2. 同济大学附属上海市肺科医院超声科, 上海 200433
2. Department of Ultrasound, Shanghai Pulmonary Hospital, Tongji University, Shanghai 200433, China
胸腔闭式引流术是治疗胸腔积液最常用的方法,不仅能有效引流积液、促进肺复张、减少致热原[1],还可借助引流管注射药物进行局部治疗,如注入尿激酶溶解密集的纤维蛋白分隔、注入糖皮质激素抑制局部炎性渗出等[2-4]。在胸腔积液引流治疗中经常会遇到引流液停流的情况,有学者认为24 h无积液引出即可拔管或更换部位再次置管引流;也有学者认为由于蛋白凝块、白细胞等会阻塞引流管造成停流,可以尝试使用生理盐水反复冲洗[5-6]。笔者在工作中发现,由于临床判断引流管位置及积液腔内部情况的准确性不高,部分患者引流管并未脱出就接受反复的胸腔穿刺和引流,不仅给患者造成了痛苦,也给临床工作增添了负担。本研究应用超声检查观察胸腔剩余积液量和引流管内口位置,并借助超声造影剂的对比增强功能提高诊断准确性,现报告如下。
1 资料和方法 1.1 一般资料选取2018年1月至3月在同济大学附属上海市肺科医院行胸腔闭式引流术治疗中出现停流,且依据病情、引出积液量和体格检查判断积液未完全引出的患者,共44例。患者平均年龄为(64.59±12.90)岁,其中男性28例、女性16例,左侧胸腔积液29例、右侧15例,结核病18例、肺癌14例、慢性阻塞性肺疾病6例、肺炎4例、肺磨玻璃结节术后2例。所有接受检查和置管的患者均被详细告知相关获益和风险,并签署知情同意书。
1.2 仪器与药剂使用MyLabTM Twice型超声诊断仪(意大利Esaote公司)进行超声检查,凸阵探头CA541,频率1~8 MHz。闭式引流采用中心静脉导管包(珠海福尼亚医疗设备有限公司),型号CVC-1,规格16 G×20 cm,内含穿刺针、中心静脉导管、J形引导钢丝、皮肤扩张器、注射器等。超声造影剂为注射用六氟化硫微泡(Sonovue,意大利Bracco公司;批号:国药准字J20130045)。
1.3 检查方法同一患者先后经过临床和超声判断引流管内口是否在积液腔内,并比较两者的准确性。(1)临床判断:患者取坐位或侧卧位,使用注射器抽取适量生理盐水反复冲洗引流管,依据冲洗时阻力、是否可以抽出积液及抽出液性状判断引流管内口是否位于积液腔内。若阻力较小,可以抽出积液,抽出积液带有颜色、泡沫或组织等,可认为仍有积液残留且引流管内口未脱出积液腔;若阻力较大、难以抽出积液或抽出积液性状未改变则判断无积液残留或引流管已脱位。(2)超声判断:患者取端坐位,首先应用常规超声检查胸膜腔内是否有积液残留、最大深度、透声情况、是否存在纤维分隔等。然后进行超声造影检查,用10 mL注射器抽取0.2~0.3 mL配制好的超声造影剂(56 mg六氟化硫冻干粉与5 mL生理盐水混合并充分震荡)和10 mL生理盐水均匀混合,从引流管外口缓慢注射,在低机械指数(mechanical index,MI)超声造影模式下(MI设置为0.10)观察增强的引流管图像和造影剂分布情况,判断引流管通畅度和内口位置。(3)最终结果判断:所有患者均经生理盐水冲洗(经超声判断为多房分隔积液且引流管内口未脱出的患者注入尿激酶等纤维蛋白溶解药物促进纤维蛋白溶解)后,继续留管观察24 h,如有积液引出则认为引流管内口未脱出积液腔,如无积液引出则判断为引流管内口已脱出。采用最终判断结果对临床和超声两种判断结果进行准确性评估。
1.4 统计学处理应用SPSS 20.0软件进行统计学分析。计量资料以x±s表示;计数资料以例数和百分数表示,组间比较采用Pearson χ2检验。检验水准(α)为0.05。
2 结果 2.1 临床判断结果使用注射器抽取适量生理盐水反复冲洗引流管,推注生理盐水阻力大者27例(61.36%),阻力小者17例(38.64%);不可抽出液体或抽出量少于注入量者36例(81.82%),可抽出较多液体者8例(18.18%)。可抽出较多液体的8例中,抽出液颜色为淡黄色2例、淡红色1例、暗红色5例,抽出液内含白色泡沫5例、含片状或条索状组织或凝块3例。临床判断8例(18.18%)引流管内口未脱出积液腔(其中包含1例可抽出积液但阻力较大者),36例(81.82%)引流管已经脱出。
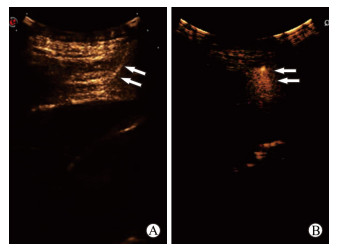
2.2 超声判断结果根据常规超声图像判断,44例患者均有胸腔积液残留,残留液最大深度为(66.92±32.70)mm。其中20例(45.45%)声像图表现为胸腔内呈絮状低回声伴细密点状高回声且可随体位流动,抽出后证实积液较为黏稠,多为血性或脓性(图 1A);11例(25.00%)可见积液腔内存在网状纤维分隔(图 1C)。超声造影模式下见引流管呈短直线样增强或无增强,止于胸壁软组织内(图 2A),判断为引流管已脱出积液腔;若继续推注造影剂,可见增强区局限于胸壁,胸膜腔内无增强(图 2B)。若观察到造影剂在引流管内流动呈线形增强(图 3A、3B,图 4A),积液腔随后开始增强,并逐渐扩散(图 3C、3D,图 4B~4D),则判断引流管未脱出积液腔;有时由于积液过于黏稠或多个纤维分隔相互不连通,也会出现造影剂扩散缓慢、局限于积液腔一处的情况(图 1B、1D)。综合分析超声造影图像后,判断29例(65.91%)引流管内口仍位于积液腔内;14例(31.82%)脱位,内口多位于肌层(7例)或脂肪层(5例),个别紧贴壁层胸膜外(2例);1例患者经超声检查无法判断引流管是否脱位,声像图可见积液透声差。对7例超声检查明确引流管内口未脱出的多房分隔积液注射纤维蛋白溶解药物,24 h内均引流出液体。

|
图 1 复杂胸腔积液声像图 Fig 1 Complicated pleural effusion under ultrasonography A: Viscous effusion; B: Distribution of contrast agents in thoracic cavity of viscous effusion; C: Multilocular pleural effusion; D: Distribution of contrast agents in thoracic cavity of multilocular pleural effusion |
|
图 2 超声造影示引流管脱出积液腔 Fig 2 Catheter outside effusion cavity as shown by contrast-enhanced ultrasound A: Linear enhancement of catheter in soft tissue of chest wall (arrows); B: Partially cloudy enhancement of soft tissue in chest wall (arrows) |

|
图 3 超声造影示引流管位于积液腔内 Fig 3 Catheter inside effusion cavity as shown by contrast-enhanced ultrasound Ultrasound contrast agent entering catheter (A, B; arrows) and effusion cavity (C, D; arrows) |

|
图 4 胸膜腔超声造影表现 Fig 4 Pleural cavity as shown by contrast-enhanced ultrasound Ultrasound contrast agent entering catheter (A) and pleural cavity (B-D) |
2.3两种方法判断引流管是否脱出积液腔的准确性比较由表 1可见,临床判断正确者22例,准确率为50.00%(22/44);超声判断正确者43例,准确率为97.73%(43/44)。经Pearson χ2检验,两种诊断方法的准确率差异有统计学意义(χ2=25.96,P<0.01),说明超声诊断准确性高于临床判断。
|
|
表 1 临床和超声判断引流管位置与最终判断结果的对比 Tab 1 Comparison of catheter positions judged by clinical data, ultrasound findings and final judgment results |
3 讨论
胸腔积液见于多种胸部疾病和肺疾病,其中最常见的病因为结核病和恶性肿瘤,积液有清亮的漏出液、渗出液,也有黏稠的血性液、脓性液[7]。胸腔闭式引流术是治疗胸腔积液最简单、最重要的方法,在临床上应用广泛。然而,在闭式引流治疗过程中,由于病情进展和药物反应可以发生胸膜增厚、纤维分隔增生以及积液性状的改变,从而导致引流管堵塞、位置移动,造成引流液停流[8]。此类原因造成的引流液停流与由于患者体位移动导致的引流管脱出胸膜腔难以鉴别,给临床医师带来不小的困扰。目前临床常常采用生理盐水推注的方法来判断引流管是否脱出,但准确性有限。另有报道采用胸部计算机断层扫描检查进行引流管位置判断,准确性较高,但费用昂贵、存在X线辐射,且不适用于重症患者[9]。
超声检查是临床公认的诊断胸腔积液最具优势、使用最多的方法,不仅可以判断积液存在与否、积液量的多少,还能观察胸膜和纤维分隔的厚度,且操作简便、费用低廉、可在床旁使用。既往受限于二维超声对引流导管显影不佳,采用超声检查判断引流管是否脱落存在一定误差。本研究开创性地将超声造影剂经引流管注射于胸腔内,观察胸腔闭式引流导管的位置及通畅度,是非血管内造影技术的又一拓展。
本研究中,临床准确判断出引流管内口未脱出的患者为8例。此类患者置管时间较长,积液内的固体成分沉积造成了引流管堵塞,通过反复生理盐水冲洗使引流管再次通畅并引流出积液。对此类患者,可以通过定期冲洗引流管、不引流时使用肝素封管等措施,减少由残留于引流管内的蛋白、细胞凝块造成的阻塞。
在临床判断引流管内口已脱出的36例患者中,14例判断正确。这类患者多由于外力牵拉导致引流管移位,应嘱患者避免剧烈运动,并加强引流管固定。由于部分患者皮下组织较为松弛,因此在注入生理盐水时阻力并不大,但抽出困难,仍然判断为引流管已脱出,后经超声造影发现造影剂停留在胸壁软组织内,积液腔无增强,证实了这一判断。
另外22例临床判断错误的患者中,其中14例由于积液黏稠度过高而引流管较细,尽管反复冲洗引流管使其通畅,但仍难以引流出积液。超声观察见此类积液透声差,可见絮状回声,提示积液性状稠厚;通过超声造影可观察到造影剂经引流管进入积液腔,弥散较慢且局限。这类患者可以通过使用内径更大或带有侧孔的引流管避免停流的发生。另有7例临床判断错误的患者为多房分隔性积液,由于积液腔内纤维分隔较厚,各腔之间几乎不连通,引流管所在分隔腔已经引流完全或已经闭合[10-11],故尽管引流管位置正常,但仍然无法引流出积液。超声造影观察到造影剂经引流管分布于1个或数个分隔腔内,其他分隔腔不增强。通过注射尿激酶(2~10万单位)等药物促进纤维蛋白分隔溶解,可进一步促进液体的引出[12]。
仅有1例患者推注生理盐水或超声造影剂时阻力极大,无法注入,临床判断引流管脱出,超声无法判断引流管是否脱位,声像图上可见积液透声差。分析原因可能由于积液黏稠,封管时又未用肝素,故引流管内液体凝固,导致无法注入生理盐水或造影剂。尽管无法判断引流管内口是否脱出,但这例患者仍需拔管重置。
综上所述,经引流管胸腔内超声造影可准确判断胸腔闭式引流管是否脱出,且能了解残留积液情况,为临床进一步治疗胸腔积液提供治疗策略,值得在临床工作中推广应用。
| [1] |
BHATNAGAR R, MASKELL N. The modern diagnosis and management of pleural effusions[J/OL]. BMJ, 2015, 351: h4520. doi: 10.1136/bmj.h4520. https://www.bmj.com/content/351/bmj.h4520
|
| [2] |
VILLENA GARRIDO V, CASES VIEDMA E, FERNÁNDEZ VILLAR A, DE PABLO GAFAS A, PÉREZ RODRÍGUEZ E, PORCEL PÉREZ J M, et al. Recommendations of diagnosis and treatment of pleural effusion. Update[J]. Arch Bronconeumol, 2014, 50: 235-249. https://www.ncbi.nlm.nih.gov/pubmed/24698396
|
| [3] |
CHUNG M H, HSIAO C Y, NIAN N S, CHEN Y C, WANG C Y, WEN Y S, et al. The benefit of ultrasound in deciding between tube thoracostomy and observative management in hemothorax resulting from blunt chest trauma[J]. World J Surg, 2018, 42: 2054-2060. DOI:10.1007/s00268-017-4417-5 |
| [4] |
MISHRA E K, CLIVE A O, WILLS G H, DAVIES H E, STANTON A E, AL-ALOUL M, et al. Randomized controlled trial of urokinase versus placebo for nondraining malignant pleural effusion[J]. Am J Respir Crit Care Med, 2018, 197: 502-508. DOI:10.1164/rccm.201704-0809OC |
| [5] |
PENZ E, WATT K N, HERGOTT C A, RAHMAN N M, PSALLIDAS I. Management of malignant pleural effusion:challenges and solutions[J]. Cancer Manag Res, 2017, 9: 229-241. DOI:10.2147/CMAR |
| [6] |
BIELSA S, ACOSTA C, PARDINA M, CIVIT C, PORCEL J M. Tuberculous pleural effusion: clinical characteristics of 320 patients[J/OL]. Arch Bronconeumol, 2018. pii: S0300-2896(18)30178-9. doi: 10.1016/j.arbres.2018.04.014.
|
| [7] |
MATHEW J L, SONI V, SINGH M, MITTAL P, SINGHI S, GAUTAM V, et al. Intrapleural streptokinase is effective and safe for children with multi-loculated empyema regardless of the time from disease onset[J/OL]. Acta Paediatr, 2018. doi: 10.1111/apa.14408.
|
| [8] |
廖维芬, 谢春梨, 李敏珍, 覃小玲. 失效模式与效应分析在预防胸腔闭式引流管滑脱中的应用[J]. 实用临床护理学杂志, 2016, 1: 160-161. |
| [9] |
王永芳, 查玉梅, 张晓荣, 吴冬梅. 浅析胸腔闭式引流术后常见问题及护理观察要点[J]. 中华全科医学, 2010, 8: 663-664. |
| [10] |
TSUJIMOTO N, SARAYA T, LIGHT R W, TSUKAHARA Y, KOIDE T, KURAI D, et al. A simple method for differentiating complicated parapneumonic effusion/empyema from parapneumonic effusion using the split pleura sign and the amount of pleural effusion on thoracic CT[J/OL]. PLoS One, 2015, 10: e0130141. doi: 10.1371/journal.pone.0130141. https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0130141
|
| [11] |
BHATNAGAR R, MASKELL N A. Treatment of complicated pleural effusions in 2013[J]. Clin Chest Med, 2013, 34: 47-62. DOI:10.1016/j.ccm.2012.11.004 |
| [12] |
FUJIWARA K, KOBAYASHI S, FUJIOKA N, TERAMOTO K, ITOH T, SUGIMURA H, et al. [Intrathoracic washing with urokinase was effective for empyema with atelectasis][J]. Kyobu Geka, 2013, 66: 391-393. |
 2018, Vol. 39
2018, Vol. 39


