热化燥伤阴。综合分析,COVID-19患者中期症候以湿阻肺脾证和湿热蕴肺证最为常见,部分患者可湿热化燥,提示病情可能转危,可能引发疫毒闭肺。
|
图 2 COVID-19患者中期主要症状聚类分析树状图 COVID-19:新型冠状病毒肺炎 |
2.4 后期四诊信息及聚类分析
373例病程>30 d COVID-19患者的症状以苔腻(50.94%,190例)、乏力(39.41%,147例)、咳嗽(37.80%,141例)、舌红(33.78%,126例)、气喘(32.17%,120例)、虚汗(23.86%,89例)、口干(22.79%,85例)、纳差(20.11%,75例)、大便不畅(19.30%,72例)、口苦(15.01%,56例)、白痰(10.72%,40例)、心悸(8.31%,31例)和苔少(8.04%,30例)为常见。少见症状有恶心(4.56%,17例)、黄痰(3.49%,13例)、肌肉酸痛(3.22%,12例)、舌淡白(2.41%,9例)等。
对上述常见症状进行系统聚类,13个变量聚为2类:口干、虚汗、乏力、口苦、心悸、舌红、苔少7个变量归为一类;咳嗽、白痰、气喘、纳差、大便不畅、苔腻6个变量归为一类(图 3)。结合中医病机分析,口干、虚汗、乏力、心悸、舌红、苔少均提示气阴受损,口苦为湿热尚存;咳嗽、气喘、白痰提示肺气受损、宣肃不利,纳差、大便不畅、苔腻为湿邪困脾、纳化失职,总属肺脾两虚所致。综合分析,COVID-19患者后期证候以气阴两虚证和肺脾气虚证最为常见,其病机以虚为主,兼夹余湿未清。

|
图 3 COVID-19患者后期主要症状聚类分析树状图 COVID-19:新型冠状病毒肺炎 |
3 讨论
COVID-19系感受天地间杂气——疫疠之邪所致。武汉地处江汉平原东部,长江及其最大支流汉江在城中交汇,市内江河纵横、湖港交织,水域面积占全市总面积的四分之一。2019年12月左右,武汉地区气候湿冷,因此此次疫情具有明显的夹“湿”特点。其总的发病机制为外感引动伏邪。外感多湿,初起邪遏肺卫,出现发热、乏力、胸闷脘痞等湿邪郁闭肌表症状,疫邪自口鼻而入,鼻气通于肺,口气通于脾,故发病后兼见咳嗽等肺系和纳差、腹泻等脾胃症状。随着病情进展,外感引动伏邪,伏邪属“毒”,藏于太阴肺、脾,发则并见咳甚、气喘、纳差、大便不爽、舌苔厚腻等表现,湿毒胶结,蕴蒸不化,往往缠绵难愈;其间湿毒逐渐化热,出现口苦、舌红、苔黄等湿热内蕴之象。少部分患者还可能湿热化燥,出现闭肺、壅肠而病情转重。进入恢复期后,患者表现为肺脾正气受损,兼有余邪未清,表现为咳嗽、吐痰、口干、乏力及纳差、苔腻、大便不爽等。
本研究结果显示,多数COVID-19患者初起以发热(52.25%,395/756)、咳嗽(43.25%,327/756)、乏力(27.25%,206/756)、胸闷(26.72%,202/756)、气喘(17.59%,133/756)等症状为主,此阶段相当于该病的早期(前驱期),此时邪气尚表浅,多数患者尚无肺炎表现,与王玉光等[5]的报道基本一致。值得注意的是,早期无症状、因社区普查而入院的患者占18.12%(137/756),这一数据需引起重视,提示早期无症状的患者临床并不少见。聚类分析显示,COVID-19患者早期基本病因病机为疫邪夹湿、袭表犯肺,总以湿遏肺卫为主;中期患者反不发热,以湿阻肺脾证和湿热蕴肺证最为常见,此阶段相当于疾病的进展期,部分患者还可湿热化燥,提示病情可能转危,引发疫毒闭肺的危证;后期患者证候以气阴两虚证和肺脾气虚证最为常见,其病机以虚为主,兼有余湿未清,此阶段相当于疾病的恢复期。
本研究基于不同病程阶段探索了COVID-19的证候规律,发现随病程进展其证候的确具有明显的规律性,呈现由表入里、由湿化热、由实转虚的特征性变化,可认为早期(前驱期)以湿遏肺卫证为主,中期(进展期)表现为湿阻肺脾证或湿热蕴肺证,部分患者还可能会出现疫毒闭肺的危症,后期(恢复期)以(肺脾)气阴两虚证或肺脾气虚证为主,兼有余湿未清。这种规律有助于帮助临床医师辨证与辨病相结合,更快捷地把握COVID-19辨证治疗规律。当然,本研究结果是基于横断面调查研究,其是否契合临床后续还有待COVID-19患者证候的动态观测数据以进一步证实。
| [1] |
GUAN W J, NI Z Y, HU Y, LIANG W H, OU C Q, HE J X, et al. Clinical characteristics of coronavirus disease 2019 in China[J/OL]. N Engl J Med, 2020. doi: 10.1056/NEJMoa2002032.
|
| [2] |
ZHOU F, YU T, DU R, FAN G, LIU Y, LIU Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China:a retrospective cohort study[J]. Lancet, 2020, 395: 1054-1062. DOI:10.1016/S0140-6736(20)30566-3 |
| [3] |
中华人民共和国国家卫生健康委员会.新型冠状病毒肺炎诊疗方案(试行第六版)[EB/OL].(2020-02-18)[2020-03-20].http://www.nhc.gov.cn/yzygj/s7653p/202002/8334a8326dd94d329df351d7da8aefc2/files/b218cfeb1bc54639af227f922bf6b817.pdf.
|
| [4] |
徐万洲, 李娟, 何晓云, 张才庆, 梅四青, 李从荣, 等.血清2019新型冠状病毒IgM和IgG抗体联合检测在新型冠状病毒感染中的诊断价值[J/OL].中华检验医学杂志, 2020. doi: 10.3760/cma.j.cn114452-20200223-00109.
|
| [5] |
王玉光, 齐文升, 马家驹, 阮连国, 卢幼然, 李旭成, 等.新型冠状病毒肺炎中医临床特征与辨证治疗初探[J/OL].中医杂志, 2020, 61.doi: 10.13288/j.11-2166/r.2020.04.002.
|
 2020, Vol. 41
2020, Vol. 41


