硬脑膜动静脉瘘(dural arteriovenous fistula,DAVF)是发生在颅内硬脑膜及其附属结构上的动静脉短路,可由多种因素引起,包括创伤、肿瘤、炎症、静脉窦血栓、先天性或后天性静脉窦结构异常等[1-3]。脑膜中动脉(middle meningeal artery,MMA)与脑膜中静脉(middle meningeal vein,MMV)伴行,且MMV在部分患者呈静脉窦样改变,易因外伤等原因发生脑膜中动静脉短路,形成脑膜中静脉硬脑膜动静脉瘘(middle meningeal vein dural arteriovenous fistula,MMV-DAVF),后者是DAVF较少见的一种类型[1, 4]。MMV-DAVF发病率低,其与颅脑损伤的关系、临床表现、结构特征和治疗转归等尚不完全清楚。本研究回顾性总结了我院治疗的MMV-DAVF病例资料,并对文献报道的MMV-DAVF病例进行汇总分析。
1 资料和方法 1.1 病例选择回顾性收集海军军医大学(第二军医大学)长海医院DAVF数据库中1999年1月至2020年4月收治的MMV-DAVF患者资料,包括人口统计学、临床、治疗和随访资料。采用中文主题词“脑膜中静脉”和“脑膜中动脉”和“硬脑膜动静脉瘘”在中国知网、万方数据库、维普数据库、中国生物医学文献数据库和中文生物医学期刊数据库,和以英文主题词“middle meningeal vein”和“middle meningeal artery”和“dural arteriovenous fistula”在PubMed数据库中检索1960年1月1日至2020年8月30日的中英文文献,并对文献的参考资料进一步检索,以纳入更多的MMV-DAVF病例。MMV-DAVF病例纳入标准:(1)明确行数字减影血管造影(digital subtraction angiography,DSA)检查并诊断为DAVF;(2)文献报道中有明确的引流静脉名称,且其引流静脉首先经过MMV。
1.2 统计学处理应用SPSS 21.0软件进行数据处理,计量资料以x±s表示,计数资料以例数和百分数表示。
2 结果 2.1 我院9例MMV-DAVF患者资料分析1999年1月至2020年4月我院诊治的734例DAVF患者中MMV-DAVF患者共9例(1.2%),患者临床资料见表 1。
|
|
表 1 我院9例脑膜中静脉硬脑膜动静脉瘘患者临床资料 |
我院9例患者中男7例、女2例,年龄为29~71岁,平均年龄为(47±15)岁,其中30~50岁患者5例。7例患者有明确的头部外伤史。临床表现包括头痛(5例)、颅内杂音(5例)、眼球运动受限(2例)等。6例患者DSA检查前有CT检查资料,4例CT检查提示合并颅骨骨折,其中2例为颞骨骨折;5例伴有颅内血肿,其中3例有蛛网膜下腔出血。9例患者供血动脉均为MMA,引流静脉均包括MMV,引流方向包括上矢状窦(3例)、海绵窦(2例)、翼丛(2例)、眼上静脉(2例)等。9例患者均接受经MMA入路注射Onyx-18胶血管内栓塞治疗,其中7例患者术后即刻瘘口完全栓塞,2例次全栓塞。9例患者均未发生手术相关并发症,术后无新发神经功能缺损。4例患者完成术后半年的影像学随访,未见DAVF复发和新发。
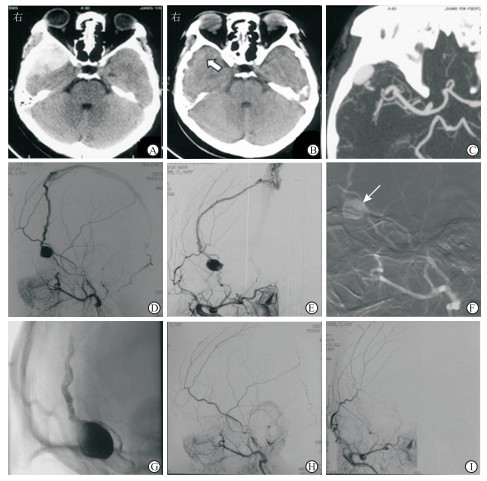
2.2 我院典型病例患者女,45岁,因“头外伤后30 d,右侧颞部颅内搏动性杂音2周”入住我院。患者外伤后2 d于外院就诊,头颅CT检查示右侧颞部硬脑膜外血肿,予保守治疗,外伤3周后复查头颅CT显示血肿吸收、颞极类圆形占位,计算机断层扫描血管造影检查提示颞极动脉瘤样结构。为求进一步诊治入住我院,入院体格检查:右侧颞部闻及颅内搏动性杂音。DSA检查示右侧MMV-DAVF,供血动脉为增粗的右侧MMA,MMA末端形成假性动脉瘤,引流静脉主要为扩张的右侧MMV,并向上矢状窦引流。采用经MMA入路注射Onyx-18胶完全栓塞瘘口、引流静脉和假性动脉瘤。术后颞部颅内搏动性杂音消失,无新发神经系统阳性体征,术后2 d出院。见图 1。
|
图 1 1例45岁女性脑膜中静脉硬脑膜动静脉瘘患者影像学资料 A:外伤后第2天头颅CT检查提示右侧颞部硬脑膜外血肿;B,C:外伤后3周复查头颅CT示血肿吸收、颞极类圆形占位(B,箭头所示),CTA示颞极动脉瘤样结构(C);D,E:右侧颈外动脉侧位、正位DSA示脑膜中静脉硬脑膜动静脉瘘,脑膜中动脉远端假性动脉瘤;F:局部麻醉下行栓塞治疗,微导管头端(箭头所示)尽可能接近静脉端;G:注射Onyx-18胶完全栓塞瘘口、引流静脉和假性动脉瘤;H,I:颈外动脉侧位、正位DSA示瘘口消失.CT:计算机断层扫描;CTA:计算机断层扫描血管造影;DSA:数字减影血管造影 |
2.3 文献报道与我院共32例MMV-DAVF患者资料汇总分析
共纳入16篇文献23例MMV-DAVF患者,患者临床资料见表 2。
|
|
表 2 文献报道的23例脑膜中静脉硬脑膜动静脉瘘患者临床资料 |
汇总分析文献报道和我院共32例MMV-DAVF患者资料,男22例(68.8%)、女10例(31.2%);除1例儿童年龄不详外,其余31例患者年龄为18~78岁,平均年龄为(45±18)岁。32例MMV-DAVF患者临床症状包括头痛(16例,50.0%)、颅内杂音(12例,37.5%)、眼球运动受限(2例,6.2%)、眼球突出(3例,9.4%)、癫痫(1例,3.1%)等。26例(81.2%)患者有明确的头部外伤史。25例患者有CT检查资料,其中合并颅骨骨折21例(84.0%),共计27处骨折(我院1例合并颞骨、额骨骨折;文献报道1例合并蝶骨、颞骨和枕骨骨折,1例合并顶骨、颞骨骨折,1例合并枕骨、颞骨骨折,1例合并额骨、颞骨骨折)。颞骨骨折15处(55.6%,15/27),眼眶外侧壁骨折1处(3.7%,1/27),额骨骨折3处(11.1%,3/27),顶骨骨折2处(7.4%,2/27),枕骨骨折2处(7.4%,2/27),蝶骨骨折3处(11.1%,3/27),1处(3.7%,1/27)骨折位置不明。16例(64.0%,16/25)伴有颅内血肿,包括7例(28.0%,7/25)伴有蛛网膜下腔出血。
32例患者供血动脉均为MMA,引流静脉均包括MMV,引流方向包括上矢状窦(8例,25.0%)、海绵窦(7例,21.9%)、翼丛(9例,28.1%)、蝶顶窦(2例,6.2%)、眼上静脉(3例,9.4%)、皮质静脉(1例,3.1%)、基底丛(1例,3.1%)等。
共9例(28.1%)患者接受开放外科手术治疗,均为1982年及之前报道的病例;20例(62.5%)患者采用动脉入路血管内治疗,均为1982年之后的病例。9例行开放手术治疗的患者中,3例术后出现较严重的神经功能障碍。20例行介入栓塞治疗的患者中,16例(80.0%)术后即刻瘘口完全栓塞,2例(10.0%)次全栓塞;该20例患者均无新发神经功能缺损,其中7例有术后半年影像学随访资料,均未出现DAVF复发和新发。另有3例患者(9.4%)瘘口流量小,经保守治疗后自发愈合。
3 讨论MMA起自上颌动脉第一段,经棘孔进入颅腔。MMV成对伴行MMA主干和分支[2],有时会形成硬脑膜内静脉窦,MMA走行于该窦内。颅骨内表面这些血管走行位置存在沟槽,即中脑膜沟,该部位骨折容易引起MMV-DAVF[4, 6]。大部分MMV-DAVF患者有头部外伤史,骨折多发生在颞骨,并且骨折线多经过中脑膜沟的位置[4]。从我院和文献报道病例汇总分析情况来看,创伤性MMV-DAVF一般伴有颅内血肿,特别是硬脑膜外血肿[4]。然而MMV-DAVF并不常见,原因是MMA和MMV被翼外侧肌和颞肌围绕,不易被外界破坏而形成外伤性DAVF[1, 9]。
MMV-DAVF患者的临床症状取决于血流速度,可发生在创伤后几分钟至几个月内,头痛、颅内搏动性杂音是最常见的临床表现[1-2, 14]。MMV-DAVF患者预后一般和外伤程度、外伤位置、MMA和MMV损伤程度有关[4, 14]。当头部外伤不严重、血管损伤较轻时,DAVF可自发愈合,患者预后较好[2, 4, 12]。Wilson等[12]报道的2例创伤性MMV-DAVF患者临床表现均为头痛,其中1例有轻度头部外伤史的患者头部X线片和CT检查见细小的骨折线,DSA示左侧MMV-DAVF,该患者选择保守治疗,3个月后复查DSA未见复发,症状好转。对于血液流量较大的MMV-DAVF,需要积极治疗。
外科切除是治疗MMV-DAVF的传统方法,包括结扎颈外动脉、结扎MMA、切除DAVF与其附近的硬脑膜等手术方案[4, 6]。切除DAVF与其附近的硬脑膜可以彻底消除DAVF[4]。结扎供血动脉有时只能暂时消除DAVF瘘口,侧支循环可能迅速发展导致瘘管再通[4]。文献报道的接受外科手术治疗的9例患者术后瘘口均消失。外科手术的并发症不容忽视,Freckmann等[14]报道的3例行外科手术治疗MMV-DAVF患者,术后均发生严重的神经功能障碍。
MMV-DAVF治疗的核心是瘘口阻断,介入治疗是该病变最安全的治疗手段。汇总分析文献报道和我院接受血管内治疗的20例患者资料,其中16例术后即刻瘘口完全栓塞,我院9例患者中7例术后即刻瘘口完全栓塞,该20例患者均未发生手术相关并发症。闭塞MMV-DAVF的前提是充分认识瘘口结构,术中应完全闭塞瘘口和静脉起始端。对于MMV-DAVF,MMA通常是最直接的栓塞入路,由于瘘口通常位于颞部,该处近端的MMA较为平直,易于微导管超选。此外,选择合适的栓塞材料是瘘口完全闭塞的关键,Onyx-18胶等液体栓塞材料具有良好的弥散性,且在术中可以反复调整弥散方向沿压力梯度持续推送,有利于完全闭塞DAVF;但是,由于MMV-DAVF患者MMA与眼动脉之间存在危险吻合,在推注Onyx-18胶的过程中要特别注意Onyx-18胶的弥散方向,防止造成视网膜中央动脉的意外栓塞。
总之,MMV-DAVF发病率低,患者多有外伤史,常合并颅骨骨折和颅内血肿,经MMA入路栓塞治疗有较高的安全性和有效性。
| [1] |
KIM H S, SONG J H, OH J K, AHN J H, KIM J H, CHANG I B. Endovascular treatment of traumatic arteriovenous fistula in young adults with pulsatile tinnitus[J]. J Korean Neurosurg Soc, 2020, 63: 532-538. DOI:10.3340/jkns.2019.0233 |
| [2] |
CHANDRASHEKAR H S, NAGARAJAN K, SRIKANTH S G, JAYAKUMAR P N, VASUDEV M K, PANDEY P. Middle meningeal arteriovenous fistula and its spontaneous closure. A case report and review of the literature[J]. Interv Neuroradiol, 2007, 13: 173-178. DOI:10.1177/159101990701300208 |
| [3] |
TERADA T, NAKAI E, TSUMOTO T, ITAKURA T. Iatrogenic arteriovenous fistula of the middle meningeal artery caused during embolization for meningioma-case report[J]. Neurol Med Chir (Tokyo), 1997, 37: 677-680. DOI:10.2176/nmc.37.677 |
| [4] |
KITAHARA T, SHIRAI S, OWADA T, MAKI Y. Traumatic middle meningeal arteriovenous fistula. Report of 3 cases and analysis of 32 cases[J]. Eur Neurol, 1977, 16: 136-143. DOI:10.1159/000114891 |
| [5] |
SATOH T, SAKURAI M, YAMAMOTO Y, ASARI S. [An interesting case of the traumatic middle meningeal arteriovenous fistula][J]. No Shinkei Geka, 1982, 10: 739-745. |
| [6] |
KOMIYAMA M, YASUI T, TAMURA K, NAGATA Y, FU Y, YAGURA H. Chronic subdural hematoma associated with middle meningeal arteriovenous fistula treated by a combination of embolization and burr hole drainage[J]. Surg Neurol, 1994, 42: 316-319. DOI:10.1016/0090-3019(94)90400-6 |
| [7] |
TAKEUCHI S, TAKASATO Y, MASAOKA H, HAYAKAWA T, OTANI N, YOSHINO Y, et al. [A case of traumatic middle meningeal arteriovenous fistula on the side of the head opposite to the injured side][J]. No Shinkei Geka, 2009, 37: 983-986. |
| [8] |
SHIM J H, YOON S M, SHIM J J, KIM R S. A case of intraosseous dural arteriovenous fistulas involving diploic vein treated with transarterial onyx embolization[J]. J Korean Neurosurg Soc, 2011, 50: 260-263. DOI:10.3340/jkns.2011.50.3.260 |
| [9] |
KIM S W, CHAE K S, SHIM J H, RHO S J, CHOI H K, PARK H S. Iatrogenic dural arteriovenous fistula after superficial temporal artery to middle cerebral artery anastomosis:a case report[J]. Korean J Neurotrauma, 2015, 11: 151-153. DOI:10.13004/kjnt.2015.11.2.151 |
| [10] |
MARTINEZ M, PERGAMI P, MURNICK J, PEARL M S. Embolization of a traumatic arteriovenous fistula between the middle meningeal artery and middle meningeal vein in a child with pulsatile tinnitus[J]. Childs Nerv Syst, 2018, 34: 571-575. DOI:10.1007/s00381-017-3665-x |
| [11] |
KO J H, KIM Y J. Traumatic pseudoaneurysm of the middle meningeal artery with an arteriovenous fistula on a non-fractured site[J]. Interv Neuroradiol, 2014, 20: 352-356. DOI:10.15274/INR-2014-10025 |
| [12] |
WILSON C B, CRONIC F. Traumatic arteriovenous fistulas involving middle meningeal vessels[J]. JAMA, 1964, 188: 953-957. |
| [13] |
HANDA J, SHIMIZU Y, SATO K, HANDA H. Traumatic aneurysm and arteriovenous fistula of the middle meningeal artery[J]. Clin Radiol, 1970, 21: 39-41. DOI:10.1016/S0009-9260(70)80137-4 |
| [14] |
FRECKMANN N, SARTOR K, HERRMANN H D. Traumatic arteriovenous fistulae of the middle meningeal artery and neighbouring veins or dural sinuses[J]. Acta Neurochir (Wien), 1981, 55: 273-281. DOI:10.1007/BF01808443 |
| [15] |
ROSKI R A, OWEN M, WHITE R J, TAKAOKA Y, BELLON E M. Middle meningeal artery trauma[J]. Surg Neurol, 1982, 17: 200-203. DOI:10.1016/0090-3019(82)90280-4 |
| [16] |
NAKAMURA K, TSUGANE R, ITO H, OBATA H, NARITA H. Traumatic arterio-venous fistula of the middle meningeal vessels[J]. J Neurosurg, 1966, 25: 424-429. DOI:10.3171/jns.1966.25.4.0424 |
 2020, Vol. 41
2020, Vol. 41


