2. 解放军904医院超声科, 苏州 215007
2. Department of Ultrasound, No. 904 Hospital of PLA, Suzhou 215007, Jiangsu, China
镜面伪像(mirror artifact)是超声成像时固有的虚假影像之一,多见于横膈的胸腔侧,源于横膈对超声波的镜面反射(mirror reflection),通常是肝、脾内的实像在横膈以上的肺声像位置上形成虚像,对超声诊断造成明显干扰[1]。气管壁呈开口朝后的“C”字形状,形状上缺乏横膈这种易形成镜面反射的条件,一般情况下其毗邻器官如甲状腺较少发生气管镜面反射伪像。然而,我们发现在超声引导下甲状腺结节热消融治疗围手术期的超声影像中,气管壁镜面反射形成的伪像却并不少见,它不仅干扰术者对甲状腺结节消融术前和术后病情的判断,也会令术者对消融术中操作安全性产生误判,因此有必要对气管壁镜面反射伪像的声像图表现、成因和鉴别进行剖析。
1 资料和方法 1.1 一般资料对2018年1月至2018年10月在上海国际医学中心接受甲状腺结节微波消融治疗的304例患者的超声影像资料进行分析。男59例、女245例,年龄为13~81(41.98±11.93)岁,甲状腺乳头状癌患者144例、甲状腺良性结节患者160例。本研究经上海国际医学中心伦理委员会审批,所有患者均签署知情同意书。
1.2 气管壁镜面伪像的判断标准(1)消融术前、术中、术后位于甲状腺峡部水平的甲状腺结节或邻近气管的甲状腺两侧腺叶结节,在气管腔声像位置上出现符合镜面反射条件的虚像[2];(2)消融术中,穿刺针针尖在气管腔声像位置上出现符合镜面反射条件的虚像。
1.3 液体隔离法与消融方法超声仪采用中国MINDRAY Resona 7S型彩色多普勒超声仪(高频探头L14-5WU,中心频率为9.0 MHz)、日本日立HI VISION Preirus型彩色多普勒超声仪(探头频率为7~14 MHz)。微波消融采用南京维京九洲医疗器械研发中心MTC-3型微波消融仪和MTC-3CA-Ⅲ型消融针。常规体位消毒、铺巾,于颈部皮肤穿刺点、皮下穿刺路径、甲状腺周围间隙均以1%利多卡因溶液实施局部麻醉。根据结节所处位置,按需要在超声实时引导下向结节最邻近的甲状腺周围间隙内注射生理盐水或透明质酸钠凝胶,实现甲状腺与相邻结构的空间隔离[3-4]。之后在超声引导下向靶结节内置入微波消融针,进行由远及近、由深及浅、固定式或移动式消融。微波输出功率为20~35 W,术中超声造影提示消融区血液灌注完全消失时结束治疗。动态录像消融全过程。
1.4 消融后随访消融术后第1、3、6、12个月为随访节点,每次均实施以超声检查为核心的综合随访方案。对术后出现的气管壁镜面伪像进行各时间节点的连续动态比较。
1.5 影像学资料分析围绕镜面伪像对消融术前决策、术中安全性判断、术后疗效评判的影响,回顾患者的消融术前讨论、术中记录及术后随访报告。调阅患者的消融术前、术中、术后超声检查资料,记录镜面伪像的发生率、发生部位及其声像学表现。分析出现镜面伪像时大界面的形态,并与无镜面伪像时进行比较。
2 结果 2.1 气管壁镜面伪像的发生率与构成304例患者的消融术前、术中及术后随访各节点超声影像中共169例(55.59%)出现气管壁镜面伪像,以消融术中出现镜面伪像者最多(149例,88.17%)。镜面伪像来源包括甲状腺结节伪像20例(11.83%)、隔离液注射针伪像133例(78.70%)、微波消融针伪像16例(9.47%)、液体隔离带伪像137例(81.07%)、甲状腺消融区伪像8例(4.73%)。
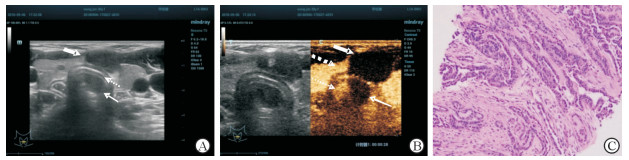
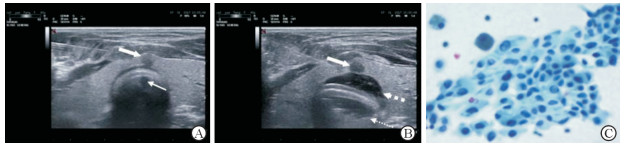
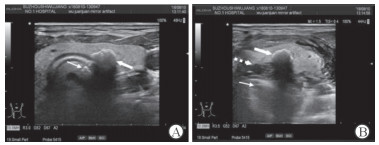
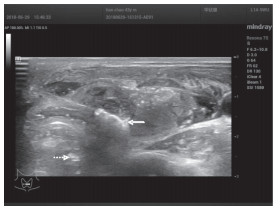
2.2 消融术前气管壁镜面伪像消融术前共12例(7.1%)患者出现气管壁镜面伪像,均为气管旁的甲状腺结节,位于峡部的乳头状癌11例,近峡部粗大钙化灶1例。峡部乳头状癌的镜面伪像貌似肿瘤已浸润至气管腔内(图 1、2),峡部粗大钙化的镜面伪像貌似气管壁内表面发生钙化(图 3)。对此,术者均曾计划放弃消融治疗,后经液体隔离法发现实为伪像而继续实施消融。
|
图 1 甲状腺峡部乳头状癌及其气管壁镜面伪像 Fig 1 An isthmic papillary thyroid carcinoma lesion and its mirror artifact across the trachea A: An isthmic hypoechoic lesion (indicated by a bold solid arrow) compressed trachea, causing segmental flatting of the anterior tracheal wall (indicated by a thin dashed arrow). A well-defined hypoechoic artifact similar in configuration to but smaller in size than the true image developed at the area representing tracheal cavity (indicated by a thin solid arrow). B: The true image of papillary thyroid carcinoma lesion (indicated by a bold solid arrow) appeared thoroughly unenhanced on contrast-enhanced ultrasound mode. The artifact (indicated by a thin solid arrow) at the area representing tracheal cavity was also unenhanced. However, the area aside (indicated by a thin dashed arrow) was distinctly enhanced, which was an artifact of the enhanced isthmic tissue (indicated by a bold dashed arrow). C: Histologic findings of the isthmic hypoechoic lesion through core-needle biopsy revealed papillary thyroid carcinoma components. The cancer cells were columnar and obviously atypical with large nuclei, sulcus and inclusion bodies. The cells were arranged in irregular adenoid papillary and solid cord-like structures, and the interstitial fibrous tissue was significantly proliferated (H-E staining. Original magnification: ×200) |
|
图 2 甲状腺峡部乳头状癌气管壁镜面伪像及其随液体隔离变化 Fig 2 Mirror artifact of isthmus papillary thyroid carcinoma and its change with hydro-dissection maneuver A: The true image of isthmic hypoechoic lesion (indicated by a bold solid arrow), sized about 2.9 mm×2.5 mm, with a transverse dimension smaller than the flat dimension of adjacent tracheal wall. A hypoechoic mirror artifact (indicated by a thin solid arrow) generated posterior to the anterior tracheal wall, in a similar shape but a smaller size than the true image. B: Fine needle aspiration was conducted with isthmus-tracheal wall hydro-dissection maneuver to investigate interfacial adhesion. The crescent-shaped isolation zone of saline (indicated by a bold dashed arrow) caused greatly flattened wall, with isolation zone artifact (indicated by a thin dashed arrow) formed posterior to the tracheal wall. The isthmic papillary thyroid carcinoma lesion still existed (indicated by a bold solid arrow), but its artifact was vanished, perhaps due to the increase of the distance between the real image and the anterior wall. C: Fine needle aspiration cytology revealed enlarged nuclei with nuclear sulci and pseudoinclusions, suggesting microscopic papillary carcinoma of the thyroid (Papanicolaou staining. Original magnification: ×400) |
|
图 3 甲状腺峡部粗大钙化灶气管壁镜面伪像及其随液体隔离变化 Fig 3 Mirror artifact of an isthmic coarse calcification and its change with hydro-dissection maneuver A: Coarse calcification (indicated by a bold solid arrow) at the position of isthmus and closely adjacent to tracheal wall causes a distinct mirror artifact (indicated by a thin solid arrow) across the anterior wall of trachea, which was far smaller than the true image, perhaps due to the overlap by the strong acoustic shadow of the true lesion. B: Hydro-dissection maneuver conducted among the posterior isthmic space during fine needle aspiration procedure caused both the appearance of mirror artifact (indicated by a thin solid arrow) of isolation zone of saline and disappearance of that of the isthmic coarse calcification, indicating that was a mirror artifact of the isthmic coarse calcification other than the calcification of the tracheal wall mucosa (the coarse calcification was indicated by a bold solid arrow, and the isolation zone was indicated by a bold dashed arrow) |
2.3 消融术中气管壁镜面伪像
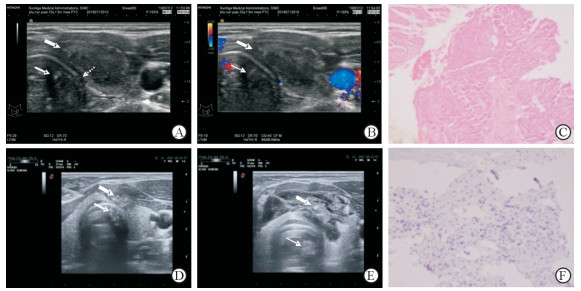
149例(88.17%)患者消融术中存在气管壁镜面伪像,包括隔离液注射针伪像133例、微波消融针热场强回声伪像16例、液体隔离带伪像137例。(1)注射针针尖的镜面伪像发生在甲状腺内侧间隙液体隔离过程中,其特点是实像针尖向前或向后移动时气管腔位置上的镜像相应地同向、同速度、同幅度运动(图 4)。(2)消融针针尖的镜面伪像发生在甲状腺结节消融过程中,消融针尖端的热量在结节内呈现向四周动态扩散的强回声改变,与此同时气管腔所在的声像位置上出现类似的动态强回声镜像。其特点是二者距离气管壁几近相等,二者连线与气管壁几近垂直;微波输出时二者同时出现,微波停止时二者同时消失;移动消融针尖时,二者同向、同速度、同幅度运动(图 5)。消融针针尖镜面伪像曾令术者担心微波热量传导至气管腔内损伤气管而有中止消融治疗的临时计划,后经严密监测呼吸和询问患者,确认患者无气管内灼热感、疼痛、呛咳、呼吸窘迫,才继续实施消融治疗。
|
图 4 隔离液注射针针尖气管壁镜面伪像 Fig 4 Mirror artifact of the needle tip appearing in the area representing tracheal cavity A: A case of follicular thyroid adenoma in the left lobe was to be treated with microwave ablation. Hydro-dissection maneuver was conducted among the posterior isthmus space and the inner thyroid space to protect the trachea. The true image of the injection needle tip (indicated by a fine solid arrow) generated virtual image with a clearer boundary and similar echo at the position representing trachea cavity (indicated by a fine dashed arrow). B: When the injection needle advanced or re-advanced, the virtual image of the needle tip kept moving in the same direction, at the same speed and at the same amplitude (indicated by a fine dashed arrow) |
|
图 5 微波消融针针尖气管壁镜面伪像 Fig 5 Mirror artifact of microwave ablation needle tip across the tracheal wall A case of right thyroid nodule was to be ablated by microwave. Hydro-dissection maneuver was conducted among the posterior isthmus space and the inner thyroid space to protect the trachea. While the microwave output was started, microwave radiation field was formed around the microwave needle tip, showing hyper-echoic true image (indicated by a fine solid arrow). The virtual image (indicated by a fine dashed arrow) generated at the position representing tracheal cavity with a clearer echo boundary, which was synchronized with the true image to blink and expand. After the suspension of microwave output, the virtual image stopped flashing and expanding. The possibility of conduction of heat into the tracheal cavity to damage the trachea was ruled out upon this manifestation |
2.4 消融术后气管壁镜面伪像
8例(4.73%)患者消融术后出现气管壁镜面伪像,均为甲状腺乳头状癌患者。消融区紧贴气管壁,呈低回声改变,气管腔的声像位置上出现团块状低回声或近似无回声的区域。其特点是:(1)二者以气管壁为分界线,近似对称;(2)二者形态较相似,但气管腔低回声区范围略小、境界较为模糊(图 6);(3)当探头向头侧或足侧移动离开消融区平面时,气管腔位置上的低回声区随即消失;(4)超声造影检查时二者均无增强现象(图 7);(5)随着消融区吸收缩小,伪像相应地变小直至消失(图 8)。乳头状癌消融区坏死组织的气管镜面伪像貌似肿瘤消融不全,或发生进展而浸润至气管内,令术者十分担心。经液体隔离法、超声造影检查及动态观察所见,术者确认其为气管壁镜面伪像。
|
图 6 甲状腺乳头状癌(PTC)消融区的气管壁镜面伪像 Fig 6 Mirror artifact of ablated area of papillary thyroid carcinoma (PTC) Pictures A to C were from a treated PTC case examined 3 months after microwave ablation. A: On the sonogram of an ablated area (indicated by a bold solid arrow) of left-side PTC at the end of the 3rd month after ablation, the transverse dimension from 0 to 3 o'clock of the anterior tracheal wall was flattened together with a rupture (indicated by a thin dashed arrow). A well-defined hypoechoic mirror artifact (indicated by a thin solid arrow) generated at the position representing tracheal cavity, with similar configuration to that of the true image of the ablated area. This artifact was absent but now readily misinterpreted as tumor invasion into tracheal cavity. B: Color Doppler flow imaging showed no color signal of blood flow both in the true image of ablated area (indicated by a bold solid arrow) and its mirror artifact position (indicated by a thin solid arrow). C: Microscopic observation of the specimen tissue near the edge of the trachea in the ablation area showed degenerated necrotic tissue and fibrosis hyperplasia with hyaline degeneration (H-E staining. Original magnification: ×200). Pictures D to F were from another treated PTC case examined 6 months after microwave ablation. D: The ablated area (indicated by a bold solid arrow) still contained more and strong echoes of tiny calcifications. The transverse dimension of tracheal wall from 0 to 2 o'clock was slightly flattened. A well-defined calcified mirror artifact (indicated by a thin solid arrow) generated at the position representing tracheal cavity, with similar configuration to that of the true image of the ablated area. This artifact was readily misinterpreted as tumor invasion into the tracheal cavity. E: Hydro-dissection maneuver revealed complete separation of the ablation area (indicated by a bold solid arrow) from the tracheal wall during fine needle aspiration procedure for therapeutic effect evaluation, indicating no adhesion to the tracheal wall. The distance between the ablation zone and the tracheal wall increased, so did the distance between the mirror artifact image (indicated by a thin solid arrow) and tracheal wall, indicating no tumor invasion into the trachea. F: Microscopic observation of the specimen from the ablation area showed obvious hyperplasia of fibrous tissue with hyaline degeneration and scattered calcification. No definite carcinoma cells were found. Immunohistochemical staining showed that the characteristic nuclear component of thyroid transcription factor 1 in thyroid follicular cells was negative (Original magnification: ×200), indicating no viable cancer tissue in the ablation area |
|
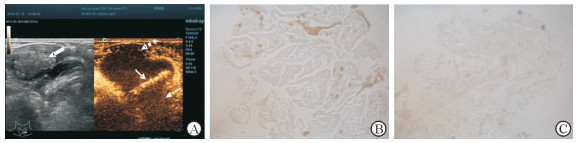
图 7 甲状腺乳头状癌消融区及其气管壁镜面伪像的CEUS模态 Fig 7 CEUS mode of ablation area of papillary thyroid carcinoma and its mirror artifacts A: A core-needle biopsy for histopathological evaluation of therapeutic efficacy was conducted to the ablation area (indicated by a bold solid arrow) of papillary thyroid carcinoma accompanied with CEUS evaluation and hydro-dissection maneuver at the end of the 3rd month of microwave ablation. On CEUS mode, both the true image of ablation area (indicated by a bold dashed arrow) and its mirror artifact (indicated by a thin dashed arrow) were thoroughly unenhanced, while the tracheal wall (indicated by a thin solid arrow) was still enhanced. It indicated that the blood supply was completely lost in the ablation area, and the tracheal wall was of integrity and with good blood supply. Hydro-dissection maneuver confirmed that the ablation area was completely separated from the tracheal wall, and there was no adhesion or tumor infiltration on the tracheal wall. B: Nicotinamide adenosine dinucleotide phosphate diaphorase (NADPH-d) enzyme chemical staining of coarse needle biospy specimens near the edge of trachea in the ablation area was negative, indicating no residual viable cells in the ablation area (Original magnification: ×200). C: Succinate dehydrogenase (SDH) staining of coarse needle biopsy specimens near the edge of trachea in the ablation area was negative too, indicating that there were no residual active cells in the ablation area (Original magnification: ×200). CEUS: Contrast-enhanced ultrasound |

|
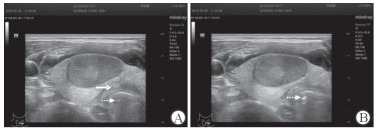
图 8 甲状腺消融区的气管壁镜面伪像的经时变化 Fig 8 Changes with time of mirror artifact of thyroid ablation area across the tracheal wall Compared with the manifestations on sonogram taken at the end of the 3rd month (A) after microwave ablation, the flat shape of the tracheal wall between 0 o'clock and 3 o'clock at 6 months after ablation (B) was significantly restored. Both the true images of ablation area (indicated by bold solid arrows) and mirror artifacts (indicated by thin solid arrows) were reduced in size |
2.5 甲状腺结节位置的比较
304例患者中135例未出现气管壁镜面伪像者,其甲状腺结节位于甲状腺上极、接近甲状软骨,或位于甲状腺下极甚至突至上纵隔内;而169例出现气管壁镜面伪像的患者,甲状腺结节均位于气管近旁区域内。甲状腺结节位置邻近气管是形成气管壁镜面伪像的重要因素(图 9)。

|
图 9 空气对超声全反射是气管壁镜面伪像的自然成因 Fig 9 Total reflection of air to ultrasound is the natural cause of mirror reflection artifacts A: The true image of the metal injection needle tip (indicated by a fine solid arrow) formed a mirror image at the position representing tracheal cavity (indicated by a fine dashed arrow); B: The true image of the metal injection needle tip (indicated by a fine solid arrow) did not form specular virtual image at the position representing thyroid adenoma except reverberation artifacts |
2.6 平坦大界面的形态比较
消融术前12例出现气管壁镜面伪像的甲状腺结节中,结节致气管壁扁平化9例,另3例气管壁虽未扁平化,但结节的最大径小于其后方气管壁较平坦段的线度。消融术中149例出现气管壁镜面伪像者,皆与液体隔离法致气管壁短暂扁平化有关。消融术后8例出现气管壁镜面伪像的陈旧性消融区,均伴有气管壁扁平化,随着消融区的萎缩气管壁扁平化程度减轻,气管壁镜面伪像逐渐弱化。气管壁扁平化、平坦界面线度大于结节实像亦为形成气管壁镜面伪像的重要因素。结节和消融区的直接压迫、液体隔离法是气管壁扁平化的直接原因。
3 讨论 3.1 气管壁镜面伪像的概念与形成条件气管由软骨、韧带和平滑肌构成。软骨和韧带的透声性较好,但气管腔内的气体对超声则近乎全反射[5]。就此而言,气管软骨-气管腔界面与横膈-肺泡腔界面具有相似性。然而通常情况下,无论超声探头于颈中央区垂直扫查甲状腺峡部-气管软骨-气管腔,还是从侧颈区向垂直扫查甲状腺叶-气管软骨-气管腔,气管软骨均呈凸起的圆弧状,缺乏横膈的平整性或轻度凹陷性。声束垂直于反射界面,界面平整、光滑,并且有足够大的线度,是镜面反射的基本形成条件[6]。气管壁虽光滑,但不具备平整性和足够大的平整线度,故甲状腺较少形成气管壁镜面伪像。气管软骨具有受挤压后变形的特点,如果气管壁由圆弧形向平面状变化,则可能导致镜面伪像形成。位于甲状腺峡部的乳头状癌结节或钙化结节可压迫气管壁致其扁平化,从而易形成气管壁镜面伪像。由此可见,本文所阐述的气管壁镜面伪像是指气管壁对超声波的镜面反射导致气管壁外侧结构,如甲状腺结节或穿刺针等实像,在气管壁内侧即气管腔位置上形成实际不存在的虚假影像。
3.2 甲状腺结节消融术中气管壁镜面伪像的形成机制液体隔离法是实施甲状腺结节热消融治疗时有效的保护措施[7]。在峡部与气管间隙(峡部后间隙)、两侧叶与气管间隙(甲状腺内侧间隙)实施液体隔离后,液体的张力挤压可使气管壁由圆弧形变为平面状。甲状腺-气管软骨-气管腔反射界面的平整性提高,线度增大,利于镜面伪像的形成。消融术中的镜面伪像主要有2种情形,分别为隔离液注射针镜面伪像和消融针镜面伪像,皆与峡部后间隙、甲状腺内侧间隙注射隔离液后气管软骨扁平化有关。隔离液注射针伪像随注射针的前进或后退发生同步运动。消融针伪像发生在微波能量输出时,消融针针尖周围热场内回声瞬间变强,强度足以使消融针针尖的气管壁镜面伪像清晰可辨。结节内热场范围不断扩大,强回声在动态中增强和扩大,镜面伪像也表现出相似的变化。当消融针前进或后退时镜像亦同步运动,停止微波能量输出时消融针伪像即消失。使用透明质酸钠凝胶作为隔离液可延长隔离带的有效隔离时长,减少甲状腺消融区与周围毗邻结构的粘连[8],但是其导致的甲状腺结节气管壁镜面伪像也更明显,这可能与其张力更大致气管软骨扁平化更明显有关。
3.3 消融术后消融区形成气管壁镜面伪像的可能机制甲状腺结节消融后消融区质地变硬[9]。紧贴气管壁的消融区可挤压气管软骨,致其弧度变小呈扁平化,利于镜面伪像的形成。随着消融区的吸收、缩小,其对气管壁的挤压逐渐减弱,气管弧度逐渐恢复,消融区气管壁镜面伪像则减弱至消失。
3.4 镜面伪像多出现在气管腔声像位置上的可能机制甲状腺周围结构组织种类多样,组织间的超声反射界面繁多,然而镜面伪像主要发生在气管腔声像位置上,这可能与气管腔内富含气体有关。空气对超声波近乎全反射,是气管壁形成镜面伪像的天然基础,而其他反射界面如甲状腺包膜背侧为软组织,对超声不具备全反射特性,因而即便反射界面接近平整且足够宽大,镜面伪像也较少见。
3.5 气管壁镜面伪像对甲状腺结节热消融治疗的不良影响(1)消融术前的不良影响。随着甲状腺结节微波消融治疗临床研究的拓展与进步,甲状腺乳头状癌也成为消融治疗的适应证之一[10]。但是对已侵犯气管的癌结节则不可以采取消融治疗。峡部乳头状癌的气管壁镜面伪像容易令术者误判肿瘤已经浸润至气管腔,从而影响其消融治疗方案的选择。(2)消融术中的不良影响。消融术中当气管腔位置上出现伴随微波启动和中止而变化的动态强回声,极易令术者认为热量通过某种途径(最有可能是静脉)进入了气管腔,可能导致气管烫伤。在真相未明时,术者的第一反应往往是停止消融治疗,并采取进一步检查和干预措施,造成手术现场的混乱和恐慌。(3)消融术后的不良影响。甲状腺乳头状癌行微波消融治疗日渐增多,如同手术切除一样,消融治疗后恶性肿瘤也存在复发和转移的可能[11]。位置紧贴气管的甲状腺乳头状癌消融区在气管腔位置上产生镜面伪像后,极易令术者误判为肿瘤消融不完全或肿瘤发生进展,突破气管壁浸润至气管腔内。
3.6 气管壁镜面伪像的识别与判断在甲状腺结节热消融的3个阶段中,正确识别和判断消融术中和术后的气管壁镜面伪像尤为重要,而消融术中消融针热场气管壁镜面伪像又是判别的重点。局部麻醉状态下,即便甲状腺内侧间隙麻醉剂使用足量也不能对气管黏膜面产生镇痛功效,无论是消融针直接触及气管壁还是热量传导至气管腔,患者均会有明显的痛感。采用由内向外的穿刺路径[12],消融针针尖方向背离气管,因此消融针直接损伤气管的可能性甚微。假设气管腔位置上的强回声改变是因热量传导至气管腔内导致,那么可以预见患者的咳嗽反射和疼痛反应将比较明显。消融术采用局部麻醉,术中应密切观察患者的疼痛反应、咳嗽反射、呼吸道通畅度等,结合停止微波能量输出时镜面伪像消失的特点,从而做出正确判断。对于紧贴气管的甲状腺乳头状癌消融区所致镜面伪像,可以通过超声造影加以判别,消融区实像与镜像在造影检查时均无造影剂充填。如若有肿瘤浸润气管腔,超声造影时肿瘤浸润区域会呈现增强改变,而镜面伪像却无增强。此外,在甲状腺乳头状癌消融术后第6个月进行消融区穿刺活组织检查评估灭活程度时[13],也可通过液体隔离法加以判别。在消融区与气管间隙注射隔离液后二者自由分开,表明消融区无活性组织浸润气管,并且随着隔离带增宽,气管壁镜面伪像弱化甚至消失。
| [1] |
MALHOTRA R, BRAMANTE R M, RADOMSKI M, NELSON M. Mirror image artifact mimicking heterotopic pregnancy on transvaginal ultrasound:case series[J]. West J Emerg Med, 2014, 15: 712-714. DOI:10.5811/westjem.2014.5.22508 |
| [2] |
AHN H, HERNÁNDEZ-ANDRADE E, ROMERO R, PTWARDHAN M, GONCALVES L F, AURIOLES-GARIBAY A, et al. Mirror artifacts in obstetric ultrasound:case presentation of a ghost twin during the second-trimester ultrasound scan[J]. Fetal Diagn Ther, 2013, 34: 248-252. DOI:10.1159/000353702 |
| [3] |
XIAOYIN T, PING L, DAN C, MIN D, JIACHANG C, TAO W, et al. Risk assessment and hydrodissection technique for radiofrequency ablation of thyroid benign nodules[J]. J Cancer, 2018, 9: 3058-3066. DOI:10.7150/jca.26060 |
| [4] |
顾建华, 赵欣, 王毅, 胡翔宇, 唐缨. 超声引导下微波消融治疗技术在甲状腺良性结节中的应用[J]. 中华超声影像学杂志, 2015, 24: 720-722. DOI:10.3760/cma.j.issn.1004-4477.2015.08.023 |
| [5] |
YOU J K, KIM D J, KIM B, HONG Y K. Thyroid cyst mirror artifact mimicking a tracheal cyst on ultrasound in a patient with excessive trachea collapsibility[J]. Radiol Case Rep, 2018, 13: 408-410. DOI:10.1016/j.radcr.2018.01.024 |
| [6] |
RUSSELL J, PATERSON K, COOPER S. Apparent heterotopic pregnancy created by mirror image artifact[J]. J Obstet Gynaecol Can, 2017, 39: 961-962. DOI:10.1016/j.jogc.2016.05.012 |
| [7] |
章建全, 盛建国, 刁宗平, 赵璐璐, 张航. 液体隔离法在颈部结节性病变经皮热消融治疗中的应用[J]. 第二军医大学学报, 2014, 35: 1045-1052. |
| [8] |
曹昆昆, 章建全, 赵佳琦, 黄禾菁, 吴震中. 透明质酸钠预防微波消融术后局部粘连的实验研究[J]. 现代生物医学进展, 2017, 17: 2837-2842. |
| [9] |
刁宗平, 章建全, 盛建国, 赵璐璐, 张航. 超声弹性成像在甲状腺良性结节射频消融中的应用价值及相关动态分析[J]. 第二军医大学学报, 2017, 38: 947-950. |
| [10] |
章建全.经皮热消融治疗在甲状腺乳头状癌及其区域淋巴结转移中的应用前景[J/CD].中华医学超声杂志(电子版), 2014, 11: 606-609.
|
| [11] |
伊丹丹, 黄韬, 宋鹏, 桑剑锋. 甲状腺微小乳头状癌手术方式对肿瘤复发影响的meta分析[J]. 东南大学学报(医学版), 2017, 36: 28-52. |
| [12] |
章建全, 马娜, 徐斌, 刘灿, 宋家琳, 刁宗平. 超声引导监测下经皮射频消融甲状腺腺瘤的方法学研究[J]. 中华超声影像学杂志, 2010, 10(19): 861-865. |
| [13] |
章建全, 闫磊, 陈红琼, 吴震中. 微波消融致甲状腺结节细胞活性的快速变化分析[J]. 中华医学杂志, 2018, 98: 3524-3527. DOI:10.3760/cma.j.issn.0376-2491.2018.43.012 |
 2019, Vol. 40
2019, Vol. 40


