2. 海军军医大学(第二军医大学)长海医院风湿免疫科, 上海 200433
2. Department of Rheumatology and Immunology, Changhai Hospital, Naval Medical University(Second Military Medical University), Shanghai 200433, China
皮肌炎(dermatomyositis,DM)是一种特发性炎症性病变,主要累及皮肤与骨骼肌,通常表现为进行性肌无力及皮疹,可同时伴有心脏、胃肠道、肺等器官损害[1]。DM临床表现具有异质性,不存在特征性皮肤病变或肌病的情况下难以诊断[2-3]。DM患者生活质量差,早期诊断和治疗有利于长期预后[4]。中性粒细胞与淋巴细胞比值(neutrophil-lymphocyte ratio,NLR)是一项易于获得的实验室指标[5],在类风湿关节炎(rheumatoid arthritis,RA)、多发性硬化(multiple sclerosis,MS)、强直性脊柱炎(ankylosing spondylitis,AS)和自身免疫性甲状腺炎等炎症性疾病中,其可作为反映基础炎症状态经济且有效的替代标志物,并与疾病活动度密切相关[6-8]。目前NLR与DM疾病活动度相关性的报道很少,本研究的目的是确定DM患者NLR水平及其与实验室指标的相关性,探讨NLR在DM诊断及疾病活动度中的作用。
1 资料和方法 1.1 研究对象回顾性分析2016年1月至2019年12月于海军军医大学(第二军医大学)长征医院及长海医院风湿免疫科初次住院治疗的DM患者资料,DM诊断均符合欧洲神经肌肉疾病中心和美国肌肉研究协作组2004年提出的特异性炎症性病变分类诊断标准[4]。排除标准:(1)入院前有糖皮质激素和(或)免疫抑制剂使用史者;(2)入院时伴有慢性、急性感染者;(3)伴有肝脏疾病者;(4)伴有其他自身免疫性疾病者;(5)伴发肿瘤者。从长征医院同期健康体检人群中选择31名健康志愿者作为健康对照组,住院患者中选择初发RA患者26例和AS患者27例作为疾病对照组,RA诊断符合美国风湿病协会RA诊断标准[9],AS诊断符合1984年修订的纽约标准[10]。本研究通过海军军医大学(第二军医大学)长征医院及长海医院医学伦理委员会审批。
1.2 临床及实验室资料DM、RA、AS组通过查阅患者初次入院病历,收集患者一般资料、临床表现(包括发热、乏力、骨骼肌受累情况、皮疹等)及住院期间实验室检查结果[包括血常规、血生物化学全套、红细胞沉降率(erythrocyte sedimentation rate,ESR)等],经糖皮质激素或环磷酰胺冲击治疗后病情好转且出院前复查资料完整的DM患者有35例。健康对照组收集清晨空腹静脉血,检测血常规、血生物化学全套、ESR等。
1.3 统计学处理应用GraphPad Prism 8软件进行数据分析。计数资料以例数和百分数表示,组间比较采用χ2检验。呈偏态分布的计量资料以中位数(下四分位数,上四分位数)表示,两组间资料比较采用Mann-Whitney U检验,治疗前后资料比较采用配对Wilcoxon符号秩检验。采用Spearman秩相关分析研究NLR与其他指标之间的相关性。采用ROC曲线评估NLR对DM的诊断价值,通过计算约登指数确定最佳截断值,并计算灵敏度和特异度,ROC AUC的比较采用Z检验。检验水准(α)为0.05。
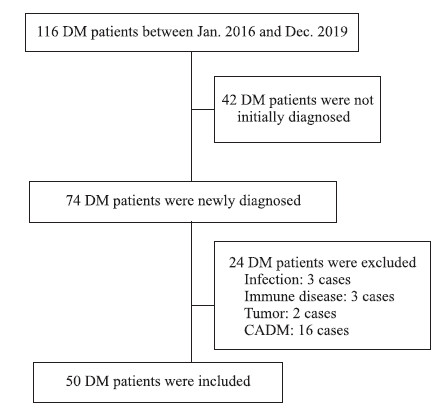
2 结果 2.1 一般资料如图 1所示,2016年1月至2019年12月于长征医院及长海医院风湿免疫科住院治疗的DM患者共116例(长征医院47例,长海医院69例),排除42例非初次就诊患者,余74例患者中16例诊断为无肌病性皮肌炎(clinically amyopathic dermatomyositis,CADM),因其临床表现、并发症及预后不同于DM[11],不纳入本研究;排除感染3例、免疫性疾病3例、肿瘤2例,最终本研究共纳入DM患者50例。
|
图 1 纳入患者筛选流程图 Fig 1 Screening flowchart of included patients DM: Dermatomyositis; CADM: Clinically amyopathic dermatomyositis |
健康对照和DM、RA、AS患者的基线资料见表 1。DM患者中男20例、女30例,年龄为56.0(50.5,68.5)岁(17~82岁),病程为2.0(1.0,5.7)个月。健康对照男13名、女18名,年龄为50.0(41.5,59.0)岁(23~75岁)。RA患者男10例、女16例,年龄为64.0(55.0,71.0)岁(47~88岁)。AS患者男18例、女9例,年龄为48.0(38.0,56.0)岁(27~72岁)。健康对照与DM患者、健康对照与RA患者、DM患者与RA患者之间性别构成比差异均无统计学意义(χ2=0.03、0.07、0.02,P均>0.05)。AS患者男性比例高于DM患者和RA患者(χ2=4.20、5.00,P均 < 0.05)。RA患者年龄大于健康对照、DM患者和AS患者(U=155.5、432.0、101.5,P均 < 0.05),AS患者年龄小于DM患者(U=385.5,P < 0.01)。DM、RA和AS患者NLR均高于健康对照(U=29.0、156.0、194.0,P均 < 0.01),DM患者NLR高于RA和AS患者(U=333.0、213.0,P均 < 0.01)。DM患者其他实验室指标肌酸激酶(creatine kinase,CK)、乳酸脱氢酶(lactic dehydrogenase,LDH)、天冬氨酸转氨酶(aspartate aminotransferase,AST)和丙氨酸转氨酶(alanine aminotransferase,ALT)水平均高于健康对照、RA患者和AS患者(DM患者vs健康对照U=117.0、68.5、206.0、134.5,DM患者vs RA患者U=154.0、89.0、158.0、95.0,DM患者vs AS患者U=195.0、24.5、119.5、163.5;P均 < 0.01)。
|
|
表 1 健康对照和DM、RA、AS患者基线资料比较 Tab 1 Comparison of baseline data between healthy controls and DM, RA and AS patients |
2.2 DM患者NLR与其他实验室指标的相关性分析
Spearman秩相关分析结果显示,DM患者的NLR与CK、LDH、AST、ALT、CRP和ESR均呈正相关(rs=0.540,P < 0.001;rs=288,P=0.042;rs=440,P=0.002;rs=498,P < 0.001;rs=304,P=0.038;rs=311,P=0.029),见图 2。

|
图 2 DM患者NLR与其他实验室指标Spearman秩相关分析 Fig 2 Spearman rank correlation analysis of NLR and other laboratory indexes in DM patients DM: Dermatomyositis; NLR: Neutrophil-lymphocyte ratio; CK: Creatine kinase; LDH: Lactic dehydrogenase; AST: Aspartate aminotransferase; ALT: Alanine aminotransferase; CRP: C-reactive protein; ESR: Erythrocyte sedimentation rate |
2.3 血NLR对DM的诊断价值
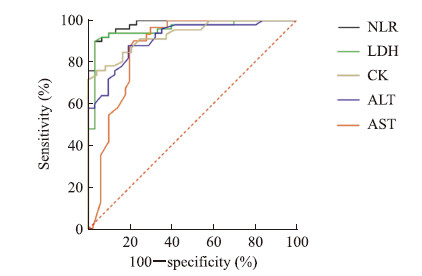
如图 3所示,NLR、LDH、CK、ALT、AST诊断DM的ROC AUC分别为0.981、0.954、0.931、0.913、0.867,根据约登指数最大值计算NLR、LDH、CK、ALT、AST诊断DM的最佳截断值分别为2.824、241.0 U/L、101.0 U/L、25.50 U/L、30.00 U/L,诊断灵敏度分别为90.00%、90.00%、76.09%、88.00%、90.32%,对应的特异度分别为96.67%、96.67%、95.83%、80.65%、78.00%。
|
图 3 NLR、LDH、CK、ALT、AST诊断DM的ROC曲线分析 Fig 3 ROC curves of NLR, LDH, CK, ALT and AST for diagnosis of DM NLR: Neutrophil-lymphocyte ratio; LDH: Lactic dehydrogenase; CK: Creatine kinase; ALT: Alanine aminotransferase; AST: Aspartate aminotransferase; DM: Dermatomyositis; ROC: Receiver operating characteristic |
对ROC AUC进行比较,NLR诊断DM的ROC AUC高于ALT与AST(Z=2.05、2.67,P=0.040、0.008),其他各指标诊断DM的ROC AUC差异均无统计学意义(P均>0.05)。见表 2。
|
|
表 2 NLR、AST、ALT、LDH诊断DM ROC曲线下面积比较 Tab 2 Comparison of area under ROC curves of NLR, AST, ALT and LDH for diagnosis of DM |
2.4 DM患者治疗前后实验室指标比较
住院期间经合理治疗后,DM患者NLR和CK、LDH、AST、ALT水平均下降,与治疗前相比差异均有统计学意义(Z=3.28、4.68、4.44、4.62、2.12,P均 < 0.05),见表 3。
|
|
表 3 DM患者治疗前后实验室指标比较 Tab 3 Comparison of laboratory indexes before and after treatment in DM patients |
3 讨论
DM是一种慢性炎症性自身免疫性疾病,主要累及肌肉和皮肤,可同时伴有多个器官损害及恶性肿瘤,实验室检查可有血清Ig、肌酶升高,补体降低。DM发病机制尚不清楚,细胞因子和趋化因子增强免疫应答在DM发病过程中发挥重要作用[12],中性粒细胞和淋巴细胞参与细胞因子和趋化因子的产生。近年来,以淋巴细胞和中性粒细胞为代表的白细胞及其分类计数已被报道可作为多种疾病的生物标志物[5, 7-8]。铁蛋白、抗黑素瘤分化相关基因5(anti-melanoma differentiation-associated gene 5,MDA5)、涎液化糖链抗原(Krebs von den Lungen-6,KL-6)被用于快速预测DM病情进展,但这些生物标志物检测复杂且费用较高[13],因此有必要进一步探索方便且经济的生物标志物。
既往有关NLR与DM相关性的研究很少,有研究表明NLR升高是DM患者生存预后独立且重要的危险因素[14],另一项研究证明DM患者NLR与CRP、ESR呈正相关[15],但这些研究均未对NLR与其他实验室指标的相关性进行分析,也未对不同自身免疫疾病患者的NLR进行对比。本研究中,DM患者NLR高于健康对照,且ALT、AST和LDH水平亦均高于健康对照,同时尽管RA、AS和DM患者NLR均高于健康对照,但RA与AS患者NLR较DM患者低,提示一定水平的NLR对于DM诊断具有一定临床价值,ROC曲线分析结果也进一步证明了NLR对DM的诊断价值。
CK水平可以反映DM疾病活动度,其他肌酶如LDH、AST和ALT也可能与疾病活动度有关[1],其中CK对诊断DM最灵敏,发病时其可升高至正常值上限的50倍,可作为诊断DM的实验室指标之一[4]。本研究结果显示,DM患者NLR不仅与ESR和CRP呈正相关,而且与肌肉损伤相关肌酶CK、AST、ALT和LDH呈正相关,说明NLR与DM疾病活动度及病情有关。因此NLR可作为一种具有成本效益、快速、可靠的非特异性炎症标志物,辅助CK用于评估DM全身炎症情况与疾病活动度,同时评估肌肉损伤程度。本研究中,DM患者经过合理治疗后NLR和CK、LDH、AST、ALT水平均下降,表明NLR可以反映患者病情变化,并预测治疗转归。
综上所述,NLR作为一种经济、简单、可重复的炎症标志物,在DM诊断和鉴别诊断(RA、AS)中具有潜在临床价值,其与DM患者肌肉损伤相关肌酶CK、AST、ALT和LDH呈正相关,可反映疾病活动度,并且在治疗病情好转后下降。本研究存在以下不足之处:(1)为单中心回顾性研究,样本量小,需开展大规模多中心前瞻性临床研究进一步证实;(2)为横断面研究,今后应规律随访患者开展纵向研究,进一步明确NLR是否在DM并发恶性肿瘤及预后评估中发挥作用。
| [1] |
FINDLAY A R, GOYAL N A, MOZAFFAR T. An overview of polymyositis and dermatomyositis[J]. Muscle Nerve, 2015, 51: 638-656. DOI:10.1002/mus.24566 |
| [2] |
LONG K, DANOFF S K. Interstitial lung disease in polymyositis and dermatomyositis[J]. Clin Chest Med, 2019, 40: 561-572. DOI:10.1016/j.ccm.2019.05.004 |
| [3] |
DEWANE M E, WALDMAN R, LU J. Dermatomyositis:clinical features and pathogenesis[J]. J Am Acad Dermatol, 2020, 82: 267-281. DOI:10.1016/j.jaad.2019.06.1309 |
| [4] |
HOOGENDIJK J E, AMATO A A, LECKY B R, CHOY E H, LUNDBERG I E, ROSE M R, et al. 119th ENMC International Workshop:trial design in adult idiopathic inflammatory myopathies, with the exception of inclusion body myositis, 10-12 October 2003, Naarden, the Netherlands[J]. Neuromuscul Disord, 2004, 14: 337-345. DOI:10.1016/j.nmd.2004.02.006 |
| [5] |
NISHIDA Y, HOSOMI S, YAMAGAMI H, SUGITA N, ITANI S, YUKAWA T, et al. Pretreatment neutrophilto-lymphocyte ratio predicts clinical relapse of ulcerative colitis after tacrolimus induction[J/OL]. PLoS One, 2019, 14: e0213505. doi: 10.1371/journal.pone.0213505.
|
| [6] |
BISGAARD A K, PIHL-JENSEN G, FREDERIKSEN J L. The neutrophil-to-lymphocyte ratio as disease actvity marker in multiple sclerosis and optic neuritis[J]. Mult Scler Relat Disord, 2017, 18: 213-217. DOI:10.1016/j.msard.2017.10.009 |
| [7] |
CHANDRASHEKARA S, MUKHTAR AHMAD M, RENUKA P, ANUPAMA K R, RENUKA K. Characterization of neutrophil-to-lymphocyte ratio as a measure of inflammation in rheumatoid arthritis[J]. Int J Rheum Dis, 2017, 20: 1457-1467. DOI:10.1111/1756-185X.13157 |
| [8] |
KESKIN H, KAYA Y, CADIRCI K, KUCUR C, ZIYPAK E, SIMSEK E, et al. Elevated neutrophillymphocyte ratio in patients with euthyroid chronic autoimmune thyreotidis[J]. Endocr Regul, 2016, 50: 148-153. DOI:10.1515/enr-2016-0017 |
| [9] |
ARNETT F C, EDWORTHY S M, BLOCH D A, MCSHANE D J, FRIES J F, COOPER N S, et al. The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis[J]. Arthritis Rheum, 1988, 31: 315-324. DOI:10.1002/art.1780310302 |
| [10] |
VAN DER LINDEN S, VALKENBURG H A, CATS A. Evaluation of diagnostic criteria for ankylosing spondylitis. A proposal for modification of the New York criteria[J]. Arthritis Rheum, 1984, 27: 361-368. DOI:10.1002/art.1780270401 |
| [11] |
UDKOFF J, COHEN P R. Amyopathic dermatomyositis:a concise review of clinical manifestations and associated malignancies[J]. Am J Clin Dermatol, 2016, 17: 509-518. DOI:10.1007/s40257-016-0199-z |
| [12] |
OLAZAGASTI J M, NIEWOLD T B, REED A M. Immunological biomarkers in dermatomyositis[J/OL]. Curr Rheumatol Rep, 2015, 17: 68. doi: 10.1007/s11926-015-0543-y.
|
| [13] |
KOBAYASHI N, TAKEZAKI S, KOBAYASHI I, IWATA N, MORI M, NAGAI K, et al. Clinical and laboratory features of fatal rapidly progressive interstitial lung disease associated with juvenile dermatomyositis[J]. Rheumatology (Oxford), 2015, 54: 784-791. DOI:10.1093/rheumatology/keu385 |
| [14] |
HA Y J, HUR J, GO D J, KANG E H, PARK J K, LEE E Y, et al. Baseline peripheral blood neutrophil-tolymphocyte ratio could predict survival in patients with adult polymyositis and dermatomyositis: a retrospective observational study[J/OL]. PLoS One, 2018, 13: e0190411. doi: 10.1371/journal.pone.0190411.
|
| [15] |
YANG W, WANG X, ZHANG W, YING H, XU Y, ZHANG J, et al. Neutrophil-lymphocyte ratio and platelet-lymphocyte ratio are 2 new inflammatory markers associated with pulmonary involvement and disease activity in patients with dermatomyositis[J]. Clin Chim Acta, 2017, 465: 11-16. DOI:10.1016/j.cca.2016.12.007 |
 2020, Vol. 41
2020, Vol. 41


