由胶原ⅩⅩⅦ α1型(collagen type ⅩⅩⅦ α1 chain,COL27A1)基因突变导致的Steel综合征是一种累及多系统的常染色体隐性遗传病,其临床特征主要有面部畸形、身材矮小、腕骨融合、桡骨头和髋关节脱位、脊柱侧凸、弓形足、颈椎畸形等[1-2]。该病属于新生儿时期即开始发病的罕见遗传病,发病率非常低(<1/100万)[3]。本研究报告了海军军医大学(第二军医大学)长海医院骨科收治的1例汉族Steel综合征合并脊柱侧凸青少年患者资料,同时回顾性分析国外文献报道的COL27A1基因突变所致Steel综合征病例资料,总结Steel综合征新的基因突变位点及临床特征,为Steel综合征的诊治提供参考。
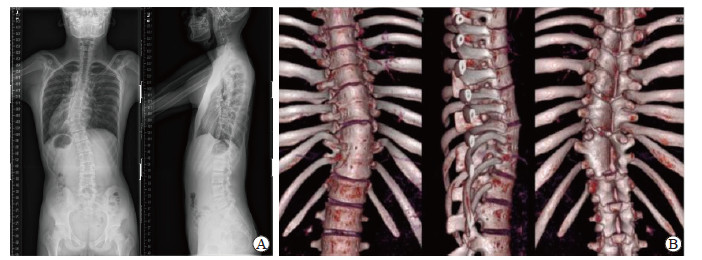
1 资料和方法 1.1 病例资料患者男,14岁,汉族,体重45 kg,身高163 cm,父母为非近亲结婚,母亲足月妊娠经阴道分娩,出生体重为2.8 kg。因“发现脊柱侧凸1年”于2017年9月3日收入海军军医大学(第二军医大学)长海医院骨科。患者1年前于外院诊断为脊柱侧凸后一直采取支具穿戴等保守治疗。自患病以来无肢体麻木、精神障碍、体力减退、食欲食量改变、大小便异常等特殊临床表现。既往无慢性疾病史、传染病史、手术史、外伤史和过敏史。入院体格检查:长椭圆脸,前额突出,鼻前倾,扁平胸,蹼状颈、颈后发际线低,椎体较小、胸椎左侧凸、剃刀背畸形,肘关节外翻,双手小指侧弯(图 1),桡骨头和腕关节脱位,下蹲受限,无异常步态,无骨盆前倾,无肢体缩短,髋关节无内收外展、内旋外旋等畸形,单足站立试验阴性。无头颅发育畸形、皮肤黏膜黄染、皮下结节包块、异常毛发、色素沉着、牛奶咖啡斑等,无听力障碍、言语或运动发育迟缓。骨龄测试显示发育落后。查血常规示白细胞计数6.32×109/L,红细胞计数5.02×1012/L,血红蛋白147 g/L,血小板计数221×109/L;查肝肾功能示总胆红素13.4 μmol/L,白蛋白42 g/L,球蛋白29 g/L,白球比1.45,丙氨酸转氨酶12 U/L,天冬氨酸转氨酶15 U/L,碱性磷酸酶266 U/L,乳酸脱氢酶166 U/L,钠142 mmol/L,钾4.2 mmol/L,葡萄糖5.0 mmol/L,血肌酐53 μmol/L;CRP 3.29 mg/L;红细胞沉降率2 mm/1 h;凝血酶原时间16.6 s,凝血酶原时间国际标准化比值1.3,活化部分凝血活酶时间40.0 s,凝血酶时间23.4 s,纤维蛋白原2.10 g/L,D-二聚体0.22 μg/mL。心电图检查示窦性心律伴不完全性右束支传导阻滞。心脏超声检查示少量心包积液,心脏大小正常,收缩功能正常;阴囊、睾丸、附睾超声检查未见明显异常;腹部超声检查示肝脏、胆囊、胰头体、脾脏、双肾未见明显异常;胸部CT检查示右锁骨下动脉异常,扁平胸,心脏前缘受压;全主动脉CT血管造影检查未见明显异常;全脊柱正侧位X线片检查示脊柱侧凸(图 2A),冠状面Cobb角T5~T12 42°、T12~L4 24°,矢状面Cobb角T5~T12 11°、T10~L2 4°、L1~L5 30°。脊柱CT三维重建示先天性脊柱畸形合并多节段和发育性缺陷、T7~T8和T9~T11阻滞椎(图 2B)。全脊柱MRI检查示脊柱侧凸畸形,C4/5、C5/6椎间盘和L2~S1椎间盘轻度膨出。本研究通过海军军医大学(第二军医大学)长海医院伦理委员会审批,患者家属同意该研究并签署研究知情同意书。

|
图 1 体格检查示患者蹼状颈和颈后发际线低(A)、肘外翻(B)、手指畸形(C) Fig 1 Physical examination showed webbed neck and low hairline (A), cubitus valgus (B) and finger deformity (C) |
|
图 2 全脊柱正侧位X线片和脊柱计算机断层扫描三维重建图像 Fig 2 Full-spine anteroposterior and lateral X-ray radiographs and three-dimensional reconstructed images of spine by computed tomography A: Full-spine anteroposterior and lateral radiographs showed scoliosis; B: Three-dimensional reconstructed images of the spine showed a congenital spinal deformity complicated with multiple segmentation and formation defects (block vertebrae at T7-T8 and T9-T11) |
1.2 文献回顾
利用PubMed数据库以“Steel syndrome”AND“COL27A1”为主题词检索1993年1月至2020年10月相关文献。纳入标准:(1)基因检测结果提示有明确的Steel综合征相关COL27A1突变;(2)有发育迟缓、长椭圆脸、前额突出、鼻前倾、双侧髋关节脱位、髋内翻或双侧髋臼浅、脊柱侧凸等Steel综合征临床特征至少2项。
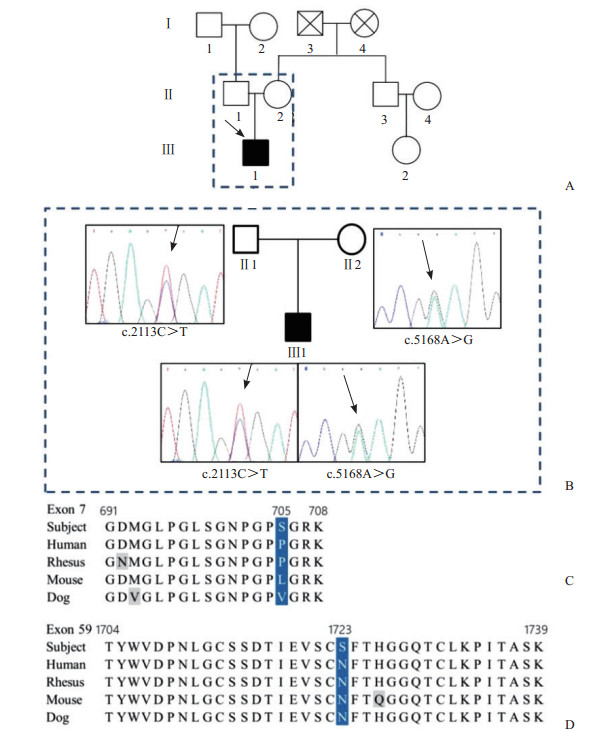
2 结果 2.1 患者家谱图、基因测序结果与治疗 2.1.1 患者家谱图患者为独生子,先证者谱系显示其父亲、母亲、祖父、祖母均无异常表型或相关临床表现(图 3A)。
|
图 3
患者家谱图和全外显子测序结果
Fig 3
Pedigree reconstruction of the family and exome sequencing
A: Pedigree reconstruction of the family (arrow indicates proband); B: Gene capture through high-throughput sequencing chromatograms (arrows indicate mutation sites); C: Exome sequencing showed p.Pro705Ser variant; D: Exome sequencing showed p.Asn1723Ser variant. □ represent normal male; ○ represent normal female; ■ represent the patient;  represent dead male; ⊗ represent dead female. Gray represents nonsense mutation; blue represents mutation site represent dead male; ⊗ represent dead female. Gray represents nonsense mutation; blue represents mutation site |
2.1.2 全外显子测序
采集患者和一级、二级亲属(患者父亲、母亲、祖父、祖母、舅舅)的外周血,用TIANamp血液DNA分离试剂盒(DP318,北京天根生物科技有限公司)提取基因组DNA,使用美国IDT公司捕获探针(xGen® Exome Research Panel)、美国Illumina公司HiSeq4000测序平台进行全外显子测序。目标区捕获高通量测序参数:目标基因数19 396,目标区域长度39 000 000,目标区域覆盖度98.0%,目标区域平均深度141.3,目标区域平均深度>10位点所占比例96.8%。结果显示患者9号染色体COL27A1基因存在2个致病性复合杂合突变,分别位于外显子7[c.2113C>T(p.Pro705Ser)(NM_032888.3,116958281),来源于父亲]和外显子59[c.5168A>G(p.Asn1723Ser)(NM_032888.3,117070009),来源于母亲](图 3B~3D)。
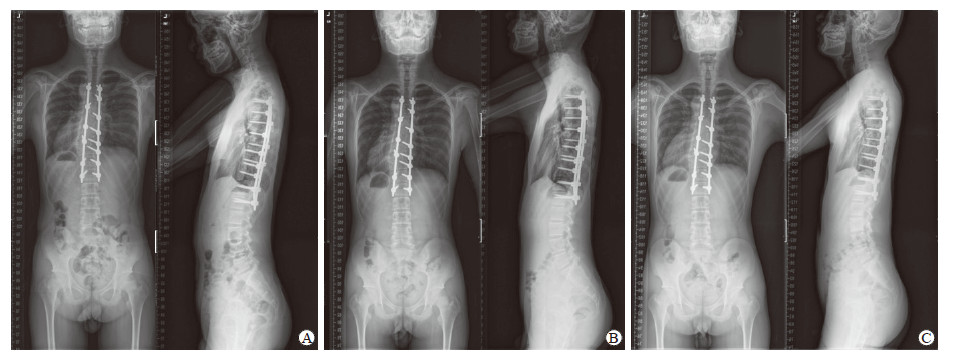
2.1.3 诊断与治疗综合患者临床表现和体征、既往史(无宫内窘迫、无脊髓灰质炎等)、家族史(无神经纤维瘤病等),X线片、CT三维重建(T7~T8和T9~T11阻滞椎)和MRI检查(排除椎管内占位、小脑扁桃体下疝畸形)结果,以及全外显子测序结果,确诊Steel综合征合并先天性脊柱侧凸。于2017年9月13日在全身麻醉下行脊柱侧凸后路三维矫形植骨融合内固定术,手术节段T3~L1,术中失血量约800 mL,采用自体血回输及异体血(红细胞悬液4 U,血浆400 mL)输注,手术时间共3 h 40 min。手术过程顺利,术中神经电生理监测未见异常,生命体征平稳,麻醉清醒后四肢活动良好。患者术后第5天拔除伤口引流管并佩戴支具下地活动,术后第7天复查全脊柱正侧位X线片示内固定位置良好,于2017年9月21日出院。患者术后恢复顺利,切口愈合良好,术后3个月、1年、2年门诊复查全脊柱正侧位X线片(图 4),术后2年全脊柱正侧位X线片示固定节段骨性融合良好,无断钉、断棒、交界性后凸、远端附加现象等并发症。
|
图 4 患者术后全脊柱正侧位X线片 Fig 4 Anteroposterior and lateral X-ray radiographs of full spine of the patient A: Postoperation 3 months; B: Postoperation 1 year; C: Postoperation 2 years |
2.2 文献回溯结果
检索到文献13篇共54例Steel综合征患者,其中波多黎各血统44例、非波多黎各血统10例。最终纳入9篇文献,共有全外显子测序确诊COL27A1突变所致Steel综合征患者17例,包括本例患者共纳入18例,其中3例为复合杂合突变(1例p.Pro705Ser和p.Asn1723Ser、1例c.93del和c.3075del、1例p.Cys174Serfs*34和p.Arg707*),其余均为纯合错义突变(11例p.Gly697Arg、1例p.Gly802Glu、1例p.Gly904Arg、1例c.4261-1G>A、1例c.3556-2A>G)。18例患者中男9例、女9例,确诊年龄为0.17~14岁,11例来自美国波多黎各,印度、阿联酋、也门、伊拉克、叙利亚、塞浦路斯、中国各1例。除1例患者临床特征不详外,余17例患者的临床表现有脊柱侧凸(17例)、身材矮小(12例)、长椭圆脸(9例)、前额突出(9例)、发育迟缓(5例)、听力受损(5例)、胸廓畸形(5例)、语言迟缓(4例)、手指畸形(4例)、宽鼻梁(3例)、肘外翻(3例)、眼距增宽(1例)等;影像学特征有髋关节脱位(16例)、桡骨头脱位(11例)、腕骨融合(9例)、髋关节发育不全(1例)等。见表 1。
|
|
表 1 COL27A1突变所致Steel综合征患者的基本特点 Tab 1 Characteristics of patients with Steel syndrome caused by COL27A1 mutation |
3 讨论
Steel综合征作为一种罕见的常染色体隐性遗传病,其家族史、临床特征、影像学检查等可提供倾向性诊断。与既往报道的17例确诊患者[4-12]相似,本例患者也有发育迟缓、腕骨融合、脊柱侧凸、长椭圆脸、前额突出、鼻前倾等临床特征,还表现为既往尚未报道的蹼状颈和颈后低发际线,但未出现听力障碍、双侧髋关节脱位、髋内翻或双侧髋臼浅等[1-2],而既往报道的17例患者均存在双侧髋关节脱位[4-12]。因此,Steel综合征患者临床特征存在异质性,最终确诊需要依据患者的基因检测结果。
目前COL27A1基因突变已被认为是Steel综合征的致病突变。COL27A1是Pace等[13]在2003年首次报道的新的编码胶原蛋白的基因,其位于第9号染色体,全长约156 000 bp,包含61个外显子。COL27A1基因调控着ⅩⅩⅦ型胶原的生成,参与软骨和其他组织的合成。因此,COL27A1在眼和耳的软骨组织中高表达,而在皮肤、胃、性腺或大脑等其他结缔组织中低表达[14]。ⅩⅩⅦ型胶原是脊椎动物纤维胶原家族中的一类,是构成细胞外基质的主要成分[15-16],在软骨钙化和骨化中起着重要作用[17-18]。Plumb等[19]在纯合子突变COL27A1基因敲除小鼠研究中发现COL27A1蛋白87个氨基酸缺失可导致严重的软骨发育不良。Christiansen等[20]研究发现COL27A1基因敲除斑马鱼在发育早期会出现脊索弯曲畸形,到发育后期则演变成以椎体形态异常为特征的脊柱侧凸。
既往人群筛查结果提示,由于波多黎各人群的奠基者效应,COL27A1基因在该人群中突变率高达2%,而在世界其他人群中此突变极为罕见[9]。波多黎各人群中COL27A1基因p.Gly697Arg突变最为常见[12],其携带率高达1/51[9]。生物化学模型研究表明,COL27A1基因p.Gly697Arg破坏了α1胶原蛋白头端保守的三螺旋结构域,与其他常见的胶原结缔组织疾病(如Ehlers-Danlos综合征和Alport综合征等)的发病机制类似[21]。之后多个国家的学者陆续报道了COL27A1基因其他位点突变所致Steel综合征的不同表型,如印度(p.Cys174Serfs*34和p.Arg707*)[10]、阿联酋(c.3556-2A>G)[11]、也门(c.4261-1G>A,剪接位点)[8]、伊拉克(c.2710G>A)[7]和叙利亚(c.93del,c3075del)[6]。
本例患者是汉族人群中发现的第1例通过全外显子测序确诊并报道的Steel综合征患者,基因测序提示第9号染色体COL27A1基因存在2个致病性复合杂合突变,分别位于外显子7的p.Pro705Ser(来源于父亲)和外显子59的p.Asn1723Ser(来源于母亲)。这与之前报道的突变位点并不一致,且千人基因组计划、外显子组整合数据库(Exome Aggregation Consortium,ExAC)、Exome Variant Server和内部数据库中均未见报道。Sanger测序结果显示p.Pro705Ser也存在于患者的祖母和父亲,但通过与突变数据库和ExAC进行比对分析认为该变异是无义替换突变。对患者母亲存在的p.Asn1723Ser进行进化保守性分析,结果显示其处于进化保守性最高的位置。本例患者的基因突变位点导致的具体功能改变尚待研究。
目前,对于综合征性脊柱畸形的诊断方法包括临床表型诊断、影像诊断、染色体诊断、基因诊断及肌肉活检诊断[22]。在本例患者的诊疗过程中,外院拍摄全脊柱正侧位X线片提示脊柱侧凸,Cobb角为20°~40°(具体不详),未见明显半椎体,先按照特发性脊柱侧凸采用保守支具治疗。1年后因自觉脊柱畸形保守治疗效果不佳、进展较快,来我院复诊,建议进一步检查脊柱CT并行三维重建。结果提示椎体分节不全和椎体形成障碍(T7~T8和T9~T11阻滞椎),结合患者发育迟缓、蹼状颈和颈后低发际线等外貌特征与肘外翻、手指畸形等临床特征,考虑Steel综合征合并先天性脊柱畸形。其临床体征鉴别诊断包括Larsen综合征、Ehlers-Danlos综合征、Turner综合征、Klippel-Feil综合征等。Larsen综合征为全身结缔组织发育障碍,常存在全身多部位关节先天性脱位、脊柱侧凸及前额突出、眼距较宽、颜面扁平、鼻梁塌陷等面部畸形,几乎所有患者均存在膝关节脱位[1, 23-24]。Ehlers-Danlos综合征属于遗传性结构蛋白病,可表现为皮肤弹性增大和前额、眼距、鼻梁较宽的特殊面容,累及骨关节系统可表现为关节过度活动、脊柱畸形等[25-26]。Turner综合征是雌性个体X染色体完全或部分缺失所致的疾病,临床表现为身材矮小、脊柱侧凸、肘外翻、蹼状颈、颈后低发际线、听力受损等[27-29]。Klippel-Feil综合征又称先天性颈椎融合畸形,颈部活动受限、短颈和颈后低发际线为其三大临床特征,部分患者可有脊柱侧凸、听力障碍和其他脏器系统畸形[30-31]。根据本例患者临床表现鉴别诊断较难,建议患者取全血行外显子测序,结果提示COL27A1基因突变,确诊为Steel综合征。
对于Steel综合征的手术治疗目前存在争议,不仅限于脊柱畸形,还包括髋关节脱位等,可能与患者的特殊体质相关。对于Steel综合征的治疗和预后,Flynn等[1]研究发现,61%合并髋关节脱位的Steel综合征患者接受复位治疗后疼痛主诉更多且日常活动更受限制,因此不建议Steel综合征合并髋关节脱位患者行关节复位治疗,而合并桡骨头脱位的Steel综合征患者行桡骨头切除不仅可改善外观而且对运功和功能无明显影响;97%合并腕骨融合的患者无明显运动或功能受限,无须临床干预;53%的Steel综合征患者合并脊柱侧凸,其中1例先天性脊柱侧凸及31%的非先天性脊柱侧凸患者接受了后路矫形自体骨移植融合内固定术,非先天性脊柱侧凸的融合节段选择参照特发性脊柱侧凸,术后随访效果良好,未发现近、远期并发症;10%的Steel综合征患者合并颈椎畸形,但仅1例寰枢关节半脱位患者接受了手术固定;34%的Steel综合征患者合并弓形足,长期随访未发现足踝症状相关主诉。本例患者需手术干预的骨科相关畸形主要为先天性脊柱侧凸(T7~T8和T9~T11阻滞椎),选择行T3~L1的后路矫形植骨融合内固定术,术中无异常出血、置钉失败、硬脊膜破裂、脊髓监测信号异常,术后恢复顺利,2年随访未见内固定失败、畸形进展等并发症。
Steel综合征较为罕见,随着全世界报道病例的逐渐增多,相信未来对这一疾病的认识会更加深入,加之成熟的辅助技术,患者预后将会得到明显改善。
| [1] |
FLYNN J M, RAMIREZ N, BETZ R, MULCAHEY M J, PINO F, HERRERA-SOTO J A, et al. Steel syndrome:dislocated hips and radial heads, carpal coalition, scoliosis, short stature, and characteristic facial features[J]. J Pediatr Orthop, 2010, 30: 282-288. DOI:10.1097/BPO.0b013e3181d3e464 |
| [2] |
STEEL H H, PISTON R W, CLANCY M, BETZ R R. A syndrome of dislocated hips and radial heads, carpal coalition, and short stature in Puerto Rican children[J]. J Bone Joint Surg Am, 1993, 75: 259-264. DOI:10.2106/00004623-199302000-00013 |
| [3] |
Steel syndrome[EB/OL]. (2020-10-30)[2020-10-31].https://www.orpha.net/consor/cgi-bin/Disease_Search.php?lng=EN&data_id=23364&Disease_Disease_Search_diseaseGroup=steel-syndrome&Disease_Disease_Search_diseaseType=Pat&Disease(s)/group%20of%20diseases=Steel-syndrome&title=Steel%20syndrome&search=Disease_Search_Simple.
|
| [4] |
AMLIE-WOLF L, MOYER-HARASINK S, CARR A M, GIAMPIETRO P, SCHNEIDER A, SIMON M. Three new patients with Steel syndrome and a Puerto Rican specific COL27A1 mutation[J]. Am J Med Genet A, 2020, 182: 798-803. DOI:10.1002/ajmg.a.61465 |
| [5] |
KRITIOTI E, THEODOSIOU A, NICOLAOU N, ALEXANDROU A, PAPAEVRIPIDOU I, EFSTATHIOU E, et al. First reported case of Steel syndrome in the European population: a novel homozygous mutation in COL27A1 and review of the literature[J/OL]. Eur J Med Genet, 2020, 63: 103939. doi: 10.1016/j.ejmg.2020.103939.
|
| [6] |
PÖLSLER L, SCHATZ U A, SIMMA B, ZSCHOCKE J, RUDNIK-SCHÖNEBORN S. A Syrian patient with Steel syndrome due to compound heterozygous COL27A1 mutations with colobomata of the eye[J]. Am J Med Genet A, 2020, 182: 730-734. DOI:10.1002/ajmg.a.61478 |
| [7] |
THURESSON A C, SOUSSI ZANDER C, ZHAO J J, HALVARDSON J, MAQBOOL K, MÅNSSON E, et al. Whole genome sequencing of consanguineous families reveals novel pathogenic variants in intellectual disability[J]. Clin Genet, 2019, 95: 436-439. DOI:10.1111/cge.13470 |
| [8] |
MADDIREVULA S, ALZAHRANI F, AL-OWAIN M, AL MUHAIZEA M A, KAYYALI H R, ALHASHEM A, et al. Autozygome and high throughput confirmation of disease genes candidacy[J]. Genet Med, 2019, 21: 736-742. DOI:10.1038/s41436-018-0138-x |
| [9] |
BELBIN G M, ODGIS J, SOROKIN E P, YEE M C, KOHLI S, GLICKSBERG B S, et al. Genetic identification of a common collagen disease in Puerto Ricans via identity-by-descent mapping in a health system[J/OL]. Elife, 2017, 6: e25060. doi: 10.7554/eLife.25060.
|
| [10] |
KOTABAGI S, SHAH H, SHUKLA A, GIRISHA K M. Second family provides further evidence for causation of Steel syndrome by biallelic mutations in COL27A1[J]. Clin Genet, 2017, 92: 323-326. DOI:10.1111/cge.13006 |
| [11] |
GARIBALLA N, BEN-MAHMOUD A, KOMARA M, AL-SHAMSI A M, JOHN A, ALI B R, et al. A novel aberrant splice site mutation in COL27A1 is responsible for Steel syndrome and extension of the phenotype to include hearing loss[J]. Am J Med Genet A, 2017, 173: 1257-1263. DOI:10.1002/ajmg.a.38153 |
| [12] |
GONZAGA-JAUREGUI C, GAMBLE C N, YUAN B, PENNEY S, JHANGIANI S, MUZNY D M, et al. Mutations in COL27A1 cause Steel syndrome and suggest a founder mutation effect in the Puerto Rican population[J]. Eur J Hum Genet, 2015, 23: 342-346. DOI:10.1038/ejhg.2014.107 |
| [13] |
PACE J M, CORRADO M, MISSERO C, BYERS P H. Identification, characterization and expression analysis of a new fibrillar collagen gene, COL27A1[J]. Matrix Biol, 2003, 22: 3-14. DOI:10.1016/S0945-053X(03)00007-6 |
| [14] |
PLUMB D A, DHIR V, MIRONOV A, FERRARA L, POULSOM R, KADLER K E, et al. Collagen ⅩⅩⅦ is developmentally regulated and forms thin fibrillar structures distinct from those of classical vertebrate fibrillar collagens[J]. J Biol Chem, 2007, 282: 12791-12795. DOI:10.1074/jbc.C700021200 |
| [15] |
BOOT-HANDFORD R P, TUCKWELL D S, PLUMB D A, ROCK C F, POULSOM R. A novel and highly conserved collagen (proα1(ⅩⅩⅦ)) with a unique expression pattern and unusual molecular characteristics establishes a new clade within the vertebrate fibrillar collagen family[J]. J Biol Chem, 2003, 278: 31067-31077. DOI:10.1074/jbc.M212889200 |
| [16] |
WADA H, OKUYAMA M, SATOH N, ZHANG S. Molecular evolution of fibrillar collagen in chordates, with implications for the evolution of vertebrate skeletons and chordate phylogeny[J]. Evol Dev, 2006, 8: 370-377. DOI:10.1111/j.1525-142X.2006.00109.x |
| [17] |
HJORTEN R, HANSEN U, UNDERWOOD R A, TELFER H E, FERNANDES R J, KRAKOW D, et al. Type ⅩⅩⅦ collagen at the transition of cartilage to bone during skeletogenesis[J]. Bone, 2007, 41: 535-542. DOI:10.1016/j.bone.2007.06.024 |
| [18] |
MAYO J L, HOLDEN D N, BARROW J R, BRIDGEWATER L C. The transcription factor Lc-Maf participates in Col27a1 regulation during chondrocyte maturation[J]. Exp Cell Res, 2009, 315: 2293-2300. DOI:10.1016/j.yexcr.2009.04.020 |
| [19] |
PLUMB D A, FERRARA L, TORBICA T, KNOWLES L, MIRONOV A Jr, KADLER K E, et al. Collagen ⅩⅩⅦ organises the pericellular matrix in the growth plate[J/OL]. PLoS One, 2011, 6: e29422. doi: 10.1371/journal.pone.0029422.
|
| [20] |
CHRISTIANSEN H E, LANG M R, PACE J M, PARICHY D M. Critical early roles for col27a1a and col27a1b in zebrafish notochord morphogenesis, vertebral mineralization and post-embryonic axial growth[J/OL]. PLoS One, 2009, 4: e8481. doi: 10.1371/journal.pone.0008481.
|
| [21] |
PERSIKOV A V, PILLITTERI R J, AMIN P, SCHWARZE U, BYERS P H, BRODSKY B. Stability related bias in residues replacing glycines within the collagen triple helix (Gly-Xaa-Yaa) in inherited connective tissue disorders[J]. Hum Mutat, 2004, 24: 330-337. DOI:10.1002/humu.20091 |
| [22] |
钱邦平, 邱勇. 综合征性脊柱畸形的挑战与对策[J]. 中国脊柱脊髓杂志, 2017, 27: 481-483. DOI:10.3969/j.issn.1004-406X.2017.06.01 |
| [23] |
HOSOE H, MIYAMOTO K, WADA E, SHIMIZU K. Surgical treatment of scoliosis in larsen syndrome with bilateral hip dislocation[J/OL]. Spine (Phila Pa 1976), 2006, 31: E302-E306. doi: 10.1097/01.brs.0000216447.42297.17.
|
| [24] |
SAJNANI A K, YIU C K, KING N M. Larsen syndrome:a review of the literature and case report[J]. Spec Care Dentist, 2010, 30: 255-260. DOI:10.1111/j.1754-4505.2010.00163.x |
| [25] |
薛旭红, 沈建雄. Ehlers-Danlos综合征[J]. 脊柱外科杂志, 2013, 11: 378-381. DOI:10.3969/j.issn.1672-2957.2013.06.014 |
| [26] |
PARAPIA L A, JACKSON C. Ehlers-Danlos syndrome-a historical review[J]. Br J Haematol, 2008, 141: 32-35. DOI:10.1111/j.1365-2141.2008.06994.x |
| [27] |
TURNER H H. A syndrome of infantilism, congenital webbed neck, and cubitus valgus[J]. Endocrinology, 1938, 23: 566-574. DOI:10.1210/endo-23-5-566 |
| [28] |
KIM J Y, ROSENFELD S R, KEYAK J H. Increased prevalence of scoliosis in Turner syndrome[J]. J Pediatr Orthop, 2001, 21: 765-766. |
| [29] |
DAY G, SZVETKO A, GRIFFITHS L, MCPHEE I B, TUFFLEY J, LABROM R, et al. SHOX gene is expressed in vertebral body growth plates in idiopathic and congenital scoliosis:implications for the etiology of scoliosis in Turner syndrome[J]. J Orthop Res, 2009, 27: 807-813. DOI:10.1002/jor.20801 |
| [30] |
刘洋, 李明. Klippel-Feil综合征研究进展[J]. 脊柱外科杂志, 2005, 3: 43-46. DOI:10.3969/j.issn.1672-2957.2005.01.014 |
| [31] |
XUE X, SHEN J, ZHANG J, TIAN Y, ZHAO H, WANG Y, et al. Klippel-Feil syndrome in congenital scoliosis[J/OL]. Spine (Phila Pa 1976), 2014, 39: E1353-E1358. doi: 10.1097/BRS.0000000000000587.
|
 2020, Vol. 41
2020, Vol. 41


