髋臼骨折属于高能量损伤,主要发生于交通事故和高处坠落伤,据文献报道欧美国家每1万人中就有37例发生骨盆骨折,其中髋臼骨折占10%,病死率达5%~20%,切开复位内固定是主要的手术方式,但手术致残率高达50%~60%[1-2]。由于骨盆解剖结构复杂,髋臼位置较深,且有重要的神经血管通过,手术处理比较棘手。随着骨科医师对骨盆解剖认识程度的加深以及内固定器械的发展,简单髋臼骨折处理比较容易,但对于复杂髋臼骨折,如T型骨折、后壁伴横型骨折、双柱骨折等,手术处理仍较困难。对于如何实施后柱骨折块及方行区骨块的有效固定,目前手术多采用两种或以上入路,手术时间长、出血多,术后恢复慢,可发生早期伤口感染、静脉血栓和晚期创伤性关节、异位骨化等并发症[3-4]。因此,采用单一的手术入路运用内固定有效固定复杂髋臼骨折、减少手术并发症、促进髋关节功能康复一直是骨科医师追求的方向之一。
临床研究发现,对于比较简单的后柱复杂髋臼骨折,如T型骨折、前壁或前柱伴横行骨折和部分双柱骨折,可以在单一前入路钢板固定前柱骨折的同时直视髂窝下方形区骨块,通过间接复位后柱骨折,平行于方形区方向植入2枚拉力螺钉,临床固定效果确切[5-6]。但早期站立位非完全负重下地是否影响该种内固定的稳定性,目前尚不明确,且相关研究报道较少。为扩大单一前入路手术适应证,本研究通过尸体生物力学对两种内固定方式固定稳定性进行比较分析,评价前柱钢板联合后柱拉力螺钉固定复杂髋臼骨折的稳定性和有效性。
1 材料和方法 1.1 完整骨盆的选择经甲醛溶液防腐处理的大小相似的健康成年男性骨盆标本6具,死亡年龄分别为41、36、53、55、61、65岁,平均(52±10)岁。经X线片和CT检查证实无代谢性骨病及肿瘤等骨骼系统的疾病。选取完整骨盆及与之相连的股骨部分,解剖时保留从L4到股骨近端约30 cm的部分。去除多余的肌肉组织,保留下腰椎的前纵韧带、棘间韧带、棘上韧带、骶髂骨间韧带、骶髂腹侧韧带、骶髂背侧韧带、骶棘韧带、骶结节韧带、耻骨联合韧带、双侧髋关节囊。留待实验时使用。
1.2 髋臼T型骨折模型建立与实验分组利用小摆锯分别离断髋臼前、后壁,并垂直向下离断髋臼,形成髋臼T型骨折模型(图 1A)。分别将右、左两侧模型采用锁定钢板联合后柱拉力螺钉(实验组)和双柱钢板(对照组)两种内固定方式进行固定(图 1B)。实验组:首先复位前柱骨折,按弓状线重建骨盆的连续性,将骨折块解剖复位后应用9孔重建锁定钢板固定,在直视下前柱钢板外缘平行方形区固定2枚4.5 mm半螺纹皮质骨螺钉,长度超过骨折线至少10 mm;对照组:左侧T型骨折模型在骨折块解剖复位后,应用同样的钢板螺钉固定前柱,后柱横断骨折,按照后柱的解剖外形将塑形好的2块重建锁定钢板固定后柱骨块(图 1C)。模型固定后均行X线和CT扫描。

|
图 1 髋臼T型骨折模型建立与分组内固定方式 Fig 1 Acetabular T fracture models and grouping internal fixation A: Illustration of acetabular T type fracture; B: Internal fixation (anterior view) of experimental and control groups and location diagram of steel plate and screw; C: Model was fixed by two reconstruction plates in control group (posterior view) |
1.3 髋臼骨折标本上标记点的设置
分别在实验组和对照组的髋臼骨折标本上设置标记点,在前柱的骨折线两侧设2对对称的标记点,于骨折线中垂线两侧分别记为1、2,在方形区分别记为3、4,在后柱分别记为5、6。示意图见图 2。

|
图 2 髋臼骨折标本上设置标记点的示意图 Fig 2 Schematic diagram of mark points on acetabular fracture specimens A: Anterior column; B: Quadratus area; C: Posterior column. 1-6 are the marking points |
1.4 纵向移位和剪切刚度的生物力学测量
如图 3所示,参考Sawaguchi等[7]的研究模拟人体双下肢直立位,用自制标本固定夹固定股骨近端1/3处,使骨盆处于双足直立位,股骨干内收15°,并保持内旋5°~10°。将固定好的标本依次放入数字控制DDL20生物力学试验机上,以10 mm/min的速度加载负荷,从0 N开始加载至1 500 N,约为体质量70 kg的正常人站立位时所承受的静态应力,并维持30 s。每具标本循环加载7次,首次加载使标本达到机械性与弹性适应性平衡,不记录数据。记录接下来的6次数据并进行统计分析。纵向位移的测量利用上海大学力学实验室自主设计研发的数字图像测量系统,图像测量的基本原理是传感器将被测对象转换成计算机可识别的图像信号,再由计算机对图像的边缘纹理等特征进行处理并提取参数,从而达到测量的目的[8]。然后根据测量数据计算每对标记点的纵向移位(该对的两个标记点之间垂直距离在加载负荷前后的变化值)。纵向位移测试完成后持续加载,记录2组内固定失效的载荷,将骨折纵向移位大于>3 mm定义为内固定失效。根据公式计算剪切刚度(EF):EF=P/ΔL,其中P为载荷,ΔL为纵向移位,计算出两组在人体正常载荷600 N时的剪切刚度。内固定的剪切刚度是指轴向载荷下内固定抵抗形变保持关节稳定的能力,剪切刚度越大内固定抗形变能力越强,髋关节越稳定,说明内固定对骨折的把持力越强,即内固定越牢靠。

|
图 3 骨盆标本固定加载 Fig 3 Fixation and loading of pelvic specimens |
1.5 统计学处理
应用SPSS 19.0软件进行统计分析。服从正态分布且方差齐性的计量资料用x±s表示,两组间比较采用t检验。检验水准(α)为0.05。
2 结果 2.1 一般情况两组T型骨折固定后,前后柱骨折稳定,骶结节韧带、骶棘韧带及闭孔内肌韧带绷紧有力,X线片及CT检查示骨折复位、螺钉未入关节腔。在多次实验加载过程中均未发生骨折或内固定松动、拔出或断裂。
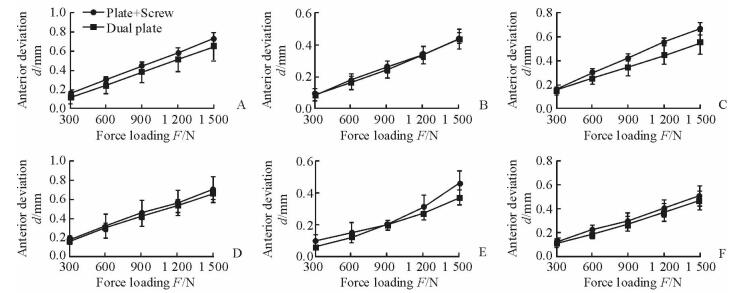
2.2 载荷与纵向移位的关系由图 4可见,随着载荷由300 N增加到1 500 N,两组髋臼骨折线两侧6对标记点纵向移位逐渐增加。不同载荷下两组各对标记点纵向移位比较差异均无统计学意义(P均>0.05)。两组最大移位均未超过1 mm,因此,两种固定方式都可以提供稳定、有效的固定,满足骨折固定的要求。
|
图 4 不同载荷-标记点纵向移位 Fig 4 Longitudinal displacement of different marking points A-F are marking points 1-6, respectively. n=6, x±s |
2.3 剪切刚度与内固定稳定性
本研究结果显示实验组和对照组内固定的剪切刚度分别为(1 428±57)和(1 621±62) N/mm,实验组剪切刚度小于对照组,但两组差异无统计学意义(P>0.05)。
3 讨论髋臼是人体最重要的杵臼关节,解剖结构特殊,具有重要的生理功能,骨折后使股骨头与髋臼之间的接触面积和应力等关系发生改变,加上髋臼位置较深,骨性结构不规则,手术治疗难度较大。Letournel和Judet[9]根据髋臼特点将髋臼骨折分为两类:简单髋臼骨折和复杂髋臼骨折。切开复位内固定是治疗复杂髋臼骨折的金标准,可允许患者早期功能锻炼,从而避免二期关节置换。骨折解剖复位直接影响关节功能预后,有效复位可减少创伤性关节炎的发生概率[10-11]。髋臼骨折术后创伤性关节炎的发生率高达20%,影像和临床结果与骨折的复位程度密切相关,如果髋臼骨折术后移位少于2 mm,绝大部分患者能获得满意的影像学表现与关节功能,如果骨折移位超过2 mm,仅66.67%的患者功能满意[12]。
髋臼骨折移位如果不能得到有效复位和固定,必然导致预后较差。近来开展的系列研究也通过髋臼生物力学来评价内固定方式的有效性和稳定性。Kistler等[13]报道应用不同的钢板固定髋臼T型骨折,通过生物力学评价内固定的稳定性,结果显示钢板固定的稳定性与其他方式差异无统计学意义。Zhang等[14]对比研究了普通拉力螺钉、拉力螺钉辅助普通重建钢板、拉力螺钉辅助锁定钢板固定髋臼后壁骨折,结果3种固定方式的稳定性相似。Zha等[15]生物力学研究证实多方向的钛板与附加拉力螺钉固定髋臼四边体骨折,其力学稳定可靠。
我们应用锁定钢板联合后柱拉力螺钉固定T型髋臼骨折,鉴于目前锁定钢板和断端加压螺钉是固定髋臼骨折最常用的内固定方式,且普通加压螺钉很早被用于固定髋臼骨折[16],另外,应用螺钉的好处在于不需要切开暴露即可做到有效固定。Im等[17]报道15例应用单独加压螺钉治疗髋臼粉碎性骨折的患者中,14例(93%)疗效满意。蔡贤华等[18]利用前入路的优势,采用前路钢板加方形区螺钉治疗髋臼骨折取得满意疗效。Gras等[19]比较了3种不同拉力螺钉与钢板治疗髋臼前柱骨折的效果,螺钉与钢板能取得同样的稳定性,但应用钢板附加拉力螺钉固定前后柱骨折的患者,术后功能康复期间生理负荷下早期站立位影响其稳定性,生物力学方面尚未见报道。本研究中,我们在同一具标本的一侧应用双柱钢板,另一侧应用锁定钢板联合后柱拉力螺钉固定,在生理载荷从首次300 N加载到1 500 N过程中髋臼骨折线的纵向移位均未超过1 mm,与Marintschev等[20]的研究结果较为相近。我们之所以选取1 500 N载荷加载,是因为该负荷大约相当于70 kg健康人体质量的2倍,模拟了单足站立时的负荷,即人在康复锻炼时如坐立在床或扶拐部分负重最大的负荷。单一的前柱钢板联后柱合拉力螺钉治疗髋臼骨折,力学性能可靠,稳定性与传统双柱钢板接近。
髋臼骨折的传统入路手术创伤大,并发症多,不利于患者的功能康复[21-24], 通过单一或微创的手术入路实现髋臼骨折的稳定固定是未来发展的方向。本研究通过生物力学实验证实采用前柱钢板联合后柱拉力螺钉内固定治疗复杂髋臼骨折,早期生理负荷站立位并不影响内固定的可靠性,该固定方式能有效维持复位后骨折对位,并防止再移位,扩大了前入路治疗复杂髋臼骨折的适应证,为临床前入路固定复杂髋臼骨折提供了理论参考。
| [1] | MAUFFREY C, HAO J, CUELLAR D O 3rd, HERBERT B, CHEN X, LIU B, et al. The epidemiology and injury patterns of acetabular fractures:are the USA and China comparable?[J]. Clin Orthop Relat Res, 2014, 472:3332-3337. |
| [2] | MAGALA M, POPELKA V, BOŽÍK M, HEGER T, ZAMBORSK Ý V, ŠIMKO P. [Conservative treatment of acetabular fractures:epidemiology and medium-term clinical and radiological results][J]. Acta Chir Orthop Traumatol Cech, 2015, 82: 51–60. |
| [3] | EL-KHADRAWE T A, HAMMAD A S, HASSAAN A E. Indicators of outcome after internal fixation of complex acetabular fractures[J]. Alex J Med, 2012, 48: 99–107. DOI: 10.1016/j.ajme.2011.12.005 |
| [4] | JEFFCOAT D M, CARROLL E A, HUBER F G, GOLDMAN A T, MILLER A N, LORICH D G, et al. Operative treatment of acetabular fractues in an older population through a limited ilioinguinal approach[J]. J Orthop Trauma, 2012, 26: 284–289. DOI: 10.1097/BOT.0b013e31821e10a2 |
| [5] | ANDERSEN R C, O'TOOLE R V, NASCONE J W, SCIADINI M F, FRISCH H M, TUREN C W. Modified stoppa approach for acetabular fractures with anterior and posterior column displacement:quantification of radiographic reduction and analysis of interobserver variability[J]. J Orthop Trauma, 2010, 24: 271–278. DOI: 10.1097/BOT.0b013e3181b2b4ca |
| [6] | SAGI H C, AFSARI A, DZIADOSZ D. The anterior intra-pelvic (modified rives-stoppa) approach for fixation of acetabular fractures[J]. J Orthop Trauma, 2010, 24: 263–270. DOI: 10.1097/BOT.0b013e3181dd0b84 |
| [7] | SAWAGUCHI T, BROWN T D, RUBASH H E, MEARS D C. Stability of acetabular fractures after internal fixation. A cadaveric study[J]. Acta Orthop Scand, 1984, 55: 601–605. DOI: 10.3109/17453678408992404 |
| [8] | ZHANG D, LUO M, AROLA D D. Displacement/strain measurements using an optical microscope and digital image correlation[J]. Opt Eng, 2006, 45: 535–545. |
| [9] | LETOURNEL E, JUDET R. Fractures of the acetabulum[M]. 2nd ed. New York: Springer-Verlag, 1993. |
| [10] | BAUMGAERTNER M R. Fractures of the posterior wall of the acetabulum[J]. J Am Acad Orthop Surg, 1999, 7: 54–65. DOI: 10.5435/00124635-199901000-00006 |
| [11] | MATTA J M. Fractures of the acetabulum:accuracy of reduction and clinical results in patients managed operatively within three weeks after the injury[J]. J Bone Joint Surg Am, 1996, 78: 1632–1645. DOI: 10.2106/00004623-199611000-00002 |
| [12] | MITSIONIS G I, LYKISSAS M G, MOTSIS E, MITSIOU D, GKIATAS I, XENAKIS T A, et al. Surgical management of posterior hip dislocations associated with posterior wall acetabular fracture:a study with a minimum follow-up of 15 years[J]. J Orthop Trauma, 2012, 26: 460–465. DOI: 10.1097/BOT.0b013e31822c4d6c |
| [13] | KISTLER B J, SMITHSON I R, COOPER S A, COX J L, NAYAK A N, SANTONI B G, et al. Are quadrilateral surface buttress plates comparable to traditional forms of transverse acetabular fracture fixation?[J]. Clin Orthop Relat Res, 2014, 472: 3353–3361. DOI: 10.1007/s11999-014-3800-x |
| [14] | ZHANG Y, TANG Y, WANG P, ZHAO X, XU S, ZHANG C. Biomechanical comparison of different stabilization constructs for unstable posterior wall fractures of acetabulum. A cadaveric study[J/OL]. PLoS One, 2013, 8:e82993. doi:10.1371/journal.pone.0082993. |
| [15] | ZHA G C, SUN J Y, DONG S J, ZHANG W, LUO Z P. A novel fixation system for acetabular quadrilateral plate fracture:a comparative biomechanical study[J/OL]. Biomed Res Int, 2015, 2015:391032. doi:10.1155/2015/391032. |
| [16] | MOUHSINE E, GAROFALO R, BORENS O, WETTSTEIN M, BLANC C H, FISCHER J F, et al. Percutaneous retrograde screwing for stabilisation of acetabular fractures[J]. Injury, 2005, 36: 1330–1336. DOI: 10.1016/j.injury.2004.09.016 |
| [17] | IM G I, SHIN Y W, SONG Y J. Fractures to the posterior wall of the acetabulum managed with screws alone[J]. J Trauma, 2005, 58: 300–303. DOI: 10.1097/01.TA.0000149329.86361.CE |
| [18] | 蔡贤华, 刘曦明, 汪国栋, 徐峰, 王华松, 李世梁, 等. 前路铁板结合方形区螺钉内固定治疗涉及方形区的髓臼骨折[J]. 中华创伤骨科杂志, 2013, 15: 102–106. DOI: 10.3760/cma.j.issn.1671-7600.2013.02.003 |
| [19] | GRAS F, MARINTSCHEV I, SCHWARZ C E, HOFMANN G O, POHLEMANN T, CULEMANN U. Screw-versus plate-fixation strength of acetabular anterior column fractures:a biomechanical study[J]. J Trauma Acute Care Surg, 2012, 72: 1664–1670. DOI: 10.1097/TA.0b013e3182463b45 |
| [20] | MARINTSCHEV I, GRAS F, SCHWARZ C E, POHLEMANN T, HOFMANN G O, CULEMANN U. Biomechanical comparison of different acetabular plate systems and constructs-the role of an infra-acetabular screw placement and use of locking plates[J]. Injury, 2012, 43: 470–474. DOI: 10.1016/j.injury.2011.11.009 |
| [21] | AIGNER R, HELLIGE R, KNIPPEL S, OBERKIRCHER L, RUCHHOLTZ S, BUECKING B. Internal fixation of acetabular fractures in an older population using the TIMI approach-midterm results of a prospective study[J]. Injury, 2017, 48: 890–896. DOI: 10.1016/j.injury.2017.02.001 |
| [22] | HAMMAD A S, EL-KHADRAWE T A, WALY A H, ABU-SHEASHA G A. The efficacy of posterior plating and anterior column screw fixation in the management of T-shaped acetabular fractures-CART analysis of prospective cohort study[J]. Injury, 2017, 48: 680–686. DOI: 10.1016/j.injury.2017.01.024 |
| [23] | XUE Z, QIN H, DING H, AN Z. A novel approach for treatment of acetabular fractures[J]. Med Sci Monit, 2016, 122: 3680–3688. |
| [24] | OH H K, CHOO S K, KIM J J, LEE M. Stoppa approach for anterior plate fixation in unstable pelvic ring injury[J]. Clin Orthop Surg, 2016, 8: 243–248. DOI: 10.4055/cios.2016.8.3.243 |
 2017, Vol. 38
2017, Vol. 38


