退变性腰椎滑脱是中老年人群常见的腰椎退变性疾病,多发于50~60岁人群,以女性多见[1]。退变性腰椎滑脱的病因和发病机制复杂,由多种因素导致相邻椎体滑移而产生一系列症候群,最常见于L4~L5节段[2]。随着滑脱的进展,退变性腰椎滑脱患者脊柱和骨盆形态会发生代偿性改变以维持脊柱的平衡,在此过程中,脊柱-骨盆矢状位参数也会发生改变[3-8]。骨盆参数主要包括骨盆倾斜角(pelvic tilt,PT)、骨盆投射角(pelvic incidence,PI)和骶骨倾斜角(sacral slope,SS)等,脊柱参数主要包括胸椎后凸角(thoracic kyphosis,TK)、胸腰椎后凸角(thoracolumbar kyphosis,TLK)、腰椎前凸角(lumbar lordosis,LL)和矢状位躯干偏移(sagittal vertical axis,SVA)等。脊柱与骨盆在解剖结构上相连接,两者的矢状位参数相互关联、协调、匹配。本研究通过比较退变性腰椎滑脱患者与无滑脱的退变性腰椎疾病患者的脊柱-骨盆矢状位参数,分析影响腰椎滑脱程度的危险因素,为指导手术治疗、恢复腰椎滑脱矢状位参数的平衡提供参考。
1 资料和方法 1.1 研究对象选择我院2016年6月至2018年6月收治的退变性腰椎滑脱患者42例作为退变性腰椎滑脱组。纳入标准:(1)患者无腰椎骨折、外伤、峡部裂、肿瘤、结核等病史;(2)无腰椎及骨盆手术史;(3)有完整站立位脊柱全长X线片资料。排除标准:(1)特发性脊柱侧凸患者;(2)既往脊柱手术史者;(3)患有感染或肿瘤的患者。对照组为于我院门诊就诊的退变性腰椎疾病无滑脱患者58例。纳入标准:退变性腰椎疾病,无滑脱,无腰椎骨折、外伤、峡部裂、肿瘤、结核、手术等病史,有完整站立位脊柱全长X线片资料。本研究经海军军医大学(第二军医大学)长海医院伦理委员会审批。
1.2 数据采集收集两组患者的年龄、性别、身高、体质量等一般资料。在脊柱全长正侧位X线片上测量脊柱-骨盆矢状位参数,包括LL(L1椎体上终板与L5椎体下终板之间的Cobb角)、TLK(T10椎体上终板与L2椎体下终板之间的Cobb角)、TK(T5椎体上终板与T12椎体下终板之间的Cobb角)、SVA(C7椎体中点矢状铅垂线与S1椎体后上角的水平距离)、PT(股骨头中心连线中点和骶骨终板中点的连线与铅垂线之间的夹角)、PI(股骨头中心连线中点和骶骨终板中点的连线与骶骨终板垂线之间的夹角)、SS(水平线与骶骨终板切线之间的夹角)。采用腰椎滑脱率评价腰椎滑脱程度,腰椎滑脱率根据Taillard方法[9]计算(滑脱椎体与下位椎体后缘距离除以下位椎体上终板矢状径)。
1.3 统计学处理采用SPSS 19.0软件进行统计学分析。计量资料经SPSS 21.0软件Q-Q图分析符合正态分布,以x±s表示,组间比较采用独立样本t检验;计数资料以例数表示,组间比较采用χ2检验。以腰椎滑脱率为因变量,脊柱-骨盆矢状位相关参数为自变量,采用logistic回归模型分析与退变性腰椎滑脱程度相关的危险因素。检验水准(α)为0.05。
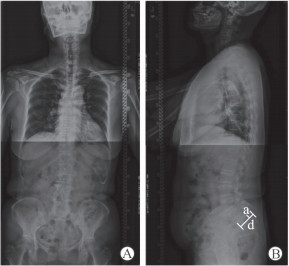
2 结果 2.1 一般资料退变性腰椎滑脱组纳入42例退变性腰椎滑脱患者,其中男17例、女25例,年龄为(59.43±5.99)岁,滑脱椎体包括L3 3例、L4 17例、L5 22例,典型脊柱全长正侧位X线片见图 1。对照组纳入无滑脱的退变性腰椎疾病患者58例,其中男24例、女34例,年龄为(60.09±6.20)岁。两组研究对象年龄、性别、身高、体质量差异均无统计学意义(P均>0.05),见表 1。
|
图 1 1例66岁女性L4/5滑脱患者脊柱全长正位(A)和侧位(B)X线片 Fig 1 Anterior posterior (A) and lateral (B) spine X-ray showing L4/5 spondylolisthesis in a 66 years old female patient a: Relative slippage distance of upper vertebral body on lateral radiograph; d: Sagittal diameter of superior endplate of lower vertebral body |
|
|
表 1 两组患者一般资料的比较 Tab 1 Comparison of general information between two groups |
2.2 两组脊柱-骨盆矢状位参数的比较
退变性腰椎滑脱组患者PT、PI、SS、LL、TLK、SVA均大于对照组且差异均有统计学意义(P均<0.05),但两组间TK差异无统计学意义(P>0.05),见表 2。
|
|
表 2 两组患者脊柱-骨盆矢状位参数的比较 Tab 2 Comparison of spinopelvic sagittal parameters between two groups |
2.3 影响腰椎滑脱程度的危险因素
退变性腰椎滑脱组患者采用logistic回归模型分析影响腰椎滑脱率的危险因素,结果发现LL、PT是影响腰椎滑脱率的危险因素(P<0.05),见表 3。
|
|
表 3 Logistic回归模型分析影响DLS患者腰椎滑脱率的危险因素 Tab 3 Risk factors of spondylolisthesis rate in DLS patients by logistic regression analysis |
3 讨论
正常脊柱呈现S型生理曲度,矢状位参数能很好地反映脊柱的平衡、代偿和生物力学改变情况[10]。脊柱和骨盆共同维持躯干平衡,退变性腰椎滑脱患者的脊柱和骨盆形态会出现代偿性改变,从而维持躯干平衡。为了探讨退变性腰椎滑脱患者脊柱-骨盆参数特征,本研究纳入42例退变性腰椎滑脱患者及58例无滑脱的退变性腰椎疾病患者,两组研究对象在年龄、性别、身高、体质量方面差异均无统计学意义,具有可比性。对两组研究对象的脊柱-骨盆矢状位参数进行比较,发现退变性腰椎滑脱组患者的PT、PI、SS、LL、TLK、SVA均大于对照组,差异均有统计学意义(P均<0.05)。这与Schuller等[11]的研究结果相似。这些结果提示在腰椎滑脱的进展中,随着滑脱程度增加SVA增大,为了维持SVA平衡,腰椎LL增大,而腰椎前凸的改变伴随骶骨的倾斜[12],SS相应发生了改变,由于PT和SS在评价骨盆形态上的效果一致[13],根据几何关系PI=PT+SS[14-15],PI也会增大。胸腰段的改变也易引起腰椎前凸改变,加速腰椎退变[16]。TK在两组之间差异无统计学意义,退变性腰椎滑脱患者腰椎前凸的改变需要通过改变胸椎后凸的角度来维持脊柱的矢状位平衡,但老年患者由于胸椎相对固定、活动度小,早期滑脱的患者该代偿性改变不明显,因此导致两组TK无明显差异。
大量研究表明,LL是需要与PI匹配的。Legaye和Duval-Beaupère[17]研究发现高PI需要高的LL匹配,Park等[18]的研究发现LL与PT、SS之间存在线性相关,Vialle等[19]研究发现LL与PI、SS之间有显著的相关性,Labelle等[20]发现退变性腰椎滑脱患者的LL、PT、SS是增大的。本研究结果与目前公认的低度滑脱的发生机制一致:PI增高,伴随的SS增大,LL代偿性增加[21-23]。由于PI=PT+SS,PT与SS在评价骨盆的位置时具有相同意义,因此在进行logistic回归分析滑脱程度的危险因素时,我们选择骨盆参数PT与脊柱矢状位参数LL、TLK、TK、SVA进行分析,结果显示LL和PT是影响滑脱程度的危险因素。
现阶段手术治疗仍是退变性腰椎滑脱的重要治疗方法,但是退变性腰椎滑脱的发病机制、病因仍不明确,需要进一步大样本随访研究。本研究主要是为手术治疗恢复脊柱-骨盆矢状位平衡提供参考依据,防止PI与LL出现不匹配,不能维持矢状位的SVA[24];PT及SS的改变说明出现骨盆倾斜,在手术中重建骨盆的PT能很好地改善骨盆的矢状位序列,维持脊柱矢状位的平衡[25-27]。术前需要对脊柱-骨盆矢状位参数进行详细分析,指导术中脊柱-骨盆矢状位平衡的重建,以获得满意的手术效果。
| [1] |
HE L C, WANG Y X, GONG J S, GRIFFITH J F, ZENG X J, KWOK A W, et al. Prevalence and risk factors of lumbar spondylolisthesis in elderly Chinese men and women[J]. Eur Radiol, 2014, 24: 441-448. DOI:10.1007/s00330-013-3041-5 |
| [2] |
盛亚超, 孙旭, 朱泽章, 史本龙, 孙伟翔, 陈曦, 等. 退变性腰椎滑脱French分型和CARDS分型的可重复性与可信度研究[J]. 中国脊柱脊髓杂志, 2017, 27: 228-234. DOI:10.3969/j.issn.1004-406X.2017.03.06 |
| [3] |
FUNAO H, TSUJI T, HOSOGANE N, WATANABE K, ISHII K, NAKAMURA M, et al. Comparative study of spinopelvic sagittal alignment between patients with and without degenerative spondylolisthesis[J]. Eur Spine J, 2012, 21: 2181-2187. DOI:10.1007/s00586-012-2374-0 |
| [4] |
LIM J K, KIM S M. Difference of sagittal spinopelvic alignments between degenerative spondylolisthesis and isthmic spondylolisthesis[J]. J Korean Neurosurg Soc, 2013, 53: 96-101. DOI:10.3340/jkns.2013.53.2.96 |
| [5] |
LABELLE H, MAC-THIONG J M, ROUSSOULY P. Spino-pelvic sagittal balance of spondylolisthesis:a review and classification[J]. Eur Spine J, 2011, 20(Suppl 5): 641-646. |
| [6] |
ROUSSOULY P, PINHEIRO-FRANCO J L. Biomechanical analysis of the spino-pelvic organization and adaptation in pathology[J]. Eur Spine J, 2011, 20(Suppl 5): 609-618. |
| [7] |
FERRERO E, OULD-SLIMANE M, GILLE O, GUIGUI P; French Spine Society (SFCR). Sagittal spinopelvic alignment in 654 degenerative spondylolisthesis[J]. Eur Spine J, 2015, 24: 1219-1227. DOI:10.1007/s00586-015-3778-4 |
| [8] |
LIU H, LI S, ZHENG Z, WANG J, WANG H, LI X. Pelvic retroversion is the key protective mechanism of L4-5 degenerative spondylolisthesis[J]. Eur Spine J, 2015, 24: 1204-1211. DOI:10.1007/s00586-014-3395-7 |
| [9] |
TAILLARD W F. Etiology of spondylolisthesis[J]. Clin Orthop Relat Res, 1976(117): 30-39. |
| [10] |
KIM H J, CHUN H J, LEE H M, KANG K T, LEE C K, CHANG B S, et al. The biomechanical influence of the facet joint orientation and the facet tropism in the lumbar spine[J]. Spine J, 2013, 13: 1301-1308. DOI:10.1016/j.spinee.2013.06.025 |
| [11] |
SCHULLER S, CHARLES Y P, STEIB J P. Sagittal spinopelvic alignment and body mass index in patients with degenerative spondylolisthesis[J]. Eur Spine J, 2011, 20: 713-719. DOI:10.1007/s00586-010-1640-2 |
| [12] |
RADOVANOVIC I, URQUHART J C, GANAPATHY V, SIDDIQI F, GURR K R, BAILEY S I, et al. Influence of postoperative sagittal balance and spinopelvic parameters on the outcome of patients surgically treated for degenerative lumbar spondylolisthesis[J]. J Neurosurg Spine, 2017, 26: 448-453. DOI:10.3171/2016.9.SPINE1680 |
| [13] |
LAMARTINA C, BERJANO P, PETRUZZI M, SINIGAGLIA A, CASERO G, CECCHINATO R, et al. Criteria to restore the sagittal balance in deformity and degenerative spondylolisthesis[J]. Eur Spine J, 2012, 21(Suppl 1): S27-S31. |
| [14] |
VRTOVEC T, JANSSEN M M, LIKAR B, CASTELEIN R M, VIERGEVER M A, PERNUŠ F. A review of methods for evaluating the quantitative parameters of sagittal pelvic alignment[J]. Spine J, 2012, 12: 433-446. DOI:10.1016/j.spinee.2012.02.013 |
| [15] |
LIM J K, KIM S M. Comparison of sagittal spinopelvic alignment between lumbar degenerative spondylolisthesis and degenerative spinal stenosis[J]. J Korean Neurosurg Soc, 2014, 55: 331-336. DOI:10.3340/jkns.2014.55.6.331 |
| [16] |
吉立新, 陈仲强. 胸腰段后凸畸形对腰椎前凸角度的影响及其临床意义[J]. 中国矫形外科杂志, 2003, 11: 1165-1166. DOI:10.3969/j.issn.1005-8478.2003.17.004 |
| [17] |
LEGAYE J, DUVAL-BEAUPÈRE G. Sagittal plane alignment of the spine and gravity:a radiological and clinical evaluation[J]. Acta Orthop Belg, 2005, 71: 213-220. |
| [18] |
PARK S J, LEE C S, CHUNG S S, KANG K C, SHIN S K. Postoperative changes in pelvic parameters and sagittal balance in adult isthmic spondylolisthesis[J]. Neurosurgery, 2011, 68(2 Suppl Operative): 355-363. |
| [19] |
VIALLE R, ILHARREBORDE B, DAUZAC C, LENOIR T, RILLARDON L, GUIGUI P. Is there a sagittal imbalance of the spine in isthmic spondylolisthesis? A correlation study[J]. Eur Spine J, 2007, 16: 1641-1649. DOI:10.1007/s00586-007-0348-4 |
| [20] |
LABELLE H, ROUSSOULY P, CHOPIN D, BERTHONNAUD E, HRESKO T, O'BRIEN M. Spino-pelvic alignment after surgical correction for developmental spondylolisthesis[J]. Eur Spine J, 2008, 17: 1170-1176. DOI:10.1007/s00586-008-0713-y |
| [21] |
ROUSSOULY P, GOLLOGLY S, BERTHONNAUD E, LABELLE H, WEIDENBAUM M. Sagittal alignment of the spine and pelvis in the presence of L5-S1 isthmic lysis and low-grade spondylolisthesis[J]. Spine (Phila Pa 1976), 2006, 31: 2484-2490. DOI:10.1097/01.brs.0000239155.37261.69 |
| [22] |
BOULAY C, TARDIEU C, HECQUET J, BENAIM C, MOUILLESEAUX B, MARTY C, et al. Sagittal alignment of spine and pelvis regulated by pelvic incidence:standard values and prediction of lordosis[J]. Eur Spine J, 2006, 15: 415-422. DOI:10.1007/s00586-005-0984-5 |
| [23] |
LAI Q, GAO T, LV X, LIU X, WAN Z, DAI M, et al. Correlation between the sagittal spinopelvic alignment and degenerative lumbar spondylolisthesis: a retrospective study[J/OL]. BMC Musculoskelet Disord, 2018, 19: 151. doi: 10.1186/s12891-018-2073-z.
|
| [24] |
WANG T, WANG H, LIU H, MA L, LIU F Y, DING W Y. Sagittal spinopelvic parameters in 2-level lumbar degenerative spondylolisthesis: a retrospective study[J/OL]. Medicine (Baltimore), 2016, 95: e5417. doi: 10.1097/MD.0000000000005417.
|
| [25] |
王太平, 郑召民, 刘辉, 张奎渤, 王华. 成人脊柱畸形矢状面平衡与生存质量的相关性分析[J]. 中华医学杂志, 2012, 92: 1481-1485. DOI:10.3760/cma.j.issn.0376-2491.2012.21.010 |
| [26] |
KIM M K, LEE S H, KIM E S, EOH W, CHUNG S S, LEE C S. The impact of sagittal balance on clinical results after posterior interbody fusion for patients with degenerative spondylolisthesis: a pilot study[J/OL]. BMC Musculoskelet Disord, 2011, 12: 69. doi: 10.1186/1471-2474-12-69.
|
| [27] |
FAUNDEZ A, ROUSSOULY P, LE HUEC J C. [Sagittal balance of the spine:a therapeutic revolution][J]. Rev Med Suisse, 2011, 7: 2470-2474. |
 2019, Vol. 40
2019, Vol. 40


