2. 第二军医大学长海医院放射科, 上海 200433;
3. 第二军医大学长海医院血管外科, 上海 200433
2. Department of Radiology, Changhai Hospital, Second Military Medical University, Shanghai 200433, China;
3. Department of Vascular Surgery, Changhai Hospital, Second Military Medical University, Shanghai 200433, China
据美国癌症联合会最新报告,新诊断的肾癌病例中约3%~5%的患者同时伴有静脉癌栓[1]。尽管传统腹腔镜手术已经成为肾癌根治术的标准术式[2],但对于伴有静脉癌栓尤其是下腔静脉癌栓的肾癌病例,开放手术依然是首选手术方式[3]。达芬奇机器人辅助腹腔镜技术以其高清的视野、灵活的腕式运动等优点大大提高了腔镜手术的安全性和临床疗效,在泌尿外科前列腺癌根治术、肾部分切除术等手术中得到了广泛应用。2011年,美国学者Abaza率先报道了5例机器人辅助全腔镜下肾切除术+腔静脉取栓术,其中2例进行了腔静脉完全阻断下切开取栓[4],取得了初步成效。经第二军医大学长海医院医学伦理委员会批准,本课题组于2014年1月13日尝试完成了中国首例机器人辅助全腔镜下右肾癌根治切除+腔静脉Ⅱ级癌栓取出术,取得了一些经验,为其后续临床推广应用奠定了基础。 1 资料和方法 1.1 一般资料
患者女性,73岁,体质指数(body mass index,BMI) 20.4 kg/m2。美国东部肿瘤协作组(Eastern Cooperative Oncology Group,ECOG)体力状况评分1分。Charlson全身合并症评分(Age-weighted) 2分。麻醉评分(American Society of Anesthesiologists Score,ASA) 2分。因“右腰痛 伴肉眼血尿4个月”于2013年12月31日入院。CT检查提示:右肾癌伴下腔静脉癌栓,肿瘤大小4.9 cm× 4.7 cm,下腔静脉内癌栓长度4.6 cm。胸片、骨扫描ECT、PET-CT检查未发现远处转移病灶。术前行酪氨酸激酶抑制剂 (tyrosine kinase inhibition,TKI) 靶向药物治疗3个月。服药期间患者出现高血压,口服抗高血压药控制良好。服药结束后复查腹部增强CT提示:肿瘤大小4.3 cm×4.4 cm,下腔静脉内癌栓长度3.3 cm(图 1)。患者既往无腹盆腔手术史。术前2 d在数字减影血管造影(digital subtraction angiography,DSA)下行下腔静脉癌栓近心端滤器放置,并给予口服抗凝药治疗。手术备血5 000 mL。术前通过第二军医大学长海医院医学伦理委员会审批,签署书面手术知情同意书,充分告知患者及家属手术相关风险及中转开放手术的可能。

|
图 1 患者术前CTA检查及术中所见 Fig 1 CTA findings after targeted therapy and surgical confirmation during operation RA: Renal artery; RA’: Accessory renal artery; GV-TT: Gonadal vein tumor thrombus; IVC-TT: Inferior vena cava tumor thrombus. A,C,E,G: Surgical confirmation; B,D,F,H: CTA finding |
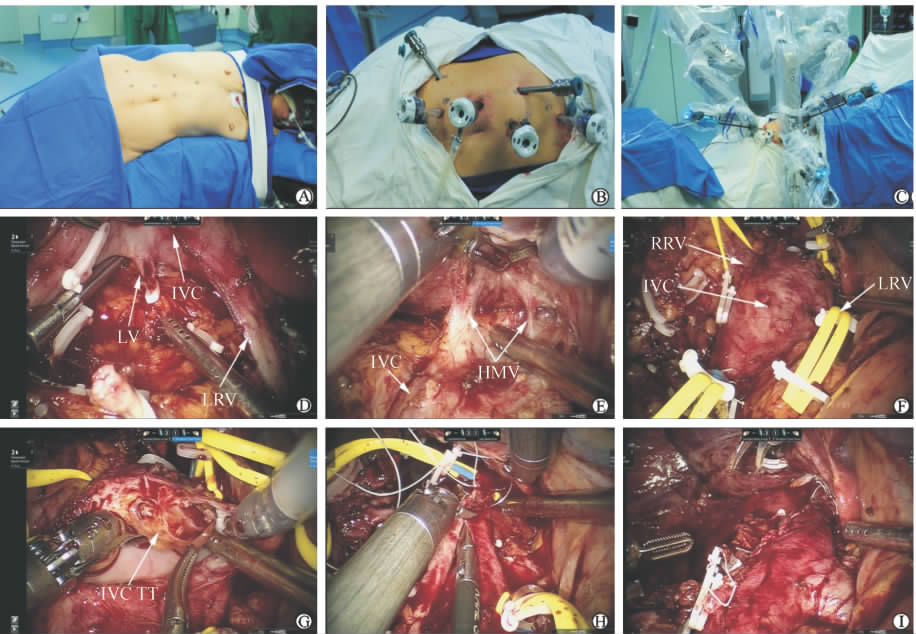
采用静吸复合全身麻醉,取健侧斜卧70°,腰部抬高,留置16F双腔导尿管。在右侧腹直肌外侧缘脐上2 cm处做1.5 cm皮肤切口,建立气腹,置入12 mm套管,直视下分别于右侧锁骨中线肋缘下1 cm、右侧髂前上棘上方2 cm处做1 cm切口,置入1、2号机械臂8 mm套管,再分别于前正中线脐上3 cm、8 cm及经右侧腹直肌脐下5 cm做1.2 cm切口,置入第1、2、3辅助孔套管,装配机械臂(图 2A~2C)。
扇形拉钩挡开肝脏,电剪刀分离并打开右侧结肠旁沟及结肠脾区,将升结肠及十二指肠翻至左侧,暴露右肾周筋膜,打开下腔静脉鞘,沿下腔静脉表面充分游离,见右侧生殖静脉明显增粗、僵硬,并在生殖静脉与下腔静脉之间见一异位肾动脉穿行(图 1B、1C)。向上游离至肝短静脉水平,并夹闭离断(图 2D),向左充分游离左肾静脉,在腔静脉与腹主动脉之间显露左肾动脉并夹闭(图 1A、1B)。于下腔静脉表面用hem-o-lok及钛夹夹闭并离断右侧生殖静脉,内见癌栓形成,癌栓可整体拽出(图 1D、1E、1F)。充分游离并夹闭离断下腔静脉深面腰静脉(图 2E)。充分游离肾脏并切除肾上腺,分离肾蒂血管周围组织,显露右肾静脉。使用血管吊带于癌栓头侧及尾侧环套下腔静脉,同样方法环套左右肾静脉。提拉血管吊带并以hem-o-lok固定依次阻断癌栓尾侧下腔静脉、左肾静脉、癌栓头侧下腔静脉(图 2F)。于右肾静脉根部纵行切开下腔静脉5 cm,完整取出下腔静脉内癌栓并切除部分与之粘连的右侧下腔静脉壁(图 2G),并连同右肾完整切除,5-0 CV线连续缝合关闭下腔静脉切口(图 2H),开放左肾静脉排出下腔静脉内气体后缝线打结,完全关闭下腔静脉(图 2I),并检查下腔静脉有无漏口,依次松开远心端及近心端血管吊带。彻底止血,取出标本,放置引流后逐层关闭切口。
|
图 2 患者术前器械固定及术中操作 Fig 2 Instrument configuration before operation and intraoperative maneuver A: Patient position; B,C: Trocar placement and instrument configuration; D: Lumbar veins (LV) dissection and ligation; E: Hepatic minor veins (HMV) dissection and ligation; F: Cross-clamping of inferior vena cava (IVC) and left renal vein (LRV); G: IVC tumor thrombectomy; H: IVC reconstruction; I: Unclamping and blood reperfusion |
手术顺利完成,手术时间363 min,下腔静脉共阻断47 min,术中出血1 200 mL,术中输血1 200 mL。术后第1天开始给予低分子肝素抗凝治疗。术后因血红蛋白(Hb)偏低(64.0 g/L)分别于手术当天输血600 mL,术后第5天输血400 mL,无其他手术并发症发生。术后第3天肠道恢复通气,引流管留置时间3 d,术后住院16 d。术后病理学检查提示:肾脏透明细胞癌,Fuhrman Ⅲ级,累及肾周及肾门脂肪,肾静脉及下腔静脉癌栓,肾上腺及输尿管未见癌组织,无淋巴结转移。术前及出院前血肌酐水平分别为68、88 μmol/L。患者出院后继续给予口服抗凝药及TKI靶向药物治疗。
3 讨 论 3.1 研究现况
肾脏肿瘤伴下腔静脉瘤栓因手术风险较高一直被列为腹腔镜手术的禁忌。2002年Fergany等[5]首次报道了普通腹腔镜下肾切除术+腔静脉切开取栓的动物实验手术。迄今为止,仅2006年由美国约翰霍普金斯医学中心Romero等[6]报道了1例完全普通腹腔镜下左肾切除术+腔静脉Ⅱ级癌栓切开取出术,但在该手术中癌栓位置较低,突入腔静脉内的长度约3 cm,术中用辛氏钳夹闭部分腔静脉后,在肾静脉入口处切开腔静脉后整体拽出瘤栓,并缝合腔静脉切口。对于传统腹腔镜技术在这一术式中的应用,其余报道均为腹腔镜下游离后行小切口开放手术取栓或手助腹腔镜手术[7,8,9]。借助达芬奇机器人外科手术系统在图像显示和机械运动方面的优势,泌尿外科医师开始追求全腔镜下肾切除术+腔静脉切开取栓术,在最大程度保证手术安全的同时,进一步提高操作准确性,减小手术创伤,将尖端的科学技术转化为患者的最终获益。 3.2 手术经验及注意事项
本研究尝试完成了中国首例达芬奇机器人辅助全腔镜下右肾切除+腔静脉Ⅱ级癌栓取出术,初步证实了该术式的可行性,取得了初步成效。结合既往文献及本例患者的经验,本研究从术前准备、术中操作技巧及术后处理等方面探讨达芬奇机器人全腔镜下肾切除+腔静脉Ⅱ级癌栓取出术的临床价值和注意事项。 3.2.1 术前准备
在术前准备方面,首先应充分评估患者一般情况、体力状态以及肿瘤分期。影像学检查用于评估肿瘤局部淋巴结转移情况,邻近器官侵犯情况,癌栓高度、有无侵犯腔静脉壁及远处转移病灶,对手术方案的制定具有十分重要的意义。核磁共振成像(magnetic resonance imaging angiography,MRA)被认为是检测腔静脉癌栓及范围的“金标准”,其敏感性可达90%~100%[10]。但是近年来多层螺旋CT的快速发展,大大提高了其在腔静脉癌栓检测中的价值,敏感性和特异性分别达到了93%和97%[11,12]。本例采用320排螺旋CT 0.5 mm薄层扫描,并可进行多平面重建,清楚地显示了腔静脉癌栓、生殖静脉癌栓和生长范围,以及肾血管等重要手术解剖细节和毗邻关系。有学者提出,无论是MRI还是CT,对于腔静脉癌栓的检测,更重要的不是采用哪种方法,而是检查时机的选择,最好应在术前2周内进行,因为一部分患者癌栓生长较快,检查时间与手术时间间隔过长可能导致癌栓升级[13,14]。其次,本例患者术前服用TKI靶向药物3个月进行减瘤,复查CT显示腔静脉癌栓未降级,但原发肿瘤大小及腔静脉癌栓范围均有所缩小。对于合并腔静脉癌栓的肾癌患者进行术前靶向药物减瘤,目前尚存争议,应全面考虑减瘤效果、药物不良反应、肿瘤进展以及对手术操作影响和患者经济负担等诸多因素[15,16]。此外,多学科合作在手术方案制定中必不可少,尤其是需要血管外科医生的参与,术前放置下腔静脉滤器、术中全程指导与协作等措施是保证手术安全的必备条件。 3.2.2 术中操作技巧
术中穿刺套管的布局以更好地显露下腔静脉为原则,并适当增加床旁助手的操作通道。术中操作以游离下腔静脉为中心,不急于处理肾蒂血管。在头侧,分离并离断肾上腺中央静脉及肝短静脉,尽量增加癌栓上方可利用腔静脉长度;在尾侧本例手术中发现伴有癌栓的生殖静脉从腔静脉表面汇入,并在两者之间有异位肾动脉穿过;游离腔静脉左侧时应注意保护左肾静脉。离断术区所有腰静脉是避免腔静脉阻断切开取栓时大量出血的关键步骤。夹闭右肾动脉,并将腔静脉、左肾静脉、右肾静脉充分游离后,以血管阻断带阻断癌栓两端腔静脉及左肾静脉,切开取栓时应注意癌栓的性状、是否侵犯腔静脉壁等,我们建议腔静脉管腔可保留40%以上时无需用人造血管补片修补。腔静脉阻断与开放应按照一定顺序进行,阻断血流:癌栓尾侧腔静脉-左肾静脉-癌栓头侧腔静脉,开放血流:左肾静脉-癌栓尾侧腔静脉-癌栓头侧腔静脉,这样有助于防止左肾静脉血流逆灌,排出腔静脉内血块或气体,并判断缝合有无漏口。有关机器人辅助全腔镜下肾切除术+腔静脉完全阻断切开取栓术操作经验的相关文献 [4,17]较少,仍需进一步积累。 3.2.3 术后处理
术后合理使用抗凝药是关键,注意出血和血栓栓塞的风险。Lee等[17]报道的病例术后11 d并发双下肢深静脉血栓形成。本例患者术后血红蛋白偏低,手术当天输血600 mL,术后第5天输血400 mL。有学者建议术后48 h后开始使用抗凝药,避免早期出血[14],也有学者建议术后使用抗凝药时需将部分凝血活酶时间(partial thromboplastin time) 控制在50~60 s[18]。
综上所述,达芬奇机器人全腔镜下肾切除术+腔静脉Ⅱ级癌栓取出术安全、可行,微创效果好,但术者需具备丰富的开放肾癌伴腔静脉癌栓手术和达芬奇机器人手术经验,且需多学科协作完成,其肿瘤学疗效仍需进一步随访观察。因此,临床应严格把握适应证,把手术安全放在第一位。 4 利益冲突
所有作者声明本文不涉及任何利益冲突。
| [1] | Edge S B,Byrd D R,Compton C C,Fritz A G,Greene F L,Trotti A.American Joint Committee on Cancer.American Cancer Society: AJCC cancer staging manual[M].7th ed.New York,NY: Springer-Verlag,2010:479-489. |
| [2] | Ljungberg B,Cowan N C,Hanbury D C,Hora M,Kuczyk M A,Merseburger A S,et al.EAU guidelines on renal cell carcinoma:the 2010 update[J].Eur Urol,2010,58:398-406. |
| [3] | Lawindy S M,Kurian T,Kim T,Mangar D,Armstrong P A,Alsina A E,et al.Important surgical considerations in the management of renal cell carcinoma (RCC) with inferior vena cava (IVC) tumour thrombus[J].BJU Int,2012,110:926-939. |
| [4] | Abaza R.Initial series of robotic radical nephrectomy with vena caval tumor thrombectomy[J].Eur Urol,2011,59:652-656. |
| [5] | Fergany A F,Gill I S,Schweizer D K,Kaouk J H,El Fettouh H A,Cherullo E E,et al.Laparoscopic radical nephrectomy with level Ⅱ vena caval thrombectomy:survival porcine study[J].J Urol,2002,168:2629-2631. |
| [6] | Romero F R,Muntener M,Bagga H S,Brito F A,Sulman A,Jarrett T W.Pure laparoscopic radical nephrectomy with level Ⅱ vena caval thrombectomy[J].Urology,2006,68:1112-1114. |
| [7] | Disanto V,Pansadoro V,Portoghese F,Scalese G A,Romano M.Retroperitoneal laparoscopic radical nephrectomy for renal cell carcinoma with infrahepatic vena caval thrombus[J].Eur Urol,2005,47:352-356. |
| [8] | Sundaram C P,Rehman J,Landman J,Oh J.Hand assisted laparoscopic radical nephrectomy for renal cell carcinoma with inferior vena caval thrombus[J].J Urol,2002,168:176-179. |
| [9] | Martin G L,Castle E P,Martin A D,Desai P J,Lallas C D,Ferrigni R G,et al.Outcomes of laparoscopic radical nephrectomy in the setting of vena caval and renal vein thrombus:seven-year experience[J].J Endourol,2008,22:1681-1685. |
| [10] | Oto A,Herts B R,Remer E M,Novick A C.Inferior vena cava tumor thrombus in renal cell carcinoma:staging by MR imaging and impact on surgical treatment[J].AJR Am J Roentgenol,1998,171:1619-1624. |
| [11] | Hallscheidt P J,Fink C,Haferkamp A,Bock M, Luburic A,Zuna I,et al.Preoperative staging of renal cell carcinoma with inferior vena cava thrombus using multidetector CT and MRI:prospective study with histopathological correlation[J].J Comput Assist Tomogr,2005,29:64-68. |
| [12] | Nazim S M,Ather M H,Hafeez K,Salam B.Accuracy of multidetector CT scans in staging of renal carcinoma[J].Int J Surg,2011,9:86-90. |
| [13] | Boorjian S A,Sengupta S,Blute M L.Renal cell carcinoma:vena caval involvement[J].BJU Int,2007,99:1239-1244. |
| [14] | Woodruff D Y,van Veldhuizen P,Muehlebach G,Johnson P,Williamson T,Holzbeierlein J M.The perioperative management of an inferior vena caval tumor thrombus in patients with renal cell carcinoma[J].Urol Oncol,2013,31:517-521. |
| [15] | Cost N G,Delacroix S E,Sleeper J P,Smith P J,Youssef R F,Chapin B F,et al.The impact of targeted molecular therapies on the level of renal cell carcinoma vena caval tumor thrombus[J].Eur Urol,2011,59:912-918. |
| [16] | Bigot P,Fardoun T,Bernhard J C,Xylinas E,Berger J,Roupret M,et al.Neoadjuvant targeted molecular therapies in patients undergoing nephrectomy and inferior vena cava thrombectomy:is it useful?[J].World J Urol,2014,32:109-114. |
| [17] | Lee J Y,Mucksavage P.Robotic radical nephrectomy with vena caval tumor thrombectomy:experience of novice robotic surgeons[J].Korean J Urol,2012,53:879-882. |
| [18] | Ayyathurai R,Garcia-Roig M,Gorin M A,González J,Manoharan M,Kava B R,et al.Bland thrombus association with tumour thrombus in renal cell carcinoma:analysis of surgical significance and role of inferior vena caval interruption[J].BJU Int,2012,110:E449-E455. |
 2014, Vol. 35
2014, Vol. 35


