上尿路尿路上皮癌(upper-tract urothelial carcinoma,UTUC)是来源于肾盏至输尿管远端尿路上皮的恶性肿瘤,包括肾盂癌和输尿管癌。UTUC发病率低,仅约十万分之一,占所有尿路上皮癌的5%~10%[1]。目前UTUC的标准治疗方案为根治性肾输尿管切除术加膀胱袖状切除术[2]。已有文献报道,对部分低级别、单发、体积小的UTUC,保留肾单位手术如输尿管节段切除术、输尿管镜或经皮肾镜下肿瘤激光烧灼术等可获得较满意的治疗效果[3-4]。UTUC术后肿瘤复发最常见为膀胱复发,其发生率为16.7%~60.7%[5-6]。本研究旨在探讨UTUC术后膀胱复发的相关危险因素。
1 资料和方法 1.1 临床资料收集2008年1月至2017年12月于我院泌尿外科就诊并确诊为UTUC患者的病例资料。所有纳入患者的临床和手术信息完整,病理诊断明确且术后随访信息完整。2008年至2011年UTUC术后膀胱灌注化学治疗未应用于全部患者,2012年后UTUC术后3 d内常规行1次膀胱灌注化学治疗,常用化学治疗药物包括丝裂霉素、表柔比星和吡柔比星。本研究通过海军军医大学(第二军医大学)生物医学研究伦理委员会审批。
1.2 观察指标收集患者的年龄、性别等基本资料。通过门诊、住院电子病历和电话随访收集患者的手术方法、术后病理结果(肿瘤的数量、位置、分期、分级、淋巴结转移情况)、术后膀胱灌注情况与术后随访资料。
1.3 统计学处理采用SPSS 19.0软件进行统计学分析。计量资料以x±s表示,计数资料以例数和百分数表示。通过单因素Cox回归模型分析与UTUC术后膀胱复发相关的危险因素,包括性别、年龄(<65岁和≥65岁[7])、膀胱癌病史、尿脱落细胞(阳性、阴性或未检查)、肾积水、输尿管镜检查、术前肌酐水平(<133 μmol/L和≥133 μmol/L,<133 μmol/L为临床肌酐的正常参考值)、肿瘤分类(输尿管癌、肾盂癌或两者均有)、肿瘤位置[输尿管下段、输尿管中段、输尿管上段(包括肾盂)]、手术方式(开放和腹腔镜)、治疗方式(根治术和局部切除术)、肿瘤分期(Ta、T1、T2和≥T3)、肿瘤分级(低级别或级别未知和高级别)、淋巴结转移(阳性、阴性或未行淋巴结清扫)、术后膀胱灌注化学治疗情况;检验水准(α)为0.1。将单因素分析差异有统计学意义的危险因素纳入多因素Cox回归模型,采用向前逐个纳入方法明确UTUC术后膀胱复发的独立危险因素;检验水准(α)为0.1。采用Kaplan-Meier生存曲线和log-rank检验分析患者无膀胱复发生存情况;检验水准(α)为0.05。
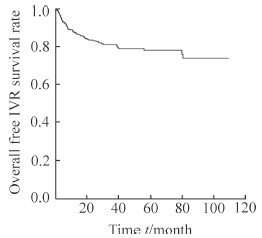
2 结果 2.1 一般资料共纳入445例UTUC患者,其中男性293例、女性152例,平均年龄为(66.2±10.6)岁。仅患输尿管癌的患者为214例,仅患肾盂癌194例,同时患输尿管和肾盂癌37例。术前伴肾积水患者为151例,其中112例术前肌酐水平≥133 μmol/L;无肾积水294例。195例尿脱落细胞检查阳性,64例阴性,186例未行尿脱落细胞检查。254例行术前输尿管镜检查,191例未行输尿管镜检查。378例行腹腔镜手术,67例行开放手术。384例行根治性肾盂输尿管切除术加膀胱部分袖状切除术,61例行保留肾单位肿瘤局部切除术。术后病理结果示:145例患者肿瘤位于输尿管下段,61例位于输尿管中段,239例位于输尿管上段(包括肾盂);肿瘤分期为Ta期84例、T1期131例、T2期82例、≥T3期148例;低级别或级别未知UTUC患者为127例,高级别318例;淋巴结转移阳性25例,阴性或未行淋巴结清扫420例。术后行单次膀胱灌注化学治疗者379例,未行该治疗者66例。术后中位随访时间为33.5个月,共80例(18.0%)患者发生膀胱复发,其中53例(66.2%)为术后1年内复发,20例(25.0%)为术后1~3年(≥1年且<3年)复发,7例(8.7%)为术后3年后(≥3年)复发(图 1)。69例患者膀胱初次复发后行经尿道膀胱肿瘤电切除术,8例行膀胱根治性切除术加输尿管皮肤造口术,3例因肿瘤远处转移或高龄拒绝手术治疗。膀胱复发后行手术治疗的77例患者术后病理结果示:55例为高级别,15例为低级别,7例分级未报告;72例为Ta或T1期,5例为T2期。
|
图 1 UTUC患者术后总体无IVR的Kaplan-Meier生存曲线 Fig 1 Kaplan-Meier curve of overall free IVR survival rate of UTUC patients after surgery UTUC: Upper-tract urothelial carcinoma; IVR: Intravesical recurrence |
2.2 UTUC术后膀胱复发危险因素单因素Cox回归分析
单因素Cox回归分析发现,UTUC患者年龄≥65岁、有膀胱癌病史、输尿管下段UTUC、行保留肾单位肿瘤局部切除术与UTUC术后膀胱复发密切相关(P均<0.01),见表 1。
|
|
表 1 UTUC患者术后膀胱复发危险因素单因素Cox回归模型分析 Tab 1 Univariable Cox regression model for predicting intravesical recurrence of UTUC patients after surgery |
2.3 UTUC术后膀胱复发危险因素多因素Cox回归分析
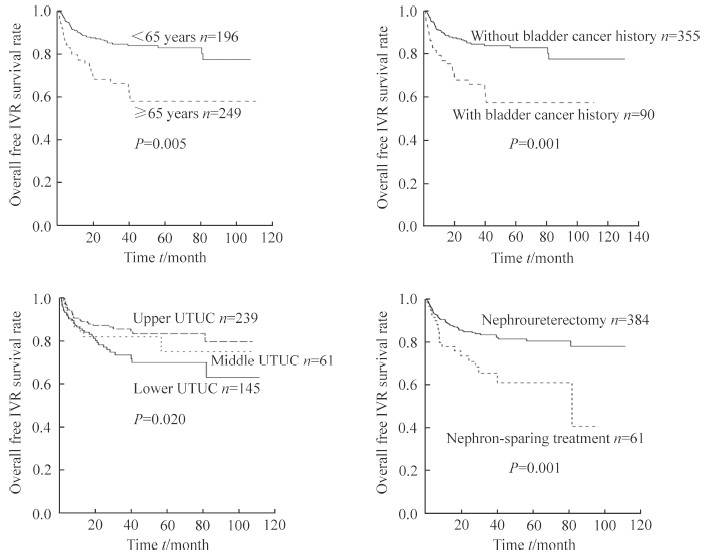
将年龄≥65岁、有膀胱癌病史、输尿管下段UTUC、行保留肾单位肿瘤局部切除术纳入多因素Cox回归模型进行分析,发现上述因素均为UTUC术后膀胱复发的独立危险因素(P均<0.1,表 2)。应用Kaplan-Meier生存曲线分析发现,年龄≥65岁、有膀胱癌病史、UTUC肿瘤发生于输尿管下段、行保留肾单位肿瘤局部切除术UTUC患者的无膀胱复发生存率均低于年龄<65岁、无膀胱癌病史、UTUC肿瘤发生于输尿管中段或上段、行根治性肾盂输尿管切除术加膀胱部分袖状切除术的患者,且差异均有统计学意义(P均<0.05,图 2)。
|
|
表 2 UTUC 患者术后膀胱复发危险因素多因素 Cox 回归模型分析 Tab 2 Multivariable Cox regression model for predicting intravesical recurrence of UTUC patients after surgery |
|
图 2 不同IVR独立危险因素UTUC患者术后无IVR的Kaplan-Meier生存曲线 Fig 2 Kaplan-Meier curves of free IVR survial rate of UTUC patients with several independent risk factors of IVR after surgery UTUC: Upper-tract urothelial carcinoma; IVR: Intravesical recurrence |
3 讨论
膀胱是UTUC术后复发的常见部位,本研究对UTUC术后患者随访33.5个月,发现UTUC术后膀胱复发率为18.0%(80/445),其中膀胱初次复发发生于术后1年内、术后1~3年(≥1年且<3年)、术后3年后(≥3年)的患者分别为53例(66.2%)、20例(25.0%)、7例(8.7%),提示UTUC术后膀胱复发率可能随时间推移逐渐下降。探讨UTUC术后膀胱复发危险因素对于实现UTUC患者危险分层、预后判断、随访策略制定有重要意义。《欧洲泌尿外科协会UTUC诊治指南》将UTUC术后膀胱复发危险因素分为3类:(1)患者相关因素,包括性别、膀胱癌病史、吸烟史及术前肾功能等;(2)肿瘤相关因素,包括术前尿脱落细胞、肿瘤位置和分期、是否为多发肿瘤等;(3)治疗相关因素,包括腹腔镜手术、是否行膀胱袖状切除术、切缘是否阳性等[8]。
Xylinas等[9]分析1 839例UTUC患者的病例资料,发现高龄、男性、腹腔镜手术、肿瘤内镜下处理、输尿管下段肿瘤、膀胱癌病史、肿瘤分期等是UTUC术后膀胱复发的独立危险因素。与该研究结果相似,本研究通过多因素Cox回归模型分析与UTUC术后膀胱复发相关的危险因素,发现患者年龄≥65岁、有膀胱癌病史、行保留肾单位肿瘤局部切除术和肿瘤发生于输尿管下段是UTUC术后膀胱复发的独立危险因素。目前,我院泌尿外科已对UTUC患者术后常规行单次膀胱灌注化学治疗,仅少数早期UTUC患者未行该治疗。可能是由于UTUC术后未行膀胱灌注化学治疗患者例数少,本研究中并未发现UTUC术后是否行膀胱灌注化学治疗是膀胱复发的危险因素。O’Brien等[10]研究发现UTUC根治术后行单次膀胱灌注化学治疗能够降低膀胱复发率的11%。因此,对于存在UTUC术后膀胱复发高危因素的患者,需术后行膀胱灌注化学治疗并且加强膀胱镜随访监测,但是否需增加膀胱灌注化学治疗次数仍有待明确。
近年来,诊断性输尿管镜检查是否增加UTUC术后膀胱复发存在争议。本研究发现术前输尿管镜检查并不是UTUC术后膀胱复发的危险因素。Marchioni等[5]通过meta分析发现,UTUC术前行诊断性输尿管镜检查组膀胱复发率(39.2%~60.7%)较未行输尿管镜检查组(16.7%~46.0%)明显升高(P<0.001)。Lee等[11]发现诊断性输尿管镜检查明确UTUC后立即行手术治疗并不增加术后膀胱复发率,而输尿管镜检查5 d后再行手术治疗则会增加膀胱复发率。Yoo等[12]对387例UTUC患者的临床资料进行分析,发现输尿管镜检查不增加输尿管癌患者术后膀胱复发风险,但肾盂癌患者行输尿管镜检查后膀胱复发率较输尿管癌患者明显增高(62.2% vs 39.6%,P=0.012)。目前,诊断性输尿管镜的应用指征以及输尿管镜检查发现UTUC后是否需预防性应用膀胱灌注化学治疗仍有待进一步探索。
腹腔镜手术是否增加UTUC术后膀胱复发风险同样存在争议。本研究发现腹腔镜手术与开放手术并不是UTUC术后膀胱复发的独立危险因素,但我院泌尿外科数据以腹腔镜手术为主(占84.9%,378/445),可能使结果存在偏倚。Kido等[13]与Liu等[14]分析行根治性手术治疗的UTUC患者资料发现,腹腔镜或开放性UTUC根治术并不影响UTUC术后膀胱复发率。而Shigeta等[15]则发现腹腔镜UTUC根治术中气腹时间延长会增加UTUC术后膀胱复发率。
综上所述,本研究发现年龄≥65岁、有膀胱癌病史、行保留肾单位肿瘤局部切除术和肿瘤发生于输尿管下段是UTUC术后膀胱复发的独立危险因素,对于存在上述危险因素的UTUC患者术后需加强随访监测,并定期复查膀胱镜。对存在术后膀胱复发高危因素的UTUC患者,是否需增加膀胱灌注化学治疗次数仍有待明确。
| [1] | SORIA F, SHARIAT S F, LERNER S P, FRITSCHE H M, RINK M, KASSOUF W, et al. Epidemiology, diagnosis, preoperative evaluation and prognostic assessment of upper-tract urothelial carcinoma (UTUC)[J]. World J Urol, 2017, 35: 379–387. DOI: 10.1007/s00345-016-1928-x |
| [2] | 那颜群, 叶章群, 孙颖浩, 孙光. 中国泌尿外科疾病诊断治疗指南[M]. 2014版. 北京: 人民卫生出版社, 2014: 33-34. |
| [3] | SIMHAN J, SMALDONE M C, EGLESTON B L, CANTER D, STERIOUS S N, CORCORAN A T, et al. Nephron-sparing management vs radical nephroureterectomy for low-or moderate-grade, lowstage upper tract urothelial carcinoma[J]. BJU Int, 2014, 114: 216–220. DOI: 10.1111/bju.2014.114.issue-2 |
| [4] | GADZINSKI A J, ROBERTS W W, FAERBER G J, WOLF J S. Long-term outcomes of nephroureterectomy versus endoscopic management for upper tract urothelial carcinoma[J]. J Urol, 2010, 183: 2148–2153. DOI: 10.1016/j.juro.2010.02.005 |
| [5] | MARCHIONI M, PRIMICERI G, CINDOLO L, HAMPTON L J, GROB M B, GURULI G, et al. Impact of diagnostic ureteroscopy on intravesical recurrence in patients undergoing radical nephroureterectomy for upper tract urothelial cancer:a systematic review and metaanalysis[J]. BJU Int, 2017, 120: 313–319. DOI: 10.1111/bju.2017.120.issue-3 |
| [6] | SEISEN T, GRANGER B, COLIN P, LEON P, UTARD G, RENARD-PENNA R, et al. A systematic review and meta-analysis of clinicopathologic factors linked to intravesical recurrence after radical nephroureterectomy to treat upper tract urothelial carcinoma[J]. Eur Urol, 2015, 67: 1122–1133. DOI: 10.1016/j.eururo.2014.11.035 |
| [7] | WHO Guidelines Approved by the Guidelines Review Committee. Global recommendations on physical activity for health[J]. Geneva:World Health Organization, 2010: 1–58. |
| [8] | ROUPRET M, BABJUK M, COMPERAT E, ZIGEUNER R, SYLVESTER R J, BURGER M, et al. European Association of Urology guidelines on upper urinary tract urothelial cell carcinoma:2015 update[J]. Eur Urol, 2015, 68: 868–879. DOI: 10.1016/j.eururo.2015.06.044 |
| [9] | XYLINAS E, KLUTH L, PASSONI N, TRINH Q D, RIEKEN M, LEE R K, et al. Prediction of intravesical recurrence after radical nephroureterectomy:development of a clinical decision-making tool[J]. Eur Urol, 2014, 65: 650–658. DOI: 10.1016/j.eururo.2013.09.003 |
| [10] | O'BRIEN T, RAY E, SINGH R, COKER B, BEARD R, British Association of Urological Surgeons Section of Oncology. Prevention of bladder tumours after nephroureterectomy for primary upper urinary tract urothelial carcinoma:a prospective, multicentre, randomised clinical trial of a single postoperative intravesical dose of mitomycin C (the ODMIT-C Trial)[J]. Eur Urol, 2011, 60: 703–710. DOI: 10.1016/j.eururo.2011.05.064 |
| [11] | LEE J K, KIM K B, PARK Y H, OH J J, LEE S, JEONG C W, et al. Correlation between the timing of diagnostic ureteroscopy and intravesical recurrence in upper tract urothelial cancer[J/OL]. Clin Genitourin Cancer, 2016, 14: e37-e41. doi: 10.1016/j.clgc.2015.07.008. http://cn.bing.com/academic/profile?id=fa1d096779d15fbaf04c069f0aa3736c&encoded=0&v=paper_preview&mkt=zh-cn |
| [12] | YOO S, YOU D, SONG C, HONG B, HONG J H, KIM C S, et al. Risk of intravesical recurrence after ureteroscopic biopsy for upper tract urothelial carcinoma:does the location matter?[J]. J Endourol, 2017, 31: 259–265. DOI: 10.1089/end.2016.0611 |
| [13] | KIDO K, HATAKEYAMA S, FUJITA N, YAMAMOTO H, TOBISAWA Y, YONEYAMA T, et al. Oncologic outcomes for open and laparoscopic radical nephroureterectomy in patients with upper tract urothelial carcinoma[J/OL]. Int J Clin Oncol, 2018 Feb 12. doi: 10.1007/s10147-018-1248-9.[Epubaheadofprint]. https://link.springer.com/article/10.1007%2Fs10147-018-1248-9 |
| [14] | LIU J Y, DAI Y B, ZHOU F J, LONG Z, LI Y H, XIE D, et al. Laparoscopic versus open nephroureterectomy to treat localized and/or locally advanced upper tract urothelial carcinoma: oncological outcomes from a multicenter study[J/OL]. BMC Surg, 2017, 17: 8. doi: 10.1186/s12893-016-0202-x. https://bmcsurg.biomedcentral.com/articles/10.1186/s12893-016-0202-x |
| [15] | SHIGETA K, KIKUCHI E, HAGIWARA M, ANDO T, MIZUNO R, MIYAJIMA A, et al. Prolonged pneumoperitoneum time is an independent risk factor for intravesical recurrence after laparoscopic radical nephroureterectomy in upper tract urothelial carcinoma[J]. Surg Oncol, 2017, 26: 73–79. DOI: 10.1016/j.suronc.2017.01.003 |
 2018, Vol. 39
2018, Vol. 39


