2. 复旦大学附属金山医院放射科, 上海 201508
2. Department of Radiology, Jinshan Hospital, Fudan University, Shanghai 201508, China
子宫腺肌症是一种常见的妇科良性疾病,因其临床表现缺乏特异性,术前诊断率仅为2%~26%[1]。随着非侵袭性影像学技术的进展,磁共振成像(magnetic resonance imaging,MRI)成为目前子宫腺肌症最可靠的检查方法,其中结合带区异常增厚、T1WI和(或)T2WI高信号是其诊断的主要征象,然而,MRI诊断标准尚未统一,且其诊断征象易受激素水平、子宫肌层收缩、结合带蠕动等影响[2-6]。本研究通过回顾性分析海军军医大学(第二军医大学)长海医院2013年1月至2016年1月37例经病理证实的子宫腺肌症患者的MRI资料,以明确子宫结合带厚度最大值(maximal junctional zone thickness,JZmax)、JZmax与结合带厚度最小值(minimal junctional zone thickness,JZmin)的差值(difference between the smallest and largest junctional zone thickness,JZdiff)、JZmax与肌层厚度最大值(maximal myometrial thickness,Mmax)的比值(JZmax/Mmax)3个结合带厚度评估参数和T1WI、T2WI高信号的诊断效能,加深对子宫腺肌症MRI主要诊断征象的认识,提高诊断水平。
1 资料和方法 1.1 病例资料纳入海军军医大学(第二军医大学)长海医院2013年1月至2016年1月经病理证实且术前行MRI检查的37例子宫腺肌症患者为子宫腺肌症组。子宫腺肌症组患者年龄为32~65岁,平均(46.7±7.3)岁。临床主要表现为痛经、月经量增多、不孕等,其中有17例患者合并子宫肌瘤、13例合并卵巢巧克力囊肿。收集同期行MRI检查的37例子宫及卵巢无明显病变者作为对照组。对照组患者年龄为18~79岁,平均(54.6±13.2)岁,其中肠癌20例、盆腔正常14例、痔疮2例、溃疡性结肠炎1例。
1.2 MRI扫描参数采用德国西门子1.5T超导MRI系统行MRI检查。检查时避开月经期,检查前取下金属节育环,适度充盈膀胱。自旋回波(spin echo,SE)T1加权像(weighted imaging,WI)扫描参数:重复时间(repetition time,TR)为550 ms,回波时间(echo time,TE)为14 ms,层厚为5 mm,间距为1.5 mm,矩阵为256×256。快速自旋回波(turbo spin echo,TSE)T2WI扫描参数:TR为4 500 ms,TE为96 ms,层厚为5 mm,间距为1.5 mm,矩阵为256×256;T2WI抑脂序列扫描参数:TR为3 000 ms,TE为64 ms,层厚为5 mm,间距为1.5 mm,矩阵为256×256。分别行矢状面、横断面扫描,部分加扫冠状面。
1.3 图像阅读与测量方法将MRI扫描图像发至图像存储与传输系统(picture archiving and communication system,PACS),分别由2位有经验的影像科医师阅片分析。在中矢状面观察和测量JZmax、Mmax和JZmin,并计算JZdiff(JZdiff=JZmax-JZmin)和JZmax/Mmax。观察两组T1WI和(或)T2WI上子宫壁内有无高信号及其类型。
1.4 统计学处理采用SPSS 18.0软件进行统计学分析。JZmax、JZdiff数据不符合正态分布,以中位数(下四分位数,上四分位数)表示,组间比较采用秩和检验;JZmax/Mmax数据符合正态分布,以x±s表示,组间比较采用两样本均数比较的t检验。根据病理结果对各参数绘制受试者工作特征(receiver operating characteristic,ROC)曲线,计算ROC曲线下面积(area under curve,AUC)、截断值、灵敏度、特异度及准确度。检验水准(α)为0.05。
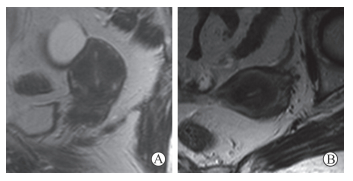
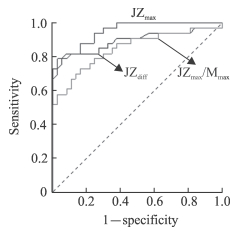
2 结果 2.1 子宫结合带厚度子宫腺肌症组患者中除4例(10.8%)结合带显示不清外,其余在T2WI矢状位上均表现为结合带不同程度增厚,呈弥漫性均匀增厚,与外肌层分界不清(典型图像见图 1)。在T2WI矢状位上对照组结合带均可清晰显示,呈均匀或不均匀低信号影。子宫腺肌症组和对照组患者的JZmax、JZdiff、JZmax/Mmax值见表 1,两组的JZmax、JZdiff、JZmax/Mmax差异均有统计学意义(P均 < 0.01)。JZmax、JZdiff和JZmax/Mmax诊断子宫腺肌症的ROC曲线分析结果显示,与其他两个参数相比,JZdiff≥3.4 mm诊断子宫腺肌症的灵敏度最高,而JZmax≥10 mm诊断子宫腺肌症的AUC、特异度和准确度最高(图 2、表 2)。
|
图 1 T2WI示子宫结合带均匀增厚的典型图像 Fig 1 Typical images of homogeneous thickening in junctional zone on T2WI A 60-year female patient. A: Sagittal T2WI; B: Axial T2WI.WI: Weighted imaging |
|
|
表 1 子宫腺肌症组与对照组患者的JZmax、JZdiff、JZmax/Mmax值 Tab 1 Values of JZmax, JZdiff, and JZmax/Mmax of patients in adenomyosis and control groups |
|
图 2 JZmax、JZdiff和JZmax/Mmax诊断子宫腺肌症的ROC曲线 Fig 2 ROC curves of JZmax, JZdiff and JZmax/Mmax for diagnosis of adenomyosis JZmax: Maximal junctional zone thickness; JZdiff: Difference between the smallest and largest junctional zone thickness; JZmax/Mmax: Ratio of JZmax and maximal myometrium thickness; ROC: Receiver operating characteristic |
|
|
表 2 JZmax、JZdiff、JZmax/Mmax诊断子宫腺肌症的ROC曲线下面积、截断值、灵敏度、特异度和准确度 Tab 2 AUC of ROC curve, cut-off value, sensitivity, specificity and accuracy of JZmax, JZdiff, and JZmax/Mmax for diagnosis of adenomyosis |
2.2 T1WI和(或)T2WI高信号
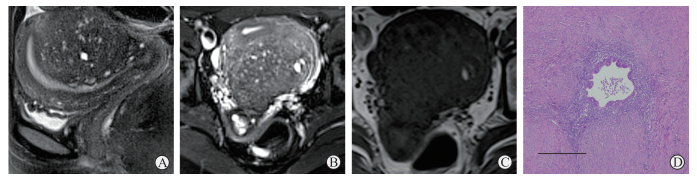
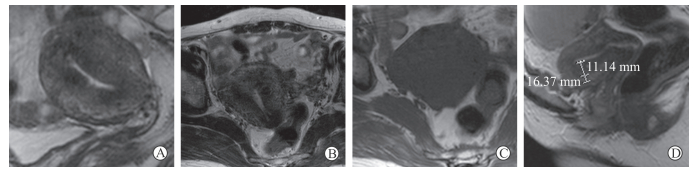
子宫腺肌症患者中18例(48.6%)仅见T2WI高信号,14例(37.8%)T1WI、T2WI均可见高信号,多呈飘雪征改变(图 3);线状条纹征(图 4A~4C)5例(13.5%),微囊征(图 4D)5例(13.5%),浆膜下囊性出血征1例(2.7%)。对照组T1WI、T2WI均未见明显高信号。
|
图 3 呈飘雪征表现的子宫腺肌症患者的MRI及病理图 Fig 3 MRI images of snowdrift sign in patients with adenomyosis and the pathology A 32-year female patient. A, B: Sagittal (A) and axial (B) fat-suppressed T2WI showed that the posterior wall of the uterus was full, with a round conjunctival hypotensive mass and unclear local boundaries, scattered the patchy or small saccular hyperintense (snowdrift sign); C: Axial T1WI showed that patchy hyperintense was scattered in the lesions with isointense signals, but the number of hyperintense was reduced obviously; D: Pathology showed the endometrioid tissue was found in the myometrium of the uterus, and the surrounding smooth muscle proliferated, with disordered and knitted arrangement (H-E staining, scale bar=500 μm). MRI: Magnetic resonance imaging; WI: Weighted imaging |
|
图 4 T2WI呈线状条纹征和微囊征表现的子宫腺肌症患者的典型图像 Fig 4 Typical images of linear stripe sign and microcapsule sign on T2WI in patients with adenomyosis A-C: A 56-year female patient. Sagittal T2WI (A) showed that the junctional zone was thickened evenly, and a short stripe of hyperintensity (linear stripe sign) extending from the endometrium to the junction zone was seen in the anterior wall of the uterus. The linear stripes were not well displayed on axial T1WI (B) and T2WI (C); D: A 45-year female patient. Sagittal T2WI showed that the thickness of the junctional zone was not uniform, and there was dot-shaped high-signal shadow wrapped in annular low-signal (microcapsule sign) in junction zone of the anterior wall, with JZmax=11.14 mm, but JZmax/Mmax=68.1%. WI: Weighted imaging; JZmax: Maximal junctional zone thickness; JZmax/Mmax: Ratio of JZmax and maximal myometrium thickness |
3 讨论
子宫腺肌症指子宫肌壁内出现具有活性的子宫内膜或内膜样组织,常伴周围平滑肌肥大和增生[7],多数研究者认为该病是由于子宫内膜与肌层间没有黏膜下层,内膜基底层的腺体及间质直接侵及内肌层所致[4, 8-10]。MRI是现今国内外公认的最可靠的子宫腺肌症检查方法,但目前子宫腺肌症的MRI诊断标准不统一、临床医师对诊断征象认识不充分,为其准确诊断带来了一定挑战[3-4, 11]。通过本研究并结合相关文献,现将子宫腺肌症的MRI主要诊断征象分析如下。
3.1 子宫结合带区异常增厚结合带正常结构破坏与异常增厚是MRI诊断子宫腺肌症的重要征象之一,主要表现为T2WI结合带区低信号且呈弥漫性或局灶性增厚,经病理证实为异位内膜周围增生肥大的平滑肌组织所致[12]。然而,类似子宫内膜,结合带随卵巢激素变化存在周期性增厚及生理性蠕动[2, 4, 9, 11],为子宫腺肌症的MRI诊断带来挑战。
目前结合带增厚常用JZmax、JZdiff及JZmax/Mmax 3个参数进行评估,本研究通过绘制ROC曲线发现JZmax≥10 mm、JZdiff≥3.4 mm、JZmax/Mmax≥61%均具有显著的诊断价值。JZmax > 12 mm是目前诊断子宫腺肌症接受度最高的标准[13-14],其诊断子宫腺肌症的灵敏度为63%、特异度为96%,准确度为85%[4];而本研究中JZmax≥10 mm时其诊断效能最佳,灵敏度为78.8%、特异度为97.3%、准确度为88.6%,与上述文献[4]报道的准确度及特异度相似,且其灵敏度更高,表明JZmax≥10 mm具有较高的临床诊断价值。本研究中JZmax/Mmax≥61%时的诊断灵敏度为72.7%、特异度为83.8%、准确度为78.6%,虽然其灵敏度高于文献[15]报道(JZmax/Mmax > 40%时的灵敏度为65%),但其报道的特异度为92%、准确度为83%。分析其原因,文献中患者年龄为30~88岁,平均年龄约51岁,绝经后患者占31%[15],而本研究中绝大多数患者处于育龄期。绝经后子宫外肌层由于蜕变、脱水,T2WI信号常降低,接近结合带区信号[4],这可能是本研究中JZmax/Mmax诊断截断值高于既往研究[15]的原因,但受研究样本量限制,特异度和准确度有待提高,诊断标准仍需进一步明确。有研究发现JZdiff > 4.6 mm时有一定的诊断价值,其诊断效能略高于JZmax > 12 mm,尤其是在特异度方面[16-17]。目前关于JZmax的诊断灵敏度、特异度及准确度的描述仍比较少,本研究结果显示,JZdiff≥3.4 mm时的诊断灵敏度、特异度和准确度均较高(灵敏度为81.8%、特异度为91.9%、准确度为87.1%),有较高临床诊断参考价值。
本研究发现JZmax诊断子宫腺肌症的特异度优于JZdiff和JZmax/Mmax,而JZdiff诊断子宫腺肌症的灵敏度优于JZmax和JZmax/Mmax,三者在子宫腺肌症的MRI诊断中发挥着不同作用。JZmax的诊断效能最佳,简单直观且易于评估,但因结合带受卵巢激素影响较大,因此不仅常存在个体先天发育的差异,还存在周期性蠕动及生理性增厚的差异[2, 4, 11]。此外,受病灶在子宫肌层位置、大小的影响,结合带厚度也存在病理性差异,导致JZmax的诊断效能局部受限。JZmax/Mmax为结合带与相应肌层最大厚度的比值,其诊断能有效降低子宫个体先天发育差异的影响;JZmax/Mmax还在局限性子宫腺肌症微小病灶中发挥着独特的诊断优势,但JZmax/Mmax为间接评估指标,受JZmax及Mmax相关因素的影响,诊断上常存在误差,尤其是当肌层内合并子宫肌瘤等占位性病变时,会造成部分漏诊。JZdiff能降低月经周期结合带弥漫性生理性增厚的影响,在诊断腺肌瘤局部累及结合带及结合带不规则明显增厚时具有良好作用,但当结合带弥漫性均匀异常增厚或结合带蠕动所致结合带局部增厚时其诊断意义受限。
此外,本研究发现有4例(10.8%)患者结合带显示欠清,低于文献报道的20%~30%,因文献提及结合带在经前期、孕期及绝经后期多显示欠清,无法评估[4],而本次研究对象多为育龄期女性,受研究样本年龄分布及样本数量限制,具有一定的局限性。
3.2 T1WI和(或)T2WI高信号子宫腺肌症患者常在T2WI低信号结合带或腺肌瘤病灶内见散在斑片状、小囊样或不规则形高信号,典型者呈飘雪征,部分亦在T1WI中见类似高信号灶,但数量多少于T2WI。经病理证实仅表现为T2WI高信号的病灶为异位内膜组织或囊性扩张内膜腺体,而T1WI、T2WI均表现为高信号的病灶为出血内膜岛[12, 18]。
本研究中有18例(48.6%)子宫腺肌症患者仅在T2WI可见病灶内高信号,有14例(37.8%)在T2WI、T1WI上均见高信号,出现率均低于文献报道的50%~88%[19],这可能是因为异位内膜组织多为对月经周期激素变化反应迟钝的内膜基底型,出血灶往往较少。此外,即使没有出血或治疗,这些高信号的数量常随时间变化[3, 12],而且当异位内膜灶或出血灶较小时MRI诊断易存在主观忽视,也可能造成影响。
本研究中有5例(13.5%)患者T2WI可见由内膜延伸至结合带的高信号线状条纹征,高度提示子宫内膜基底层直接侵袭肌层可能,从形态学上直观表明子宫内膜直接侵袭的病因学说。尽管线状条纹征出现率不高,但其在子宫腺肌症的诊断中发挥着无法比拟的独特作用。此外,有5例(13.5%)局限性子宫腺肌症表现为在增厚不明显的T2WI低信号结合带内可见点状或短条状高信号的微囊征,该病灶可能是子宫内膜早期异位灶,此时邻近肌层组织增生不明显。因本研究是回顾性分析,无法进行针对性病理取材证实该推测。早期子宫腺肌症病灶的识别有利于提高临床诊疗效果,因此进一步行前瞻性研究尤为必要。
肌层内异位的内膜组织出血严重时常导致囊性子宫腺肌症的发生,T2WI表现为与子宫分界欠清的低信号环包裹的多房混杂囊性信号灶,低信号环的囊壁有时表现为内层低信号和外层略高信号2层,分别代表结合带和外肌层,其中T1WI高信号囊液表示出血[3-4]。本研究仅发现1例浆膜下囊性子宫腺肌症,且病灶范围较大累及左侧附件,表现为多个大小不一的囊样混杂信号,部分在T1WI上表现为高信号。
3.3 合并症有文献提及约39%的子宫腺肌症患者合并卵巢巧克力囊肿,其中至少63%的患者结合带无明显增厚[7],本研究中子宫腺肌症合并巧克力囊肿患者13例(35.1%),李小川和郎景和[11]认为子宫内膜异位症是通过以局部雌激素升高为主的激素异常影响内膜下肌层的蠕动,从而导致腺肌症的发生,但二者复杂的关系还有待进一步探讨。
综上所述,子宫腺肌症的MRI诊断征象主要包括结合带区异常增厚和T1WI、T2WI高信号,JZmax≥10 mm、JZdiff≥3.4 mm、JZmax/Mmax≥61%时其诊断价值显著,其中JZmax的诊断效能最佳,而JZdiff、JZmax/Mmax能不同程度弥补JZmax的诊断不足。T1WI和(或)T2WI中的飘雪征、线状条纹征、微囊征、囊性出血征诊断子宫腺肌症具有独特性。综合评估这些MRI诊断征象可提高MRI的诊断价值,为早期正确诊断子宫腺肌症提供可能。
| [1] | BENAGIANO G, BROSENS I, HABIBA M. Adenomyosis:a life-cycle approach[J]. Reprod Biomed Online, 2015, 30: 220–232. DOI: 10.1016/j.rbmo.2014.11.005 |
| [2] | BENAGIANO G, HABIBA M, BROSENS I. The pathophysiology of uterine adenomyosis:an update[J]. Fertil Steril, 2012, 98: 572–579. DOI: 10.1016/j.fertnstert.2012.06.044 |
| [3] | TAMAI K, TOGASHI K, ITO T, MORISAWA N, FUJIWARA T, KOYAMA T. MR imaging findings of adenomyosis:correlation with histopathologic features and diagnostic pitfalls[J]. Radiographics, 2005, 25: 21–40. DOI: 10.1148/rg.251045060 |
| [4] | NOVELLAS S, CHASSANG M, DELOTTE J, TOULLALAN O, CHEVALLIER A, BOUAZIZ J, et al. MRI characteristics of the uterine junctional zone:from normal to the diagnosis of adenomyosis[J]. AJR Am J Roentgenol, 2011, 196: 1206–1213. DOI: 10.2214/AJR.10.4877 |
| [5] | FORNAZARI V A V, VAYEGO S A, SZEJNFELD D, SZEJNFELD J, GOLDMAN S M. Functional magnetic resonance imaging for clinical evaluation of uterine contractility[J/OL]. Einstein (Sao Paulo), 2018, 16: eMD3863. doi: 10.1590/s1679-45082018md3863. |
| [6] | 陆海迪, 强金伟. 子宫腺肌症的MRI研究现状及进展[J]. 实用放射学杂志, 2016, 32: 792–795. |
| [7] | KISHI Y, SUGINAMI H, KURAMORI R, YABUTA M, SUGINAMI R, TANIGUCHI F. Four subtypes of adenomyosis assessed by magnetic resonance imaging and their specification[J]. Am J Obstet Gynecol, 2012, 207: 111–114. |
| [8] | 史精华, 金力. 子宫腺肌病发病机制的研究进展[J]. 中华妇产科杂志, 2015, 50: 709–711. DOI: 10.3760/cma.j.issn.0529-567x.2015.09.015 |
| [9] | 冒小燕, 郭孙伟. 子宫异常收缩与子宫腺肌病[J]. 中华妇产科杂志, 2011, 46: 147–149. |
| [10] | 韦人瑞, 黄小飞, 李静, 张明理. 子宫腺肌症MRI检查的价值及病理分析[J]. 临床医学研究与实践, 2017, 2: 135–136. |
| [11] | 李晓川, 郎景和. 古子宫与子宫内膜异位症[J]. 中华妇产科杂志, 2011, 46: 219–221. |
| [12] | 侯金文, 程华, 李传福. 子宫腺肌症的MRI表现及其病理学对照研究[J]. 中华放射学杂志, 2002, 36: 67–71. |
| [13] | SOFIC A, HUSIC-SELIMOVIC H, CAROVAC A, JAHIC E, SMAILBEGOVIC V, KUPUSOVIC J. The significance of MRI evaluation of the uterine junctional zone in the early diagnosis of adenomyosis[J]. Acta Inform Med, 2016, 24: 103–106. DOI: 10.5455/aim. |
| [14] | KRENTEL H, CEZAR C, BECKER S, DI SPIEZIO SARDO A, TANOS V, WALLWIENER M, et al. From clinical symptoms to MR imaging: diagnostic steps in adenomyosis[J/OL]. Biomed Res Int, 2017, 2017: 1514029. doi: 10.1155/2017/1514029. |
| [15] | BAZOT M, CORTEZ A, DARAI E, ROUGER J, CHOPIER J, ANTOINE J M, et al. Ultrasonography compared with magnetic resonance imaging for the diagnosis of adenomyosis:correlation with histopathology[J]. Hum Reprod, 2001, 16: 2427–2433. DOI: 10.1093/humrep/16.11.2427 |
| [16] | AGOSTINHO L, CRUZ R, OSÓRIO F, ALVES J, SETÚBAL A, GUERRA A. MRI for adenomyosis:a pictorial review[J]. Insights Imaging, 2017, 8: 549–556. DOI: 10.1007/s13244-017-0576-z |
| [17] | DUEHOLM M, LUNDORF E, HANSEN E S, SØRENSEN J S, LEDERTOUG S, OLESEN F. Magnetic resonance imaging and transvaginal ultrasonography for the diagnosis of adenomyosis[J]. Fertil Steril, 2001, 76: 588–594. DOI: 10.1016/S0015-0282(01)01962-8 |
| [18] | BYUN J Y, KIM S E, CHOI B G, KO G Y, JUNQ S E, CHOI K H. Diffuse and focal adenomyosis:MR imaging findings[J]. Radiographics, 1999, 19: S161–S170. DOI: 10.1148/radiographics.19.suppl_1.g99oc03s161 |
| [19] | REINHOLD C, TAFAZOLI F, WANG L. Imaging features of adenomyosis[J]. Hum Reprod Update, 1998, 4: 337–349. DOI: 10.1093/humupd/4.4.337 |
 2018, Vol. 39
2018, Vol. 39


