2. 火箭军特色医学中心骨科, 北京 100088
2. Department of Orthopaedics, Special Medical Center of PLA Rocket Force, Beijing 100088, China
Dubousset[1]曾提出“经济圆锥”的概念,认为在“经济圆锥”范围内个体能够在消耗最少能量的前提下保持姿势平衡。但随着年龄增大腰椎退变加重,老年患者的躯干重心常会偏离这个范围。骨盆后倾、胸椎过伸、膝关节和髋关节屈曲、踝关节背伸等代偿机制都需要额外消耗能量[2-4]。矢状面失平衡与生活质量评分降低密切相关,一旦个体肌肉疲劳无法调动这些代偿机制,则会发生矢状面失平衡、疼痛加重、功能障碍等[5-6]。
对于代偿机制何时失灵及为何会失灵,目前尚无定论。活动强度和种类都可能会影响个体调动代偿机制而维持直立姿势的能力,并且个体每天在进行不同的活动时矢状面平衡情况也会发生改变。因此,成人脊柱侧凸患者仅拍摄1次静态的全脊柱正侧位X线片并不能准确反映患者矢状面的动态变化和功能障碍程度。本研究旨在评估成人脊柱侧凸患者长时间行走前后整体和局部的影像学参数,并且基于患者初始的矢状面平衡状态评估长时间行走后代偿机制的改变。
1 资料和方法 1.1 研究对象与分组选择2016年1月至2018年6月于海军军医大学(第二军医大学)长征医院就诊的成人脊柱侧凸患者125例。纳入标准:(1)典型的腰椎前凸丢失(骨盆投射角-腰椎前凸角>10°);(2)冠状面无主弯(侧凸Cobb角 < 30°)。排除标准:(1)有压缩性骨折病史;(2)髋关节病变;(3)脊柱滑脱;(4)典型的腰椎管狭窄症;(5)特发性或神经肌源性脊柱侧凸;(6)冠状面侧凸Cobb角≥ 30°;(7)休门病。所有纳入患者在完成第1次站立位全脊柱正侧位X线片拍摄后,立即在门诊走廊匀速步行15 min,在此期间不能坐下或靠墙休息,随后再次拍摄站立位全脊柱正侧位X线片。由1名科研助理负责监督患者的步行过程。根据行走前矢状面参数将患者分为两组:代偿组(行走前矢状面平衡,矢状面躯干偏移 < 40 mm且骨盆倾斜角>20°)和失代偿组(行走前矢状面失平衡,矢状面躯干偏移≥ 40 mm且骨盆倾斜角>20°)。本研究通过海军军医大学(第二军医大学)长征医院医学伦理委员会审批。
1.2 影像学参数评估所有纳入患者均行站立位全脊柱正侧位X线片检查,运用医学影像信息系统(picture archiving and communication system,PACS)测量以下影像学参数。(1)矢状面躯干偏移:C7铅垂线至S1后上角垂线的水平距离;(2)胸椎后凸角:T5上终板与T12下终板延长线的夹角;(3)腰椎前凸角:L1上终板与S1上终板延长线的夹角;(4)骨盆入射角:S1上终板中点和双侧股骨头中心的连线与S1上终板垂线的夹角;(5)骨盆倾斜角:S1终板中点和双侧股骨头中心的连线与垂线的夹角;(6)骶骨倾斜角:S1上终板和水平线的夹角。
1.3 统计学处理应用SPSS 20.0软件进行统计学分析。呈正态分布的计量资料以x±s表示,两组间比较采用独立样本t检验;呈偏态分布的计量资料以中位数(下四分位数,上四分位数)表示,两组间比较采用Mann-Whitney U检验,组内步行15 min前后脊柱矢状面参数的比较采用Wilcoxon符号秩检验;计数资料以例数和百分数表示,两组间比较采用χ2检验。每组步行15 min前后矢状面躯干偏移变化值与其余矢状面参数变化值的相关性分析采用Spearman相关分析。检验水准(α)为0.05。
2 结果 2.1 纳入研究对象基本资料共纳入98例成人脊柱侧凸患者,其中女83例、男15例,年龄为57~74岁,平均(65.4±6.8)岁。代偿组19例(19.4%),其中女16例、男3例,年龄为58~69岁,平均(64.1±5.9)岁,BMI为(24.2±4.6)kg/m2;失代偿组79例(80.6%),其中女67例、男12例,年龄为57~74岁,平均(66.7±7.2)岁,BMI为(24.9±5.1)kg/m2;两组患者性别构成比、年龄、BMI差异均无统计学意义(χ2=0.004,P=0.948;t=1.459,P=0.148;t=0.547,P=0.586)。
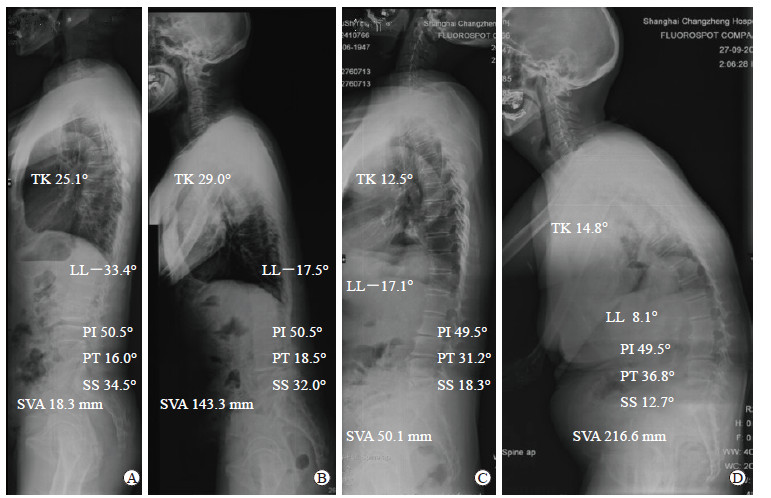
2.2 两组患者步行前后矢状面参数比较步行前,代偿组患者腰椎前凸角大于失代偿组,差异有统计学意义(Z=2.784,P=0.003);代偿组骨盆入射角-腰椎前凸角和矢状面躯干偏移均小于失代偿组,差异均有统计学意义(Z=1.953,P=0.028;Z=3.815,P < 0.01);两组骨盆倾斜角、骶骨倾斜角、胸椎后凸角差异均无统计学意义(P均>0.05)。步行15 min后,代偿组中有15例患者出现矢状面失平衡,失代偿组所有患者均矢状面失平衡;两组间骨盆倾斜角、骶骨倾斜角、腰椎前凸角、胸椎后凸角、骨盆入射角-腰椎前凸角、矢状面躯干偏移差异均无统计学意义(P均>0.05)。代偿组和失代偿组患者步行15 min后骶骨倾斜角、骨盆入射角-腰椎前凸角、矢状面躯干偏移均较步行前增大,骨盆倾斜角和腰椎前凸角均较步行前减小,差异均有统计学意义(代偿组Z=1.718、P=0.043,Z=2.198、P=0.015,Z=3.875、P < 0.01,Z=1.639、P=0.047,Z=3.624、P < 0.01;失代偿组Z=1.842、P=0.031,Z=1.943、P=0.021,Z=2.917、P=0.002,Z=1.812、P=0.039,Z=3.893、P < 0.01);失代偿组患者步行15 min后胸椎后凸角也较步行前增大,差异有统计学意义(Z=2.287,P=0.012)。见表 1和图 1。
|
|
表 1 两组成人脊柱侧凸患者步行15 min前后矢状面参数 Tab 1 Sagittal parameters of adult scoliosis patients before and after a 15-min walk in two groups |
|
图 1 两组成人脊柱侧凸患者的典型影像学表现 Fig 1 Representative radiographs of adult scoliosis patients in two groups A, B: Compensated group, a 59-year-old woman with adult scoliosis; C, D: Decompensated group, a 63-year-old woman with adult scoliosis. A, C: Before a 15-min walk; B, D: After a 15-min walk. TK: Thoracic kyphosis; LL: Lumbar lordosis; PI: Pelvic incidence; PT: Pelvic tilt; SS: Sacral slope; SVA: Sagittal vertical axis |
2.3 两组患者步行前后矢状面躯干偏移变化值与其余矢状面参数变化值的相关性
代偿组、失代偿组患者步行15 min前后矢状面躯干偏移变化值均与骨盆倾斜角变化值呈负相关(rs=-0.519、-0.625,P=0.024、0.001),与骶骨倾斜角变化值、腰椎前凸角变化值、骨盆入射角-腰椎前凸角变化值均呈正相关(代偿组rs=0.519、0.645、0.645,P=0.024、0.003、0.003;失代偿组rs=0.625、0.407、0.407,P=0.001、0.005、0.005)。见表 2。
|
|
表 2 两组成人脊柱侧凸患者步行15 min前后矢状面躯干偏移变化值与其余矢状面参数变化值的相关性 Tab 2 Correlation between difference of sagittal vertical axis and differences of other sagittal parameters of adult scoliosis patients before and after a 15-min walk in two groups |
3 讨论
本研究拓展了对成人脊柱侧凸患者长时间行走后矢状面参数变化的认识。之所以选择15 min作为长时间行走标准,是因为既要保证足够的运动持续时间,又要兼顾门诊患者的依从性。代偿组和失代偿组患者步行15 min后矢状面躯干偏移均较步行前增大,腰椎前凸角均较步行前减小(P均 < 0.01),表明大多数合并腰椎前凸角减小的成人脊柱侧凸患者在步行15 min后可能出现矢状面失平衡;并且在矢状面失代偿患者中,可能至少有1种代偿机制减弱或消失,如骨盆后倾减小、胸椎过伸减小、腰椎前凸减小等。
对脊柱平衡及其相关影响因素的全面理解是准确评估患者病情、制定个体化手术策略的重要基础。Barrey等[2]提出成人脊柱侧凸畸形矢状面特点可以分为平衡、代偿机制下平衡、失平衡3个阶段。在后2个阶段,机体会调动一系列脊柱本身和脊柱外的代偿机制以维持直立姿势。脊柱本身的代偿包括骨盆后倾、胸椎过伸、腰椎相邻节段椎间隙夹角>15°、腰椎相邻节段后滑脱、颈椎过度前凸。脊柱外的代偿机制主要涉及下肢状态改变,包括髋关节和膝关节屈曲、踝关节背伸[6-10]。这些代偿机制依赖于竖脊肌、屈髋肌、股后肌群、股四头肌的收缩和相互配合[11-13],这些肌群正常收缩和舒张维持矢状面平衡。但随着活动时间的延长,这些肌群不可避免地出现疲劳并最终无法维持矢状面平衡[3, 14]。除了肌群的疲劳,小关节突刺激和相邻节段棘间压力过高也会引起继发性疼痛,从而导致代偿机制持续性减弱。
本研究中,80.6%(79/98)的成人脊柱侧凸患者初始状态下(步行前)即表现为矢状面失平衡,表明这些患者的代偿机制一开始就已经无法维持正常的直立姿势。失代偿组患者步行前矢状面躯干偏移为85.6(42.3,135.5)mm,步行后为197.5(148.2,347.3)mm,差异有统计学意义(P < 0.01),表明在步行15 min额外运动的情况下,所有代偿机制逐渐失灵,导致矢状面失平衡明显加重。长时间行走后出现矢状面失平衡虽然对失代偿组患者手术决策的影响较小,但对代偿组患者是否需要接受手术治疗却有很重要的参考价值。
本研究中,步行前矢状面平衡(代偿组)的成人脊柱侧凸患者仅占所有纳入患者的19.4%(19/98),其中78.9%(15/19)的患者在行走15 min后出现矢状面失平衡,这些患者可能在行走前由于代偿机制掩盖了矢状面失平衡,但在额外运动(长时间行走)负荷下骨盆和腰椎伸肌群出现疲劳而逐渐出现矢状面失平衡。然而,代偿组21.1%(4/19)的成人脊柱侧凸患者步行15 min后矢状面仍然保持平衡,这些患者在维持直立平衡的同时,胸椎伸展、骨盆倾斜程度并未发生明显改变。但无论运动多久这部分患者都不会出现矢状面失平衡吗?如果不是,那么他们需要行走多久才能使代偿机制失灵并出现矢状面失平衡?尽管本研究未回答该问题,但仍表明对于矢状面代偿平衡的成人脊柱侧凸患者,静态的影像学检查不能准确地评估其脊柱畸形的动态特点。因此,初始状态下矢状面平衡的成人脊柱侧凸患者需要步行15 min后重新评估其潜在的矢状面不稳定性,这也许可对是否需要采取手术干预提供重要指导。
本研究未纳入与矢状面参数密切相关的生活质量相关评分,但长时间行走后生活质量相关评分降低是矢状面代偿平衡成人脊柱侧凸患者的一个重要特点。既往研究表明,联合应用骨盆倾斜角、骨盆入射角-腰椎前凸角与矢状面躯干偏移3个参数可以预测成人脊柱侧凸患者的功能障碍,从而指导手术决策[14-15]。Smith等[16]研究发现手术矫形可以改善代偿性腰椎前凸患者的生活质量相关评分、疼痛和功能障碍,认为仅依靠矢状面躯干偏移可能会低估矢状面代偿平衡患者的病情,而联合骨盆入射角-腰椎前凸角可以更准确、全面地评估患者病情。但Smith等[16]并未阐明患者在畸形矫正后生活质量相关评分改善的原因,这可能与矫形手术使术前矢状面动态失平衡恢复稳定有关。此外,本研究为回顾性研究,无法对患者到达门诊前参与的活动进行评估或控制,也没有设置无矢状面畸形的对照组。
综上所述,成人脊柱侧凸患者在行走15 min后,骨盆和脊柱伸肌发生疲劳,导致维持躯干矢状面平衡的代偿机制逐渐失灵,从而使大部分患者出现矢状面失平衡或失平衡加重。对于初次就诊时X线片显示矢状面躯干偏移 < 40 mm、骨盆倾斜角>20°的患者,建议在行走15 min后再次拍摄站立位全脊柱正侧位X线片,重新评估患者是否存在潜在的矢状面失平衡,从而为此类患者制定更合理的手术决策。
| [1] |
DUBOUSSET J. Three-dimensional analysis of the scoliotic deformity[M]//WEINSTEID S L. The Pediatric spine: principles and practice. New York: Raven Press, 1994: 479-496.
|
| [2] |
BARREY C, ROUSSOULY P, LE HUEC J C, D'ACUNZI G, PERRIN G. Compensatory mechanisms contributing to keep the sagittal balance of the spine[J]. Eur Spine J, 2013, 22(Suppl 6): S834-S841. |
| [3] |
BUCKLAND A J, VIRA S, OREN J H, LAFAGE R, HARRIS B Y, SPIEGEL M A, et al. When is compensation for lumbar spinal stenosis a clinical sagittal plane deformity?[J]. Spine J, 2016, 16: 971-981. DOI:10.1016/j.spinee.2016.03.047 |
| [4] |
DIEBO B G, FERRERO E, LAFAGE R, CHALLIER V, LIABAUD B, LIU S, et al. Recruitment of compensatory mechanisms in sagittal spinal malalignment is age and regional deformity dependent:a full-standing axis analysis of key radiographical parameters[J]. Spine (Phila Pa 1976), 2015, 40: 642-649. DOI:10.1097/BRS.0000000000000844 |
| [5] |
LAFAGE V, SCHWAB F, SKALLI W, HAWKINSON N, GAGEY P M, ONDRA S, et al. Standing balance and sagittal plane spinal deformity:analysis of spinopelvic and gravity line parameters[J]. Spine (Phila Pa 1976), 2008, 33: 1572-1578. DOI:10.1097/BRS.0b013e31817886a2 |
| [6] |
SCHWAB F, LAFAGE V, PATEL A, FARCY J P. Sagittal plane considerations and the pelvis in the adult patient[J]. Spine (Phila Pa 1976), 2009, 34: 1828-1833. DOI:10.1097/BRS.0b013e3181a13c08 |
| [7] |
OBEID I, HAUGER O, AUNOBLE S, BOURGHLI A, PELLET N, VITAL J M. Global analysis of sagittal spinal alignment in major deformities:correlation between lack of lumbar lordosis and flexion of the knee[J]. Eur Spine J, 2011, 20(Suppl 5): 681-685. |
| [8] |
BARREY C, ROUSSOULY P, PERRIN G, LE HUEC J C. Sagittal balance disorders in severe degenerative spine. Can we identify the compensatory mechanisms?[J]. Eur Spine J, 2011, 20(Suppl 5): 626-633. |
| [9] |
BARREY C, PINHEIRO-FRANCO J L, LE-HUEC J C, PERRIN G, ROUSSOULY P. Compensatory mechanisms contributing to the maintenance of sagittal balance in degenerative diseases of the lumbar spine[M]//PINHEIRO-FRANCO J, VACCARO A, BENZEL E, MAYER H. Advanced concepts in lumbar degenerative disk disease. Heidelberg, Berlin: Springer, 2016: 725-737.
|
| [10] |
LAMARTINA C, BERJANO P. Classification of sagittal imbalance based on spinal alignment and compensatory mechanisms[J]. Eur Spine J, 2014, 23: 1177-1189. DOI:10.1007/s00586-014-3227-9 |
| [11] |
LEGAYE J, DUVAL-BEAUPÈRE G. Sagittal plane alignment of the spine and gravity:a radiological and clinical evaluation[J]. Acta Orthop Belg, 2005, 71: 213-220. |
| [12] |
JACKSON R P, MCMANUS A C. Radiographic analysis of sagittal plane alignment and balance in standing volunteers and patients with low back pain matched for age, sex, and size. A prospective controlled clinical study[J]. Spine (Phila Pa 1976), 1994, 19: 1611-1618. DOI:10.1097/00007632-199407001-00010 |
| [13] |
VAN WINGERDEN J P, VLEEMING A, BUYRUK H M, RAISSADAT K. Stabilization of the sacroiliac joint in vivo:verification of muscular contribution to force closure of the pelvis[J]. Eur Spine J, 2004, 13: 199-205. DOI:10.1007/s00586-003-0575-2 |
| [14] |
VIVEROS P, MARQUEZ A C, BARBERÁ L, ROSSEL J P G. Graphical analysis for operation management:a graphical method to support operation decision making[J]. Qual Reliab Eng Int, 2016, 32: 2299-2311. DOI:10.1002/qre.1936 |
| [15] |
AMES C P, SMITH J S, SCHEER J K, BESS S, BEDERMAN S S, DEVIREN V, et al. Impact of spinopelvic alignment on decision making in deformity surgery in adults:a review[J]. J Neurosurg Spine, 2012, 16: 547-564. DOI:10.3171/2012.2.SPINE11320 |
| [16] |
SMITH J S, SINGH M, KLINEBERG E, SHAFFREY C I, LAFAGE V, SCHWAB F J, et al. Surgical treatment of pathological loss of lumbar lordosis (flatback) in patients with normal sagittal vertical axis achieves similar clinical improvement as surgical treatment of elevated sagittal vertical axis:clinical article[J]. J Neurosurg Spine, 2014, 21: 160-170. DOI:10.3171/2014.3.SPINE13580 |
 2020, Vol. 41
2020, Vol. 41


