胫骨干骨折属于高能量损伤,由于胫骨解剖形状和应力环境特殊,特别是粉碎性骨折术后,加上术者术中不恰当操作因素的影响,常导致胫骨骨折延迟愈合、骨不连发生[1-4]。据文献报道,胫骨骨折延迟愈合发生率为4.4%,特别是开放性骨折胫骨延迟愈合达到13%~41%[5-7],而开放性骨折骨不连发生率更高达10%~69%[8-10],胫骨已成为长骨干骨不连的高发部位。目前,对于胫骨骨折术后骨不连的治疗方法很多,但存在较多争议,采用何种内固定及手术方式治疗能够获得最佳的手术效果是当前研究的热点和难点。治疗胫骨骨不连时,因腓骨支撑形成应力遮挡,以致一部分骨不连需要反复手术才能愈合,并遗留骨不连、畸形愈合等严重的并发症[11-12]。促进骨不连的治愈、避免并发症及改善患者生活质量成为临床医师需要考虑的问题。文献报道,通过部分腓骨截骨来增加胫骨的应力传导可以促进胫骨骨不连的骨折愈合[13-14]。Thomas等[14-15]通过尸体生物力学实验进一步验证腓骨截骨可减少胫骨的张应力,增加骨折断端的压应力,从而缩小胫骨间隙促进骨折愈合。我科在总结以往经验的基础上,对2008年7月至2013年6月收治的45例胫骨骨不连患者进行腓骨截骨结合自体髂骨植骨治疗,取得满意疗效,现报道如下。
1 资料和方法 1.1 一般资料45例患者中男31例,女14例;年龄25~56 (33.5±11.2)岁。患者基本资料见表 1。骨不连判断标准[11] :骨折修复过程终止,主要是骨折块间有纤维组织或软骨组织形成,骨折在6个月仍未连接,再连续观察3个月,采取稳定骨折措施如石膏固定、支具固定制动或切开植骨仍未愈合者。骨折部位有疼痛,负重后局部疼痛加重,X线片显示骨折端硬化、无连续性骨痂通过或至少3层骨皮质无连续性骨痂通过。纳入标准:年龄18~60岁,均为非感染性骨不连。排除标准:病理性骨折,严重心脑血管、泌尿系统等全身疾病,急性感染,慢性疾病,或近期使用糖皮质激素和免疫抑制剂的患者。本研究经过长海医院伦理委员会批准,并取得所有纳入患者的知情同意及签字。
|
|
表 1 患者一般资料 Tab 1 Summary of clinical characteristics of patients |
1.2 腓骨截骨力学原理
在正常生理情况下,胫骨对上端的力量进行向下的传导,胫骨的生理弯曲对上端作用力的传导有分散作用,力量随着胫骨曲度的改变而改变,部分力量通过骨间膜分传至腓骨,由腓骨进行传递。当胫腓骨骨折时,因为腓骨的愈合能力早于胫骨成为应力遮挡结构,从而使胫骨的负重能力减少,通过部分腓骨截骨(截骨段>2 cm),增加胫骨的力学传导和负重,使胫骨紧密对合,促进胫骨骨折愈合[15-16]。如图 1所示。
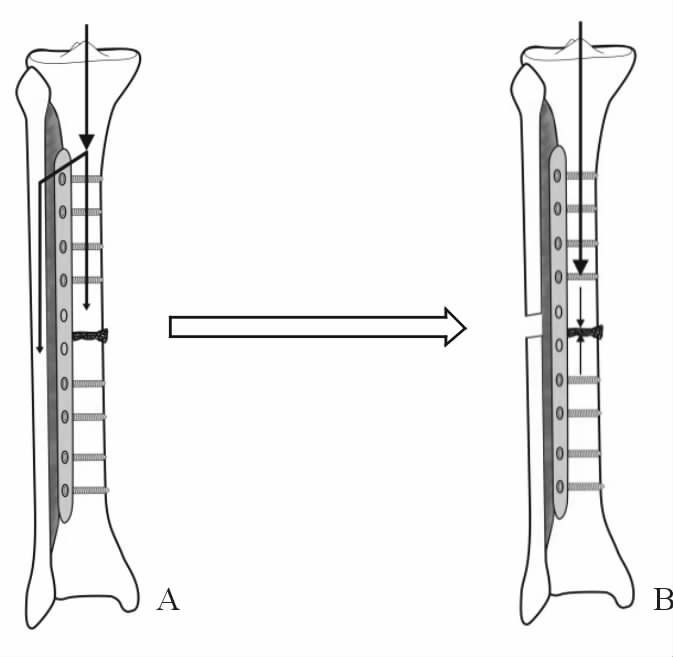
|
图 1 腓骨截骨示意图 Fig 1 Illustration of fibular osteotomy A: The mechanical transmission way on calf without fibulectomy; B: Mechanical transmission way on calf with fibulectomy |
1.3 手术方法
所有患者均行硬膜外麻醉或腰麻,取胫骨中下段前外侧切口,依次切开,显露骨断端。对于内固定失效的患者行内固定取出,本次研究纳入的32例钢板内固定患者中24例行钢板内固定取出更换锁定加压钢板髂骨植骨,再行腓骨截骨术: 采用腓骨后外侧入路或原手术切口,找到腓骨长短肌和比目鱼肌间隙(小腿外、后侧肌群间隙),钝性分离至腓骨,行骨膜下剥离显露腓骨,用骨刀或线锯截取2 cm的腓骨(图 2),截骨平面距踝关节至少8 cm,避免影响踝关节的稳定性,一般截取骨块大于2 cm,截取骨块过小因腓骨愈合较胫骨快而影响胫骨愈合。对于骨折端间隙过大而不能充分加压的患者,必要时加大截骨,适当短缩患肢(一般不超过2 cm)。另外8例钢板内固定患者行单纯腓骨截骨结合自体髂骨植骨术,11例髓内钉固定患者全部行髓内钉取出更换钢板内固定。首先用刮匙彻底刮除断端纤维结缔组织,咬骨钳咬除坏死骨及硬化骨,用钻头打通两端髓腔至正常骨组织。初试复位,尽量使骨折端进行加压,缩小骨折端间隙,从而获得较大的接触面。再选择长度合适的钢板予以加强固定,并通过钢板固定来维持小腿的完整力线。用游标卡尺测量骨折缺损的大小,然后取适量髂骨修剪成长条状骨条,将松质骨及皮质骨条填塞于骨折断端进行充分植骨。

|
图 2 术中显露并截取腓骨 Fig 2 Exposed fibular and fibular osteotomy during the operation A: The fibular was exposed during the operation; B: The fibular osteotomy (arrow) was taken out (about 2 cm) |
1.4 术后处理
术后肢体保暖,禁止吸烟,常规应用抗生素1~3 d,预防使用利伐沙班等,同时给予止痛处理。术后第1天小腿肌肉等长收缩锻炼,第2天开始患肢主动、渐进、增强太极式功能锻炼。术后第1天及1、3、6、9、12个月门诊随访时行X线片或CT检查。疗效评估:末次随访时采用Olerud-Molander评分标准[17]评定下肢关节功能;记录患者的关节活动度和疼痛情况,包括疼痛、关节僵硬、关节肿胀、上楼梯、跑、跳、蹲、行走及工作能力9项内容(满分100分):90~100分为优、60~89分为良、 30~59分为可,0~29分为差。并测量肢体的短缩情况:手术前后髂前上棘到外踝尖的距离之差。骨折愈合标准:完全负重后局部无疼痛,骨折间隙无压痛,X线或CT示胫骨至少3层骨皮质有连续性骨痂,无内固定失效。
2 结 果 2.1 手术情况及疗效患者手术时间为1.3~2.5 (1.7±0.5) h,术中出血量为200~500 (250.0±59.6) mL,腓骨截骨长度为2~3 (2.4±0.5) cm,髂骨植骨量为3~23 (7.8±1.3) cm3。随访时间为12~48 (16.5±3.3)个月,45例患者的骨折愈合时间为3~11 (5.6±2.4)个月。26例(58%)患者3~5个月愈合,13例(29%)患者6~8个月愈合,其余6例(13%)患者9~11个月愈合。肢体无短缩27例,短缩<1 cm者9例,短缩1~2 cm 6例,短缩>2 cm 3例。2 例肥大型骨不连患者伤口皮肤发生浅表感染,经换药2周愈合;1例肥大型骨不连患者术后2周发生深部感染,伤口红肿,给予抗炎处理,效果不佳,1周后流脓性分泌物,伤口经换药处理、抗生素治疗2周仍然效果不佳,予以二次清创、摆管冲洗、使用敏感抗生素4周后伤口愈合,复查炎性指标正常,术后6个月获骨性愈合;3例患者取骨区轻微疼痛。末次随访时评定下肢关节功能:优23例,良14例,可5例,差3例。
2.2 典型病例病例1,女性,58岁,车祸外伤导致右胫腓骨骨折。外院X线片示右胫腓骨下段骨折,伤后3 d行切开复位钢板内固定。术后3个月开始下床负重,自述小腿骨折处反复疼痛,术后9个月复查X线片示骨折未愈合,骨折端吸收;体格检查:右小腿肌肉萎缩明显,患肢末梢血供、感觉正常;诊断:右胫骨骨折术后骨不连。保留胫骨钢板,行腓骨钢板内固定取出+腓骨截骨结合自体髂骨移植(4.0 cm×3.0 cm×1.5 cm)。术后第1天开始行肢体功能锻炼,术后2个月扶拐下床逐步负重行走。术后6个月复查X线片示骨折愈合。术后18个月取出钢板,末次随访,患者对功能恢复满意(图 3)。

|
图 3 病例1术前、术后影像学表现和术中截骨、植骨情况 Fig 3 The pre- and post-operative imagings and intra-operative osteotomy and bone grafting in case one A: The X-ray imaging of tibial nonunion with plate internal fixation after surgery 9 months; B,C: Implant removing and fibular osteotomy and iliac bone grafting during operation; D: The post-anterior X-ray imaging of bone union 6 months after surgery; E: The X-ray imaging of remove of internal fixation 1.5 year after surgery |
病例2,男性,42岁。车祸外伤致左胫骨骨折。外院X线片示左胫骨下段骨折,伤后2 d行胫骨骨折切开髓内钉内固定术。术后5个月开始下床负重,主诉患肢反复疼痛,术后12个月复查X线片示骨折未愈合,骨折端吸收(图 4A);体格检查:右小腿色素沉着,患肢末梢血供、感觉正常;诊断:胫骨骨折髓内钉术后肥大型骨不连。于是在腰麻下行左胫骨髓内钉内固定取出+腓骨截骨结合自体髂骨移植(3.0 cm×4.0 cm×1.4 cm,图 4B)。术后开始功能锻炼,术后3个月扶拐下床逐步负重行走,术后5个月复查X线片示完全愈合(图 4C)。
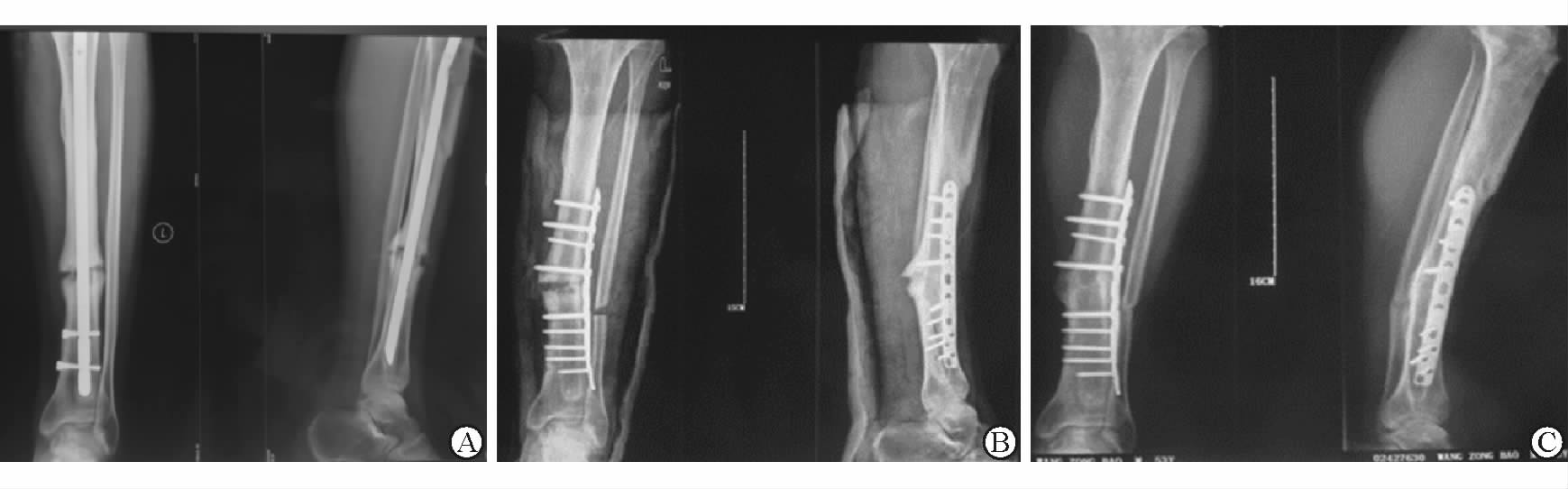
|
图 4 病例2的术前、术后影像学表现 Fig 4 The pre- and post-operative imagings in case two A: The X-ray imaging of tibial hypertrophic nonunion with plate internal fixation 12 months after surgery; B: The X-ray imaging of intramedullary fixation removing and exchange plating with fibular osteotomy and tiliac bone grafting; C: The post-anterior X-ray imaging of bone union 5 months after surgery |
3 讨 论
胫骨骨不连是胫骨骨折特别是开放性骨折初期治疗的常见并发症,形成原因复杂,治疗也比较棘手。随着内固定器械的不断改进和植骨技术的发展,治愈率有所提高,但对胫骨骨不连的治疗效果仍不满意,且并发症较多[18-21]。我们尝试采用腓骨截骨结合自体髂骨植骨治疗胫骨骨不连,使患者不愈合骨顺利愈合,骨折愈合率达到100%,且并发症少,不仅避免了多次反复手术给患者带来的严重创伤,而且取得满意的临床效果。
3.1 胫骨骨折术后骨不连的原因分析胫骨骨折是较为常见的骨折类型,由于其胫骨中段及中下段骨折后血运易受到破坏,骨不连发生率较其他部位高。首先,由于骨不连的形成原因较为复杂,在排除全身性因素及初始损伤相关因素的影响下,医源性手术操作加重对骨折造成血运的破坏[22-23],在骨折愈合过程中受到不利于骨折愈合的应力,如断端旋转应力或剪切应力,使髓腔、骨膜、周围组织新生血管形成和相互之间吻合过程受到影响,修复细胞的来源和演变变得迟缓,最终导致骨愈合停止,骨不连发生。其次,内固定材料选择不当,钢板长度、强度不够,髓内钉过细或使用不扩髓的髓内钉,使固定不稳,造成骨不稳定[24]。此外,下肢是负重肢体,腓骨和钢板的应力遮挡效应导致的骨质疏松及旋转应力引起骨折断端活动造成的力学不稳。本组入院患者钢板螺钉断裂13例,钢板螺钉松动11例,髓内钉过细5例,断裂3例,说明内固定不稳定是发生骨不连的一个重要原因。2例外固定支架固定患者,X线片显示骨折端对位对线较差,局部骨质严重疏松,骨折间隙较大。因此,外固定支架在骨折的复位方向和力学稳定性方面存在明显不足。综合分析胫骨骨折术后骨不连的原因可以发现,无论选择什么样的固定方式,确保骨折断端固定稳定和紧密接触才是骨折愈合最重要的保证。
3.2 胫骨骨折术后骨不连治疗方式探讨针对胫骨骨折术后骨不连的治疗方法较多,如保留髓内钉结合钢板固定、髓内钉动力化、更换锁定钢板、更换髓内钉等。由于骨折的部位、类型以及所造成的因素不同,临床中对于胫骨骨折髓内钉术后骨不连治疗尚未有明确的定论,其治疗方式仍然存在许多争议。对非峡部段的骨不连患者采用附加钢板固定,其双皮质螺钉还可起到阻挡钉的力学稳定作用[25]。Ateschrang等[26]报道了附加钢板治疗28例股骨骨不连患者,27例患者得到骨性愈合,愈合率达96.4%,但附加钢板只限于髓内钉过细引起的肥大型骨不连,适应证有限。
采用髓内钉动力化治疗是一种简单的方法,但主要适应于早期短斜型、横断骨折类型较为稳定的病例。也有反对者认为静力交锁髓内钉治疗胫骨骨折愈合率高达90%以上,而动力化骨愈合率只有54%[27]。扩髓更换髓内钉是较为常用的手术方案,其作用机制主要通过增强机械稳定性以及扩髓的生物学内植骨效应来促进骨折愈合。Hsiao等[28]报道胫骨扩髓增加1 mm,髓内钉与胫骨接触面积增加38.4%,通过增加髓内钉与髓腔的接触面积可以增加骨折端的稳定性和抵抗扭转载荷的刚度。据文献报道,扩髓更换髓内钉治疗胫骨骨不连愈合率达76%~98%[29]。Tsang等[30]报道扩髓更换增粗2 mm 的髓内钉治疗胫骨干骨不连96例,结果89例(93%)患者愈合。扩髓更换髓内钉适应于胫骨峡部骨不连,而对于非峡部或粉碎性骨折,髓内钉稳定性及抗旋转能力较差。目前研究多表明髓内钉在控制胫骨干旋转方面不如钢板。骨不连患者骨折部位大多需要切开暴露复位,髓内钉闭合插入不仅对软组织的保护效应不明显,而且会增加对膝关节的损伤。
当胫骨干骨折髓内钉或钢板内固定术后骨不连存在明显的旋转畸形或短缩时,改用髓内钉动力化、附加钢板疗效也不佳的时候,取出髓内钉改用钢板是最佳选择。Chen等[31]应用锁定加压钢板结合植骨治疗38例骨不连患者,愈合率为100%,El-Rosasy等[32]运用加压锁定钢板治疗13例胫骨远端畸形肥大型骨不连患者,小腿力线得到很好纠正,骨折愈合率为100%,愈合时间平均为3个月。我们使用钢板螺钉内固定结合自体骨植骨治疗胫骨干骨折术后骨不连也取得了满意的疗效。
3.3 腓骨截骨治疗胫骨骨不连的力学效果分析骨的质量与其生长发育过程中所受的生理性应力密切相关。Wolf定律认为:新骨形成取决于对应力的反应。骨重建是按其所进化的生理力学需要进行的,骨痂在需要处生长,而在不需要处吸收。在正常生理情况下,胫骨对上端的力量进行向下的传导,部分力量通过骨间膜分传至腓骨。胫腓骨骨折术后的患者由于腓骨骨折愈合的生长速度超过胫骨,成为应力遮挡结构,胫骨不愈合的患者由于内固定物具有应力遮挡作用,也承受了部分应力的传导,因此,胫骨骨折端所能承受到的应力非常小,甚至完全没有,这对骨折的愈合起到了非常大的阻碍作用。通过将完整的腓骨打断,甚至截骨,消除腓骨的应力遮挡,骨折断端充分地加压接触,使应力能够经由胫骨经过骨折端进行向下的传导,从而缩短骨折愈合所需要的骨传导和骨诱导的时间,加速骨折愈合,在尸体生物力学上已得到验证[16-17]。我们的临床手术疗效表明,腓骨截骨是治疗胫骨骨不连的有效方式之一。另外,截骨的位置通常选择外踝上方至少8 cm 处,过低则可能影响踝关节的稳定性。
当骨不连清除骨端瘢痕组织后必然留有不同程度的骨缺损,除了坚强的内固定和应力刺激,有效植骨是促进骨折愈合的重要方面,植骨填充骨缺损,同时发挥内支架作用,通过自体骨诱导成骨作用,不仅利用骨折早期愈合,而且可以降低应力遮挡率加速骨折愈合。根据我们的临床经验,依据骨折断端缺损大小,选择适量的髂骨进行三维植骨促进骨折愈合。当然,骨折断端缺损不宜大于5 cm,否则很容易造成骨块坏死、吸收而影响骨折的愈合。同时配合早期的功能锻炼,有助于促进骨折的愈合。
通过腓骨截骨结合髂骨植骨治疗胫骨骨不连可以对骨折断端进行加压,增加断端接触面积,具有明显促进骨折愈合的协调作用,临床愈合率高,并发症少,该方法为胫骨延迟愈合、骨不连的治愈提供了一条新途径。不足的是,腓骨截取会造成不同程度的肢体短缩,但大部分患者都能够通过功能锻炼得到良好的康复。
| [1] | JAIN A K, SINHA S. Infected nonunion of the long bones[J]. Clin Orthop Relat Res, 2005(431): 57–65. |
| [2] | CASTILLO R C, BOSSE M J, MACKENZIE E J, PATTERSON B M; LEAP Study Group. Impact of smoking on fracture healing and risk of complications in lamb threatening open tibia fractures[J]. J Orthop Trauma, 2005, 19: 151–157. DOI: 10.1097/00005131-200503000-00001 |
| [3] | AUDIGÉ L, GRIFFIN D, BHANDARI M, KELLAM J, RVEDI T P. Path analysis of factors for delayed healing and nonunion in 416 operatively treated tibial shaft fractures[J]. Clin Orthop Relat Res, 2005, 438: 221–232. |
| [4] | BHANDARI M, TORNETTA P 3rd, SPRAGUE S, NAJIBI S, PETRISOR B, GRIFFITH L, et al. Predictors of reoperation following operative management of fractures of the tibial shaft[J]. J Orthop Trauma, 2003, 17: 353–361. DOI: 10.1097/00005131-200305000-00006 |
| [5] | PHIEFFER L S, GOULET J A. Delayed unions of the tibia[J]. Instr Course Lect, 2006, 55: 389–401. |
| [6] | CLANCEY G J, WINQUIST R A, HANSEN S T Jr. Nonunion of the tibia treated with Kuntscher intramedullary nailing[J]. Clin Orthop Relat Res, 1982, 167: 191–196. |
| [7] | ALKHAWASHKI H M. Shock wave therapy of fracture nonunion[J]. Injury, 2015, 46: 2248–2252. DOI: 10.1016/j.injury.2015.06.035 |
| [8] | BUEHOLZR W. 洛克伍德-格林成人骨折[M]. 北京: 人民军医出版社, 2009: 1706-1767. |
| [9] | CLEVELAND K B. Delayed union and nonunion of fractures[M]. Philadelphia: Mosby, 2013: 59. |
| [10] | LE NAIL L R, STANOVICI J, FOURNIER J, SPLINGARD M, DOMENECH J, ROSSET P. Percutaneous grafting with bone marrow autologous concentrate for open tibia fractures:analysis of forty three cases and literature review[J]. Int Orthop, 2014, 38: 1845–1853. DOI: 10.1007/s00264-014-2342-x |
| [11] | LAVELLE D G. Delayed union and nonunion of fractures:Campbell's operative orthopaedics[M]. Louis: Mosby, 1998: 2579-2629. |
| [12] | TEITZ C C, DENNIS R C, FRANKEL V H. Problems associatedwith tibial fractures with intact fibulae[J]. J Bone Joint Surg Am, 1980, 62: 770–776. DOI: 10.2106/00004623-198062050-00011 |
| [13] | DUJARDYN J, LAMMENS J. Treatment of delayed union or non-union of the tibial shaft with partial fibulectomy and an Ilizarov frame[J]. Acta Orthop Belg, 2007, 3: 630–634. |
| [14] | THOMAS K A, HARRIS M B, WILLIS M C, LU Y, MACEWEN G D. The effects of the interosseous membrane and partial fibulectomy on loading of the tibia:a biomechanical study[J]. Orthopedics, 1995, 18: 373–383. |
| [15] | THOMAS K A, BEARDEN C M, GALLAGHER D J, HINTON M A, HARRIS M B. Biomechanical analysis of nonreamed tibial intra-medullary nailing after simulated transverse fracture andfibulectomy[J]. Orthopedics, 1997, 20: 51–57. |
| [16] | ABADIE B, LEAS D, CANNADA L, MALM P, MORWOOD M, HOWES C, et al. Does screw configuration or fibular osteotomy decrease healing time in exchange tibial nailing?[J]. J Orthop Trauma, 2016, 30: 622–626. DOI: 10.1097/BOT.0000000000000647 |
| [17] | OLERUD C, MOLANDER H. A scoring scale for symptom evaluation after ankle fratue[J]. Arch Orthop Trauma Surg, 1984, 103: 190–194. DOI: 10.1007/BF00435553 |
| [18] | TALL M, BONKOUNGOU D, SAWADOGO M, DA S C, TOE M F. Treatment of nonunion in neglected long bone shaft fractures by osteoperiosteal decortication[J]. Orthop Traumatol Surg Res, 2014, 100(6 Suppl): S299–S303. |
| [19] | SUGAYA H, MISHIMA H, AOTO K, LI M, SHIMIZU Y, YOSHIOKA T, et al. Percutaneous autologous concentrated bone marrow grafting in the treatment for nonunion[J]. Eur J Orthop Surg Traumatol, 2014, 24: 671–678. DOI: 10.1007/s00590-013-1369-9 |
| [20] | NIU Y, BAI Y, XU S, LIU X, WANG P, WU D, et al. Treatment of lower extremity long bone nonunion with expandable intramedullary nailing and autologous bone grafting[J]. Arch Orthop Trauma Surg, 2011, 131: 885–891. DOI: 10.1007/s00402-010-1226-9 |
| [21] | PATIL S, MONTGOMERY R. Management of complex tibial and femoral nonunion using the Ilizarov technique and its cost implications[J]. J Bone Joint Surg Br, 2006, 88: 928–932. |
| [22] | HEPPENSTALL R B. The present role of bone graft surgery in treating nonunion[J]. Orthop Clin North Am, 1984, 15: 113–123. |
| [23] | SCHMIDT A H, FINKEMEIER C G, TORNETTA P 3rd. Treatment of closed tibial fractures[J]. Instr Course Lect, 2003, 52: 607–622. |
| [24] | BRINKER M R, O'CONNOR D P. Current concepts review:exchange nailing of ununited fractures[J]. J Bone Joint Surg Am, 2007, 89: 177–188. |
| [25] | YE J, ZHENG Q L. Augmentative locking compression plate fixation for the management of long bone nonunion after intramedullary nailing[J]. Arch Orthop Trauma Surg, 2012, 32: 937–940. |
| [26] | ATESCHRANG A, ALBRECHT D, STÖCKLE U, WEISE K, STUBY F, ZIEKER D. High success rate for augmentation compression plating leaving the nail in situ for aseptic diaphyseal tibial nonunions[J]. J Orthop Trauma, 2013, 27: 145–149. DOI: 10.1097/BOT.0b013e31825d01b2 |
| [27] | VAUGHN J, GOTHA H, COHEN E, FANTRY A J, FELLER R J, VAN METER J, et al. Nail Dynamization for delayed union and nonunion in femur and tibia fractures[J/OL]. Orthopedics, 2016, 39:e1117-e1123. doi:10.3928/01477447-20160819-01. |
| [28] | HSIAO C W, WU C C, SU C Y, FAN K F, TSENG I C, LEE P C. Exchange nailing for aseptic tibial shaft nonunion:emphasis on the influence of a concomitant fibulotomy[J]. Chang Gung Med J, 2006, 29: 283–290. |
| [29] | SWANSON E A, GARRARD E C, O'CONNOR D P, BRINKER M R. Results of a systematic approach to exchange nailing for the treatment of aseptic tibial nonunions[J]. J Orthop Trauma, 2015, 29: 28–35. DOI: 10.1097/BOT.0000000000000151 |
| [30] | TSANG S T, MILLS L A, FRANTZIAS J, BAREN J P, KEATING J F, SIMPSON A H. Exchange nailing for nonunion of diaphyseal fractures of the tibia:our results and an analysis of the risk factors for failure[J]. Bone Joint J, 2016, 98-B: 534–541. DOI: 10.1302/0301-620X.98B4.34870 |
| [31] | CHEN S B, ZHANG C Q, JIN D X, CHENG X G, SHENG J G, ZENG B F. Treatment of aseptic nonunion after intramedullary nailing fixation with locking plate[J]. Orthop Surg, 2009, 1: 258–263. DOI: 10.1111/os4.2009.1.issue-4 |
| [32] | EL-ROSASY M A, EL-SALLAKH S A. Distal tibial hypertrophic nonunion with deformity:treatment by fixator-assisted acute deformity correction and LCP fixation[J]. Strat Traum Limb Recon, 2013, 8: 31–35. DOI: 10.1007/s11751-012-0150-7 |
 2017, Vol. 38
2017, Vol. 38


