颅内自发性椎动脉夹层(VADAs)是青年人和中年人自发性蛛网膜下隙出血或后循环脑卒中的原因之一[1, 2],且近年来发病率有上升趋势,逐渐成为临床研究的热点。目前临床针对VADAs的治疗方法主要包括外科手术治疗、闭塞载瘤动脉和支架辅助弹簧圈血流重建治疗等,其中对于支架辅助弹簧圈进行血流重建治疗未破裂椎动脉夹层动脉瘤的可行性和安全性仍有争议。2009年6月到2014年3月我院对38例VADAs患者采用多支架血流重建性治疗,获得较好疗效,总结了一些经验,现报告如下,供同行参考。 1 资料和方法 1.1 研究对象
2009年6月到2014年3月所有接受多支架血流重建性治疗的VADAs患者。所有研究对象均符合以下纳入标准:(1)症状性椎动脉未破裂夹层动脉瘤(uis-VADAs),并且被脑血管造影(DSA)证实;(2)初次治疗采用2枚或2枚以上支架辅助弹簧圈重构血管。排除标准:(1)急性外伤性或者医源性病史;(2)破裂椎动脉夹层动脉瘤(ris-VADAs);(3)颅外V3段或基底动脉的病变;(4)初次治疗采用闭塞载瘤动脉的方法;(5)颅内双侧uis-VADAs,并且接受了多种治疗方法;(6)失随访患者。共38例VADAs患者纳入本研究,男31例,女7例,年龄26~75岁,中位年龄48岁。 诊断标准:DSA检查提示椎动脉主干有向外的梭型或半梭型扩张,伴或不伴椎动脉狭窄,则VADAs的诊断成立。 1.2 治疗过程
经DSA证实为未破裂椎动脉夹层动脉瘤。术前3d服用抗血小板药物(阿司匹林100mg/d,氯吡格雷75mg/d)行药物准备。治疗当天,按80U/kg给予肝素,经动脉行全身肝素化。此后每小时给药量减半,至1250U时,予1250U/h维持给药。所有患者均采用全麻施行手术,以保证手术过程顺利进行。支架完全打开,并且覆盖病变所在部位上下超过5mm,则该支架被认为释放成功。支架能否放置成功主要基于术者经验、受累部位、对侧血管的解剖特点。2011年2月前,术后予低分子肝素抗凝3d,同时使用阿司匹林300mg/d抗凝6个月,氯吡格雷75mg/d抗凝6周,6个月后根据造影复查结果进行药物调整,若无支架内狭窄或血栓形成,则改为阿司匹林100mg/d,终生服用。2011年2月后,术后不再常规使用低分子肝素抗凝,而是直接服用双联抗血小板药物(阿司匹林100mg/d+氯吡格雷75mg/d)6周,然后改为服用单一抗血小板药物(阿司匹林100mg/d),终生服用。 1.3 随访方法和评价指标
影像学随访依照传统方法,采用头颅磁共振血管造影(MRA)或者DSA。MRA首次复查时间为术后3个月,DSA为术后6个月,之后每年复查1次。术后即刻栓塞程度包括:完全栓塞、次全栓塞、部分栓塞。复查结果依据影像学检查分为:治愈、改善、稳定、复发。其中,治愈是指瘤体不显影;改善指部分栓塞的病变内血栓进一步形成;稳定指与术后即刻比较无明显差异;复发指与术后即刻相比动脉瘤显影部分较前增大。临床结果以改良Rankin评分(mRS)进行评估,依据最后一次随访的结果被分为预后良好(mRS0~1)和预后不良(mRS2~6)。
2 结 果 2.1 临床疗效
所有病变均采用多支架血流重建性治疗,支架释放成功率为100%。患者临床特征详见表 1。术后即刻栓塞结果:8例完全栓塞,7例次全栓塞,23例部分栓塞。术中无血栓形成。影像学随访结果:38例患者中,1例(2.6%,1/38)发生缺血事件(图 1)。8例完全栓塞和7例次全栓塞复查结果为影像学治愈。23例部分栓塞中,有9例影像学治愈,6例改善,8例稳定。其中,2例患者初次治疗在外院进行,来我院行再次治疗,治疗后6个月复查结果为稳定。临床随访结果:术后随访19个月(4~126个月),无患者死亡。
|
|
表 1 38例未破裂椎动脉夹层动脉瘤患者的临床特征 Tab 1 Clinical characteristics of 38 patients with un-ruptured vertebral artery dissection aneurysm |
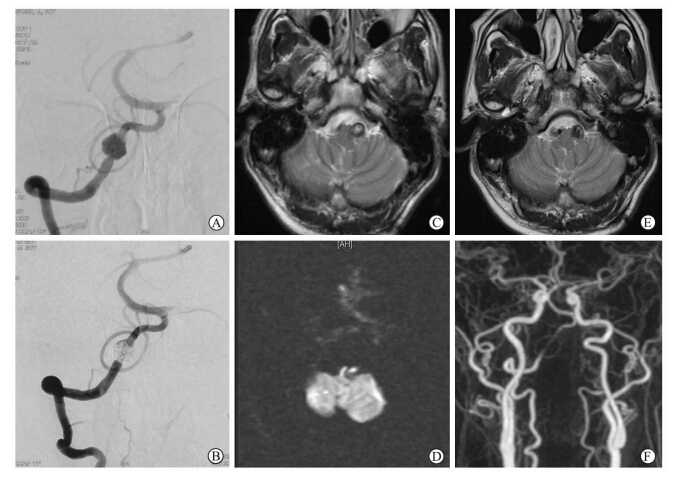 | 图 1 多支架治疗术后发生缺血事件的椎动脉夹层患者影像资料 Fig 1 Postoperative ischemic event after treated by reconstructive treatment with multiple stents and coiling n 80-year-old male patient,suffering from repeated dizziness for two weeks,was admitted. A: Right vertebral artery dissection along with occlusion of the left vertebral artery was revealed by DSA; B: Partial obliteration was gained immediately after four solitaire stents and coiling was used to embolize the aneurysm and reconstruct the parent artery; C,D : Cranial MRI examination showed acute infarction in the right cerebellum; E,F: 3 months later,cranial MRA examination displayed no new infarction,with disappeared symptoms |
51岁男性患者,因“头痛2周”至当地医院就诊,行头颅MRI检查发现右侧椎动脉夹层动脉瘤可能,遂至我中心治疗,DSA确诊为右侧椎动脉夹层动脉瘤(图 2A、2B),使用3枚Enterprise支架+弹簧圈行血管重建性治疗,术后即刻治疗结果为部分栓塞(图 2C、2D)。6个月后行DSA复查,显示影像学治愈,动脉瘤不显影(图 2E、2F)。
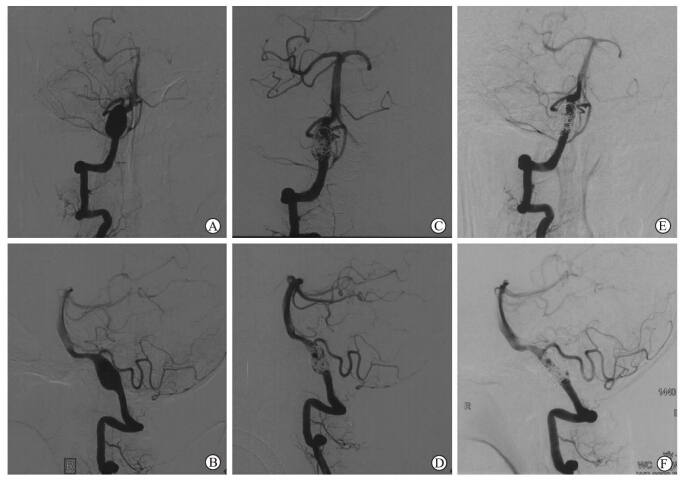 | 图 2 采用3枚重叠支架联合弹簧圈治疗的典型未破裂椎动脉夹层动脉瘤患者影像资料 Fig 2 R-UVADA treated with three overlapping stents and coiling A 51-year-old patient was admitted due to headache for two weeks. Right-unruptured vertebral artery dissection aneurysm (A,B) was revealed,with right posterior inferior cerebellar artery involved. Partial obliteration was gained immediately after three stents and coiling was used to embolize the aneurysm and reconstruct the parent artery(C,D). Complete obliteration was showed by 6-month follow-up angiography |
VADAs越来越多地被诊断为自发性蛛网膜下隙出血或后循环脑卒中的原因,特别是青年人和中年人[1, 2]。造影发现椎动脉主干发生囊样扩张时,提示夹层动脉瘤形成,未来可能会导致致命性的出血风险[3]。出血急性期时,进行外科手术常有较高的致残率和死亡率[4]。目前,治疗未破裂椎动脉夹层动脉瘤的方法有闭塞载瘤动脉和多支架辅助血流重建。牺牲载瘤动脉来填塞动脉瘤的方法,常被用来治疗复发风险较高的VADAs[5, 6]。尽管大多数椎动脉夹层动脉瘤可以采用单支架辅助弹簧圈栓塞或闭塞载瘤动脉的方法治疗,但术后缺血和再出血事件仍时有发生[7, 8, 9]。而且,对于那些伴对侧椎动脉闭塞、对侧椎动脉夹层动脉瘤、累及小脑后下动脉(PICA)的病变,闭塞载瘤动脉的方法并不适用。除此之外,闭塞载瘤动脉可能会导致对侧椎动脉形成夹层动脉瘤或前循环形成动脉瘤;一旦对侧或前循环的血管发生狭窄或者闭塞,闭塞载瘤动脉的治疗方法将会导致丧失一条可用的代偿途径。
随着颅内支架技术的不断发展[10],血流重建性治疗被越来越多地应用于急性症状性夹层动脉瘤患者,并且有望成为代替闭塞载瘤动脉的选择[11, 12, 13]。考虑到术后复发和出血,闭塞载瘤动脉的治疗方法可能适用于那些需要完全阻止出血的患者。但是,缺血事件可能因此而发生,特别是在病变累及PICA或病变血管为基底动脉主供血动脉的情况下。尽管单支架治疗是一个很有希望的选择[14],但并不能完全阻止病灶复发、出血的可能[15]。
多个重叠支架的应用相比单支架确实提高了栓塞即刻的动脉瘤栓塞程度,降低了术后复发率[16, 17, 18]。在长期随访的过程中,多支架辅助弹簧圈重建的患者发生再出血和影像学复发的概率较低。即使是部分栓塞的患者,也未发生。而且,我中心前期研究结果显示,单支架治疗后复发的患者,再次置入1枚或多枚支架,也可明显改善预后[18]。这些发现提示多支架辅助弹簧圈进行血流重建比单支架治疗能更有效地预防复发。其原因可能如下:首先,支架相关的良性血流动力学改变有助于阻止弹簧圈压缩,动脉瘤破裂和增长。其次,这些有利的血流动力学改变的比例与支架的数目成正比。重叠支架可有助于降低支架网孔的直径,提高金属覆盖率,加强载瘤动脉的强度,并且有利于载瘤动脉塑形。因此,本中心在以下情况下更愿意采用多支架技术血流重建来治疗VADAs:(1)单支架联合弹簧圈或不用弹簧圈治疗后结果为部分栓塞;(2)累及PICA的病变,特别是对侧PICA缺如或前循环发育不良的患者;(3)对侧同样有椎动脉夹层动脉瘤的患者;(4)对侧椎动脉发育不良或闭塞。
影像学随访显示:23例术后即刻栓塞结果为部分栓塞,7例为次全栓塞,8例为完全栓塞。其中,2例初次治疗在外院接受多支架辅助栓塞的病例,来我院后,再次放置了2枚LVIS支架,6个月复查结果分别为稳定和改善。当动脉瘤直径较大时,采用普通多支架重建治疗效果可能不理想,而且经济负担较重。采用我中心自主研发的Tubridge血流导向装置进行治疗,1例术后即刻治疗结果为次全栓塞,复查为治愈。另外1例术后即刻为部分栓塞,6个月后复查结果为治愈。
临床随访结果显示:100%预后良好(mRS,0~1)。1例发生可能与治疗相关的并发症(2.6%,图 1)。该男性患者因反复发作头晕2周入院,DSA提示左侧椎动脉完全闭塞,右侧椎动脉V4段未破裂夹层动脉瘤,累及PICA;术中使用了4枚Solitaire支架行血流重建,术后2d出现吞咽困难,行头颅MRI发现右侧椎动脉主干显影不清,右侧小脑半球点状新鲜梗死灶,提示可能有支架内血栓形成。严格行双联抗血小板药物治疗,3个月后行MRA复查提示右侧椎动脉通畅,吞咽困难症状明显好转。上述病例提示:当患者一侧椎动脉已经完全闭塞时,对侧椎动脉行血管重建性治疗,发生缺血事件的概率增大,需要引起重视。
综上所述,我们的初步经验显示应用多支架行血流重建性治疗VADAs安全可行,但对于对侧已经闭塞的uis-VADAs患者需谨慎,可能会导致术后缺血事件发生。受限于样本量较小,目前相关结论仍有待进一步的大样本研究证实。
4 利益冲突
所有作者声明本文不涉及任何利益冲突。
| [1] | Mizutani T, Aruga T, Kirino T, Miki Y, Saito I, Tsuchida T. Recurrent subarachnoid hemorrhage from untreated ruptured vertebra basilar dissecting aneurysms[J]. Neurosurgery, 1995, 36:905-911. |
| [2] | Arnold M, Bousser M G, Fahrni G, Fischer U, Georgiadis D, Gandjour J, et al. Vertebral artery dissection: presenting findings and predictors of outcome [J]. Stroke, 2006, 37:2499-2503. |
| [3] | Ro A, Kageyama N, Abe N, Takatsu A, Fukunaga T. Intracranial vertebral artery dissection resulting in fatal subarachnoid hemorrhage: clinical and histopathological investigations from a medico legal perspective[J]. J Neurosurg, 2009, 110:948-954. |
| [4] | Yamaura A, Watanabe Y, Saeki N. Dissecting aneurysms of the intracranial vertebral artery[J]. J Neurosurg, 1990, 72:183-188. |
| [5] | Peluso J P, van Rooij W J, Sluzewski M, Beute G N, Majoie C B.Endovascular treatment of symptomatic intradural vertebral dissecting aneurysms[J]. AJNR Am J Neuroradiol, 2008, 29:102-106. |
| [6] | Kurata A, Ohmomo T, Miyasaka Y, Fujii K, Kan S, Kitahara T. Coil embolization for the treatment of ruptured dissecting vertebral aneurysms[J]. AJNR Am J Neuroradiol, 2001, 22:11-18. |
| [7] | Yasui T, Kishi H, Komiyama M, Iwai Y, Yamanaka K, Nishikawa M, et al. Rerupture mechanism of ruptured intracranial dissecting aneurysm in the vertebral artery following proximal occlusion[J].No Shinkei Geka, 2000, 28:345-349. |
| [8] | Zhao W Y, Krings T, Alvarez H, Ozanne A, Holmin S, Lasjaunias P. Management of spontaneous haemorrhagic intracranial vertebrobasilar dissection: review of 21 consecutive cases[J].Acta Neurochir (Wien), 2007, 149:585-596. |
| [9] | Peluso J P, van Rooij W J, Sluzewski M, Beute G N, Majoie C B. Posterior inferior cerebellar artery aneurysms: incidence, clinical presentation, and outcome of endovascular treatment[J].AJNR Am J Neuroradiol, 2008, 29:86-90. |
| [10] | Krischek O, Miloslavski E, Fischer S, Shrivastava S, Henkes H. A comparison of functional and physical properties of self-expanding intracranial stents [Neuroform3, Wingspan, Solitaire, Leo+, Enterprise][J]. Minim Invasive Neurosurg, 2011, 54:21-28. |
| [11] | Kim B M, Shin Y S, Kim S H, Suh S H, Ihn Y K, Kim D I, et al. Incidence and risk factors of recurrence after endovascular treatment of intracranial vertebrobasilar dissecting aneurysms[J]. Stroke, 2011, 42:2425-2430. |
| [12] | Park S I, Kim B M, Kim D I, Shin Y S, Suh S H, Chung E C, et al. Clinical and angiographic follow-up of stent-only therapy for acute intracranial vertebrobasilar dissecting aneurysms[J]. AJNR Am J Neuroradiol, 2009, 30:1351-1356. |
| [13] | Kim M J, Chung J, Kim S L, Roh H G, Kwon B J, Kim B S, et al. Stenting from the vertebral artery to the posterior inferior cerebellar artery[J]. AJNR Am J Neuroradiol, 2012, 33:348-352. |
| [14] | Shin Y S, Kim H S, Kim S Y.Stenting for vertebrobasilar dissection: a possible treatment option for nonhemorrhagic vertebrobasilar dissection[J]. Neuroradiology, 2007, 49:149-156. |
| [15] | Taha M M, Sakaida H, Asakura F, Maeda M, Toma N, Yamamoto A, et al. Endovascular mariagement of vertebral artery dissecting aneurysms:review of 25 patients[J]. Turk Neurosurg, 2010, 20:126-135. |
| [16] | 方亦斌, 赵开军, 李 强, 许 奕, 洪 波, 黄清海, 等. 支架结合弹簧圈治疗破裂椎动脉夹层动脉瘤[J].中国微侵袭神经外科杂志, 2013, 18:145. |
| [17] | Zhao K J, Zhao R, Huang Q H, Xu Y, Hong B, Fang Y B, et al. The interaction between stent(s) implantation, PICA involvement, and immediate occlusion degree affect symptomatic intracranial spontaneous vertebral artery dissection aneurysm (sis-VADA) recurrence after reconstructive treatment with stent(s)-assisted coiling[J]. Eur Radiol, 2014, 24:2088-2096. |
| [18] | Zhao K J, Fang Y B, Huang Q H, Xu Y, Hong B, Li Q, et al. Reconstructive treatment of ruptured intracranial spontaneous vertebral artery dissection aneurysms: long-term results and predictors of unfavorable outcomes[J]. PLoS One, 2013, 8:e67169. |
 2015, Vol. 36
2015, Vol. 36


