慢性硬膜下血肿是神经外科的常见疾病,具体发病机制不明,目前认为其主要与外伤、脑萎缩、自身免疫性疾病等密切相关[1]。慢性硬膜下血肿的治疗以钻孔引流术为主,但术后复发率高、治愈时间长仍是困扰神经外科医师的难题。临床在传统钻孔引流术的基础上,对钻孔引流术进行了一系列改良,包括按钻孔部位的额部钻孔引流与顶部钻孔引流、按钻孔数目的单孔引流与双孔引流、按引流管数目的单管钻孔引流与双管钻孔引流、按冲洗方式的灌洗和虹吸。各种术式都有其优缺点,目前尚未明确哪种术式治疗慢性硬膜下血肿更有效。随着对慢性硬膜下血肿发病机制研究的深入,单纯药物治疗的病例也逐渐增多。笔者采用阿托伐他汀钙配合单孔双管冲洗引流治疗慢性硬膜下血肿,疗效满意,现将诊治经验报告如下。
1 资料和方法 1.1 病例资料纳入我院于2016年5月至2017年4月收治的慢性硬膜下血肿患者42例,男33例、女9例,年龄为38~82岁,平均年龄为(70.0±5.8)岁。42例患者均接受阿托伐他汀钙配合单孔双管冲洗引流治疗。42例患者均有头痛,头晕症状,36例有不同程度肢体肌力障碍。本研究通过我院医学伦理委员会审批。
1.2 治疗方法所有病例均于血肿最厚处钻孔。患者取仰卧位,头偏向一侧;麻醉满意后取直切口;颅骨钻孔1个,十字形切开硬脑膜,释放血肿后,引流管反复冲洗直至清亮;向前额及向后枕各放置引流管1根,枕部引流管放置深度不超过4 cm,额部引流管尽量贴近体位最高点;明胶海绵封闭骨孔后,予以生物蛋白胶密闭空间,间断缝合头皮各层,将额部引流管略抬高,从枕部方向引流管注生理盐水,将气体排净后,快速接密闭引流袋。术后即予阿托伐他汀钙20 mg每天1次口服(直至血肿完全消失)。分别于术后即刻和第2天复查头颅计算机断层扫描(computed tomography,CT)。与术后即刻相比,术后第2天头颅CT检查如发现脑膨复明显且引流液少于20 mL,于术后第2天拔除引流管;如引流液超过20 mL且脑膨复不佳,留置引流管至术后第3天拔除。术后嘱咐患者坚持服用阿托伐他汀钙,并分别于术后1、3、6个月复查头颅CT。
2 结果 2.1 一般资料42例患者CT检查均提示存在明确的慢性硬膜下血肿(血肿最厚处超过1 cm),脑室及中线受压,脑沟消失。42例患者中36例为单侧慢性硬膜下血肿,6例为双侧慢性硬膜下血肿(3例行双侧钻孔引流术,3例仅行单侧钻孔引流术)。
2.2 治疗与随访结果所有患者的头痛、头晕症状和肌力障碍术后24 h内均改善,1个月后症状完全消失。42例患者术后即刻复查头颅CT示中线及脑室受压较术前改善,受压脑沟恢复;38例患者术后第2天复查头颅CT示受压情况进一步改善并当日拔除引流管,4例患者术后第2天复查头颅CT结果同术后即刻,于术后第3天日拔除引流管。1例双侧慢性硬膜下血肿患者因心房颤动口服华法林,术后1个月时复查头颅CT提示慢性硬膜下血肿复发,拟行二次治疗,在家突发呼吸心脏骤停死亡;22例患者术后3个月时复查头颅CT提示血肿完全消失;19例患者术后6个月时复查头颅CT示血肿完全消失。6例双侧慢性硬膜下血肿患者中,3例患者仅行单侧硬膜下血肿钻孔引流术,其中1例患者术后3个月时复查头颅CT示对侧血肿消失,2例在术后6个月复查时对侧血肿消失。
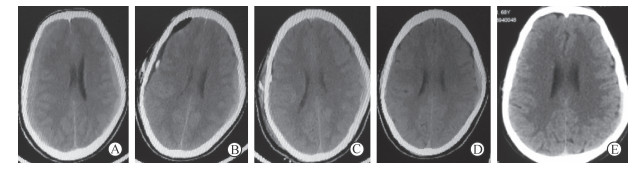
2.3 典型病例患者男,68岁,因“头部外伤1个月、头部胀痛1周加重伴左侧肢体无力3 d”入院。体格检查主要为左侧肢体肌力4级,术前头颅CT示双侧慢性硬膜下血肿,右侧为重(图 1A)。急诊行右侧硬膜下血肿钻孔引流术,术后即刻复查头颅CT提示血肿引流充分(图 1B),患者左侧肢体无力症状完全消失,肌力恢复至5级。术后一直口服阿托伐他汀钙;术后第2天复查头颅CT示脑膨复良好(图 1C),予以拔除引流管,术后第4天出院。1个月后头痛症状完全消失,复查头颅CT提示双侧血肿较前明显吸收(图 1D);3个月后复查头颅CT提示双侧血肿完全消失(图 1E)并停药。
|
图 1 典型慢性硬膜下血肿病例手术治疗前后头颅计算机断层扫描图像 A:术前双侧慢性硬膜下血肿, 中线左侧移位; B:术后即刻右侧血肿清除干净, 中线完全恢复; C:术后第2天脑膨复良好; D:术后1个月双侧慢性硬膜下血肿较术前明显减少; E:术后3个月双侧慢性硬膜下血肿完全消失 |
3 讨论
慢性硬膜下血肿好发于老年人,其具体发病机制不明,多数有外伤病史,在外力作用下,引起桥静脉或硬脑膜与脑皮质间细小交通动脉破裂出血,血液积聚在硬膜下形成硬膜下血肿[2];此外,抗凝药物的使用、持续加重的炎症反应及新生血管生成过程中反复破裂出血导致了血肿进一步增大[3]。治疗慢性硬膜下血肿药物的病理机制主要集中在炎症反应与血管生成两个方面,药物治疗慢性硬膜下血肿主要有三大类药物:糖皮质激素、氨甲环酸和他汀类药物。糖皮质激素能阻止慢性硬膜下血肿形成中的炎症应答[4],降低术后复发率,但长期应用糖皮质激素会增加感染、消化道出血及水肿等风险[5-6]。氨甲环酸通过减弱纤溶亢进降低血管通透性,从而阻止慢性硬膜下血肿扩大[7],但氨甲环酸治疗慢性硬膜下血肿的文献报道少,且其作为止血药物是否会增加缺血性脑卒中风险尚未明确。他汀类药物中阿托伐他汀应用最广泛,阿托伐他汀能促进血管生成,也有抑制炎症和降低促炎因子水平的作用[8-9],且不良反应少。药物治疗慢性硬膜下血肿仍缺乏大规模的多中心临床试验研究,而且慢性硬膜下血肿有自愈倾向,药物是否发挥了确切效果尚有争论。笔者采用阿托伐他汀钙配合单孔双管冲洗引流治疗的42例患者中,41例完全治愈;3例双侧慢性硬膜下血肿患者未行手术治疗的一侧血肿,仅单纯口服阿托伐他汀钙治疗获得治愈。
慢性硬膜下血肿量少(血肿最厚处<1 cm),无明显神经功能缺损,可单纯保守药物治疗;而血肿量多(血肿最厚处≥1 cm)且脑组织受压明确有症状,甚至出现神经功能缺损都应积极手术治疗,手术治疗的目的是减压和尽可能多地清除血肿。传统钻孔引流术短期疗效确切,但术后血肿复发及长期随访过程中局部积气、积液残留仍然是外科医师面对的难题。目前钻孔引流术手术术式多种多样,文献报道血肿复发率为2%~37%[10],复发的机制尚无统一定论,但可能与高龄、凝血功能异常、脑萎缩、双侧慢性硬膜下血肿、术后积气等因素有关[10]。笔者采用阿托伐他汀钙配合单孔双管冲洗引流治疗42例患者,仅1例(2.38%)双侧慢性硬膜下血肿患者复发,该患者为心房颤动患者,长期口服华法林抗凝。单孔双管冲洗引流有利于术中排气,减少术后积气;术后体位变化,引流更大概率都是在最低点,引流更充分,有利于脑膨复。单孔单管引流术中排气难度较大,术后容易出现颅内积气;引流管方向单一,为保证术后引流最低位,患者体位要求较高,高龄患者卧床容易出现肺炎等并发症,且引流并不充分。双孔双管引流手术操作相对复杂,术后感染风险相对较大[11],目前已逐渐被临床淘汰。
阿托伐他汀钙配合单孔双管冲洗引流是治疗慢性硬膜下血肿的有效方法,且操作相对简单,患者创伤小,值的广泛推广。
| [1] |
MIRANDA L B, BRAXTON E, HOBBS J, QUIQLEY M R. Chronic subdural hematoma in the elderly:not a benign disease[J]. J Neurosurg, 2011, 114: 72-76. |
| [2] |
SHUKLA D, DEVI B I, AGRAWAL A. Outcome measures for traumatic brain injury[J]. Clin Neurol Neurosurg, 2011, 113: 435-441. DOI:10.1016/j.clineuro.2011.02.013 |
| [3] |
INDRASWARI F, WANG H, LEI B, JAMES M L, KERMAGIS D, WARMER D S, et al. Statins improve outcome inmurlne models ofintracranial hemorrhage and traumatic brain injury:a translational approach[J]. J Neurotrauma, 2012, 29: 1388-1400. DOI:10.1089/neu.2011.2117 |
| [4] |
ESCOSA BAE M, WESSLING H, SALCA H C, HERAS ECHEVERRIA P D. Use of twist-drill craniostomy with drain in evacuation of chronic subdural hematomas:independent predictors of recurrebce[J]. Acta Neurochir (Wien), 2011, 153: 1097-1103. DOI:10.1007/s00701-010-0903-3 |
| [5] |
KAGEUAMA H, TOYOOKA T, TSUZUKI N, OKA K. Nonsurgical treatment of chronic subdural hematoma with tranexamic acid[J]. J Neurosurg, 2013, 119: 332-337. |
| [6] |
STANISIC M, LYNGSTADAAS S P, PRIPP A H, AASEN A O, LINDEQAARD K F, IVANOVIC J, et al. Chemokines as markers of local inflammation and angiogenesis in patients with chronic subdural hematoma:a prospective study[J]. Acta Neurochir (Wien), 2012, 154: 113-120. DOI:10.1007/s00701-011-1203-2 |
| [7] |
KOLIAS A G, CHARI A, SANTARIUS T, HUTCHINSON P J. Chronic subdural haematoma:modern management and emerging therapies[J]. Nat Rev Neurol, 2014, 10: 570-578. DOI:10.1038/nrneurol.2014.163 |
| [8] |
JIANG R, WANG D, POON W S, LU Y C, LI X G, ZHAO S G, et al. Effect of ATorvastatin On Chronic subdural Hematoma (ATOCH): a study protocol for a randomized controlled trial[J/OL]. Trials, 2015, 16: 528. doi: 10.1186/s13063-015-1045-y.
|
| [9] |
WANG B, SUN L, TIAN Y, LI Z, WEI H, WANG D, et al. Effects of atorvastatin in the regulation of circulating EPCs and angiogenesis in traumatic brain injury in rats[J]. J Neurol Sci, 2012, 319: 117-123. DOI:10.1016/j.jns.2012.04.015 |
| [10] |
JUNG Y G, JUNG N Y, KIM E. Independent predictors for recurrence of chronic subdural hematoma[J]. J Korean Neurosurg Soc, 2015, 57: 266-270. DOI:10.3340/jkns.2015.57.4.266 |
| [11] |
DUCRUET A F, GROBELNY B T, ZACHARIA B E, HICKMAN Z L, DEROSA P L, ANDERSEN K N, et al. The surgical management of chronic subdural hematoma[J]. Neurosurg Rev, 2012, 35: 155-169. DOI:10.1007/s10143-011-0349-y |
 2018, Vol. 39
2018, Vol. 39


