*Corresponding authors.
心房颤动(atrial fibrillation,AF)是临床最常见的心律失常,普通人群中的发病率大约在1%~2%[1, 2, 3]。血栓栓塞是AF常见的最严重的并发症之一,栓子通常来源于左心房或左心耳,一旦脱落可能导致脑血管意外而致残、致命[4, 5]。 近年来导管消融术成为非瓣膜性心房颤动(NVAF)的有效治疗手段,然而左心房或左心耳血栓(left atrial thrombus,LAT)是行射频消融的绝对禁忌证。经食管超声心动描记术(transesophageal echocardiography,TEE)是目前最为常用的诊断 LAT的检查手段,但TEE作为一种半入侵性检查存在一定的风险,且部分患者存在禁忌[4]。无创性临床检查指标是否能准确评估和预测LAT值得探索。
CHADS2评分是用来对NVAF患者缺血性脑卒中进行风险分层的一种评分方法,并可指导AF患者的抗凝治疗,目前已在临床上广泛应用,因其简单易行而得到多个AF诊疗指南的推荐[6, 7, 8]。但一些临床研究也发现该方案在卒中低危、中危风险分层上存在一定的局限性[9, 10]。为了弥补CHADS2评分方案的缺陷,有学者在CHADS2的基础上提出了CHA2DS2-VASc评分方案[11],已有较多研究证实此评分方案可以较好地识别低危患者[12, 13, 14, 15]。然而,CHA2DS2-VASc评分较CHADS2评分增加了AF患者血栓预测的敏感度,同时却降低了特异性[13, 16, 17],故也增加了患者的出血风险。
本研究通过对合并LAT的NVAF患者相关临床指标进行综合分析,发现CHA2DS2-VASc评分和左心房容积指数(LAVI)是LAT的独立预测因素,进一步将LAVI和CHA2DS2-VASc评分组合成新的评分方案CHA2DS2-VASc-LA2,评估CHADS2、CHA2DS2-VASc及CHA2DS2-VASc-LA2三种评分方案对LAT的预测价值。
1 资料和方法 1.1 病例筛选从2007年6月至2012年6月我院心血管内科收治入院的720例AF患者中,入选行射频消融术治疗、术前行TEE检查的NVAF患者203例,其中男性117例、女性86例。入选标准:(1) 入院或既往心电图、24 h动态心电图提示明确AF; (2)经心脏彩超排除瓣膜性心脏病; (3)患者的相关临床资料基本完整。依据2006年美国心脏协会/美国心脏病学会(ACC/AHA)AF分型[6]分为阵发性AF和非阵发性AF(包括持续性AF和永久性AF)。排除风湿性心脏病、先天性心脏病、心肌病、血液系统和结缔组织疾病。依据TEE检查结果将左心房或左心耳有血栓形成的患者设置为血栓组,无血栓形成的设置为对照组。
1.2 病例资料收集 1.2.1 基本情况包括年龄、性别、体质指数(BMI)、AF的分类、吸烟史、入院时的血压及心率、既往病史(高血压、冠心病、糖尿病、短暂性脑缺血或脑卒中)、服药史(阿司匹林、氯吡格雷、华法林、抗心律失常药)。
1.2.2 血液生化检查项目包括血小板(PLT)、INR、总胆固醇(TC)、低密度脂蛋白(LDL)、高密度脂蛋白(HDL)。血脂水平分级依据美国国家胆固醇教育规划(NEPC)成人治疗专家组Ⅲ(ATP Ⅲ)发布的胆固醇治疗指南为参考标准。 1.2.3 CHADS2和CHA2DS2-VASc评分
包括分值及风险分层,0分为低危,1分为中危,≥2分为高危。
1.2.4 TEE检查项目及LAVITEE检查包括LAD、右心房内径(RAD)、左心室舒张末期内径(LVDD)、右心室舒张末期内径(RVDD)、 室间隔厚度(IVSD)、左心室射血分数(LVEF)、肺动脉高压(PH),其中国际推荐超声诊断PH诊断标准为≥40 mmHg[18](1 mmHg=0.133 kPa)。依据心脏多层CT扫描结果计算LAVI,公式为: LAVI=左心房容积(LAV)/体表面积(BSA); LAV=4π/3×(左心房最大横径/2)×(左心房最大前后径/2)×(左心房最大上下径/2)[19],BSA=0.006 1×身高(cm)+0.012 8×体质量(kg)-0.152 9。LAVI≥32 mL/m2为高危组,低于32 mL/m2为非高危组[20]。
1.3 统计学处理采用SPSS 17.0统计软件进行数据处理。符合正态分布的计量资料用 ±s表示,组间比较采用t检验; 非正态分布的计量资料采用中位数和四分位数[median (Q1,Q3)]表示,组间比较采用非参数检验方法。计数资料的组间比较采用χ2检验。将单因素分析中P<0.05的变量纳入二分类的logistic回归进行危险因素的筛选,检验水准(α)为0.05。依据logistic回归分析结果,将危险因素CHA2DS2-VASc和LAVI组合成新的评分方案CHA2DS2-VASc-LA2,绘制受试者工作特性曲线(ROC),比较CHADS2、CHA2DS2-VASc和CHA2DS2-VASc-LA2评分方案对血栓形成的预测价值(≥0.5且<0.7诊断价值偏低、≥0.7且<0.9诊断价值中等、≥0.9诊断价值较高)。
2 结 果 2.1 单因素分析结果 2.1.1 一般临床资料及血生化检查结果根据TEE检查结果,血栓组39例,对照组164例,两组基本情况见表 1,其中年龄、性别、BMI、吸烟史、入院时的血压及心率、冠心病、服药史(阿司匹林、氯吡格雷、华法林、抗心律失常药)差异无统计学意义(P>0.05),但血栓组中的非阵发性AF患者比例高于对照组(66.67% vs 45.12%,P=0.020)。血生化指标中除HDL在两组间差异有统计学意义(P=0.001)外,其他指标在两组间差异均无统计学意义(P>0.05,表 1)。
|
|
表 1 血栓组和对照组入选患者基本临床资料及血生化指标 Tab. 1 Clinical characteristics and biochemical results for non-thrombus and thrombus atrial fibrillation groups |
血栓组的CHADS2和CHA2DS2-VASc分值均高于对照组(P=0.007,P<0.001),中危患者比例低于对照组(P=0.004,P=0.013),高危患者比例高于对照组(P=0.001,P<0.001),而低危患者比例两组间差异无统计学意义(P>0.05)。见表 2。
|
|
表 2 血栓组和对照组入选患者的2种评分系统的分值及危险分层 Tab. 2 Results of 2 score systems and their risk stratification in non-thrombus and thrombus atrial fibrillation groups |
2.1.3 两组TEE检查及LVAI结果
血栓组和对照组患者的TEE检查结果中RAD、LVDD、RVDD、IVSD、LVEF差异无统计学意义(P>0.05); 血栓组中的LAD、PH构成比大于对照组,差异有统计学意义(P=0.001,P<0.001)。血栓组的LAVI值高于对照组,且LAVI≥32 mL/m2的比例也高于对照组,差异有统计学意义(P<0.001)。见表 3。
|
|
表 3 患者的TEE检查及LAVI结果 Tab. 3 Echocardiographic characteristics and left atrial volume indices of patients |
结合临床实际情况对模型进行择优筛选,将P<0.05的变量: LAVI≥32 mL/m2、PH≥40 mmHg、CHA2DS2-VASc≥2及NPAF以二分类变量的形式进入回归模型进行分析(另外两个单因素分析中P<0.05的变量LAD及HDL未纳入多因素分析),结果显示: LAVI≥32 mL/m2、CHA2DS2-VASc≥2分是LAT形成的独立危险因素。当CHA2DS2-VASc评分≥2分时发生血栓的风险是评分<2时的4.462倍(OR=4.462,95%CI: 1.707~11.668,P=0.002)。LAVI≥32 mL/m2时发生血栓的风险是LAVI<32 mL/m2的4.271倍(OR=4.271,95%CI: 1.915~9.582,P<0.001)。
2.3 CHA2DS2-VASc-LA2评分依据logistic回归分析结果,将LAVI≥32 mL/m2记为2分,加入CHA2DS2-VASc评分中,组成CHA2DS2-VASc-LA2评分方案。单因素分析显示,血栓组的CHA2DS2-VASc-LA2分值(4.90±2.20)比对照组(2.72±2.10)高,差异有统计学意义(P<0.01)。使用CHA2DS2-VASc-LA2评分后血栓组CHADS2评分为0分的3例低危患者分值均有上升(表 4),无CHA2DS2-VASc-LA2评分为0分者。
|
|
表 4 CHADS2评分为0分的患者其他两种评分结果 Tab. 4 The other two scores of patients with CHADS2 score being 0 |
CHADS2评分ROC曲线下面积(AUC)为0.661(P=0.002),诊断价值偏低,最佳诊断点为2分,灵敏度为0.564,特异度为0.732; CHA2DS2-VASc评分的AUC为0.731(P<0.001),诊断价值中等,最佳诊断点为2分,灵敏度为0.744,特异度为0.707; CHA2DS2-VASc-LA2评分AUC为0.771(P<0.001),诊断价值中等,最佳诊断点为3分,灵敏度为0.758,特异度为0.720。详见图 1。
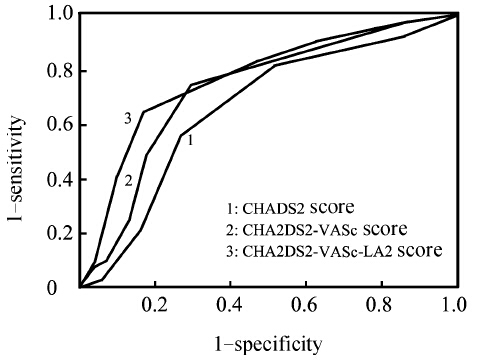
|
图 1 三种评分系统的ROC曲线结果 Fig 1 Receiver operating characteristic curve (ROC) results of three score systems The AUC for the parameters analyzed was as follows: CHADS2 score: 0.661,P=0.002; CHA2DS2-VASc score: 0.731,P<0.001; CHA2DS2-VASc-LA2 score: 0.771,P<0.001. The optimal cut-off points of CHADS2 score,CHA2DS2-VASc score,and CHA2DS2-VASc-LA2 score for predicting left atrial thrombus (LAT) were 2 points,2 points,and 3 points,respectively. The sensitivity and specificity for the parameters’ cut-off value were as follows: CHADS2 score: 0.564 and 0.732; CHA2DS2-VASc score: 0.744 and 0.707; CHA2DS2-VASc-LA2 score: 0.758 and 0.720 |
抗血小板和抗凝是临床上预防AF患者血栓形成和脑卒中风险最常用的治疗措施,两种措施各有不足,研究显示抗凝能更好地减少血栓形成及栓塞事件的发生[1],但同时增加了患者的出血风险[2],且服用普通的抗凝药物需要监测INR使得一些患者不易接受。为了使患者能得到较合理的治疗,我们需要对患者进行合理的血栓风险分层来指导治疗,但国内外研究对血栓风险分层的意见仍存在争议。CHADS2评分因其简单,可以较好地预测AF患者的中风风险,已经被临床医生及指南广泛采纳[6, 7, 8]。但本研究发现CHADS2为0分或1分的低、中危NVAF患者仍有一定的LAT发生率(7.69%,10.26%),国外研究也证实了这点[3]。这有可能使某些评分较低但实际存在LAT的患者因依据CHADS2评分进行评估而没有得到抗凝治疗,从而增加发生血栓栓塞致残、致死风险。CHA2DS2-VASc评分方案是在CHADS2的基础上提出的[11],此评分方案可以较好地识别低危患者[12, 13, 14, 15],但却降低了特异性[13, 16, 17]。
一些研究表明增大的LAD是LAT发生的独立预测因素[21, 22]。本研究通过单因素统计分析发现,血栓组的LAD水平高于对照组。Scherr等[23]通过研究AF患者电复律前结果,发现当LAD<45 mm时发生LAT的危险性较小。但左心房容积比LAD更能准确地反映左心房的实际大小,国外学者研究发现左心房容积是NVAF患者LAT发生的独立危险因素[24, 25]。即使在血栓形成危险因素较少的孤立性AF中,LAVI增大与不良心血管事件发生也紧密相关[26]。因此我们在多因素分析中纳入LAVI进行分析,结果支持上述研究。本研究通过单因素分析发现: 血栓组的HDL水平低于对照组,虽然目前缺少血脂水平和LAT的相关研究,但笔者认为,HDL与LAT存在一定相关性可能是合理的,因为LAT和静脉血栓均为红色血栓,而一些研究表明血脂水平和静脉血栓的发生关系密切[27, 28]。由于血脂水平是血管疾病的独立危险因素,可能侧面反映了血管疾病,而CHA2DS2-VASc评分中也体现了血管疾病对AF患者脑卒中的危险分层价值,因此我们未将HDL纳入多因素分析。
TEE作为AF射频消融术前排除患者左心房或左心耳是否有血栓形成的常规手段,有着很高的敏感性和特异性[19],有研究显示用TEE来诊断血栓准确率高达100%或91%[29, 30],即使是在栓塞危险因素很少的孤立性AF中也依然有很高的诊断价值[29]。但TEE为半侵入性检查且存在一定的风险,故找出一种代替TEE检查的非侵入性评估方案具有一定的临床意义。有学者提出对于CHADS2评分为0分的患者可不行TEE检查[31]。而CHA2DS2-VASc评分较CHADS2评分有着更高的敏感性[12, 13, 14, 15],那是否对于一些低危或者中低危患者可以用这两个方案来代替TEE检查呢?国外学者依据CHADS2评分、CHA2DS2-VASc评分做了一些研究,发现即使用这两种方案均评估为低危的患者用TEE检查仍有一部分检测出LAT存在[17, 32]。本研究也发现检出血栓人群中仍有7.69%的人群CHADS2评分为0分; 2.56% 的人群CHA2DS2-VASc评分为0分。依据logistic回归分析结果,将LAVI≥32 mL/m2记为2分,加入CHA2DS2-VASc评分中,组成CHA2DS2-VASc-LA2评分方案,结果发现血栓组中无CHA2DS2-VASc-LA2评分为0分者。因此,我们认为,对于CHA2DS2-VASc-LA2评分为0分者,AF患者术前可不必行TEE检查。
本研究存在一定的局限性: (1)本文是回顾性分析研究。(2)本文入选研究的样本相对较少。(3)选择人群范围较局限,均是拟行AF射频消融的患者,而这些患者往往合并心血管危险因素较少,一般临床情况较好。因此本文的结论不一定适用于所有AF人群。(4)CHA2DS2-VASc评分本身具有一定的主观性,比如对血管疾病的评分,患者没有提供血管疾病的病史不能等同于患者不存在血管疾病,因此实际评分可能偏低。(5)没有继续追踪患者的后续栓塞事件的发生情况。
4 利益冲突所有作者声明本文不涉及任何利益冲突。
| [1] | European Heart Rhythm Association; European Association for Cardio-Thoracic Surgery;Camm A J,Kirchhof P,Lip G Y,Schotten U,Savelieva I,Ernst S,et al. Guidelines for the Management of Atrial Fibrillation:The Task Force for the Management of Atrial Fibrillation of the European Society of Cardiology (ESC)[J].Eur Heart J,2010,31:2369-2429. |
| [2] | Musial J,Brzezinska-Kolarz B,Zólcinski M,Lelakowski J,Szczeklik A.Ex vivo thrombin generation in patients with venous thromboembolic disease or atrial fibrillation on long-term oral anticoagulation[J].Clin Appl Thromb Hemost,2010,16:614-621. |
| [3] | Pan M,Zhu J H,Jiang W P,Liu Z H,Li H M,Yu X H,et al.Inflammation:a possible pathogenic link to atrial fibrillation[J].Med Hypotheses,2006,67:1305-1307. |
| [4] | Stöllberger C,Chnupa P,Kronik G,Brainin M,Finsterer J,Schneider B,et al.Transesophageal echocardiography to assess embolic risk in patients with atrial fibrillation.ELAT Study Group.Embolism in Left Atrial Thrombi[J].Ann Intern Med,1998,128:630-638. |
| [5] | Sorescu D,Turk R J,Cain M,Lerakis S.Clinical and transthoracic echocardiographic predictors of abnormal transesophageal findings in patients with suspected cardiac source of embolism[J].Am J Med Sci,2003,326:31-34. |
| [6] | Fuster V,Rydón L E,Cannom D S,Crijns H J,Curtis A B,Ellenbogen K A,et al.ACC/AHA/ESC 2006 guidelines for the management of patients with atrial fibrillation:full text:a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines and the European Society of Cardiology Committee for Practice Guidelines (Writing Committee to Revise the 2001 guidelines for the management of patients with atrial fibrillation) developed in collaboration with the European Heart Rhythm Association and the Heart Rhythm Society[J].Europace,2006,8:651-745. |
| [7] | Cairns J A,Connolly S,McMurtry S,Stephenson M,Talajic M; CCS Atrial Fibrillation Guidelines Committee.Canadian Cardiovascular Society Atrial Fibrillation guidelines 2010:prevention of stroke and systemic thromboembolism in atrial fibrillation and flutter[J].Can J Cardiol,2011,27:74-90. |
| [8] | You J J,Singer D E,Howard P A,Lane D A,Eckman M H,Fang M C,et al.Antithrombotic therapy for atrial fibrillation:Antithrombotic Therapy and Prevention of Thrombosis,9th Ed:American College of Chest Physicians Evidence-Based Clinical Practice Guidelines[J].Chest,2012,141(2 Suppl):e531S-e575S. |
| [9] | Berisha B,Gashi M,Krasniqi X,Pllana E,Kocinaj D.Limitations of CHADS2 scoring system in predicting stroke risk--need to change the age criteria[J].Med Arh,2011,65:27-29. |
| [10] | Baruch L,Gage B F,Horrow J,Juul-Möller S,Labovitz A,Persson M,et al.Can patients at elevated risk of stroke treated with anticoagulants be further risk stratified?[J].Stroke,2007,38:2459-2463. |
| [11] | Lip G Y,Nieuwlaat R,Pisters R,Lane D A,Crijns H J.Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach:the euro heart survey on atrial fibrillation[J].Chest,2010,137:263-272. |
| [12] | Friberg L,Rosenqvist M,Lip G Y.Evaluation of risk stratification schemes for ischaemic stroke and bleeding in 182 678 patients with atrial fibrillation:the Swedish Atrial Fibrillation cohort study[J].Eur Heart J,2012,33:1500-1510. |
| [13] | Olesen J B,Lip G Y,Hansen M L,Hansen P R,Tolstrup J S,Lindhardsen J,et al.Validation of risk stratification schemes for predicting stroke and thromboembolism in patients with atrial fibrillation:nationwide cohort study[J].BMJ,2011,342:d124. |
| [14] | Olesen J B,Lip G Y,Lindhardsen J,Lane D A,Ahlehoff O,Hansen M L,et al.Risks of thromboembolism and bleeding with thromboprophylaxis in patients with atrial fibrillation:a net clinical benefit analysis using a‘real world’nationwide cohort study[J].Thromb Haemost,2011,106:739-749. |
| [15] | Van Staa T P,Setakis E,Di Tanna G L,Lane D A,Lip G Y.A comparison of risk stratification schemes for stroke in 79,884 atrial fibrillation patients in general practice[J].J Thromb Haemost,2011,9:39-48. |
| [16] | Parikh M G,Aziz Z,Krishnan K,Madias C,Trohman R G.Usefulness of transesophageal echocardiography to confirm clinical utility of CHA2DS2-VASc and CHADS2 scores in atrial flutter[J].Am J Cardiol,2012,109:550-555. |
| [17] | Willens H J,Gómez-Marín O,Nelson K,DeNicco A,Moscucci M.Correlation of CHADS2 and CHA2DS2-VASc scores with transesophageal echocardiography risk factors for thromboembolism in a multiethnic United States population with nonvalvular atrial fibrillation[J].J Am Soc Echocardiogr,2013,26:175-184. |
| [18] | McQuillan B M,Picard M H,Leavitt M,Weyman A E.Clinical correlates and reference intervals for pulmonary artery systolic pressure among echocardiographically normal subjects[J].Circulation,2001,104:2797-2802. |
| [19] | Tsao H M,Wu M H,Huang B H,Lee S H,Lee K T,Tai C T,et al.Morphologic remodeling of pulmonary veins and left atrium after catheter ablation of atrial fibrillation:insight from long-term follow-up of three-dimensional magnetic resonance imaging[J].J Cardiovasc Electrophysiol,2005,16:7-12. |
| [20] | Moller J E,Hillis G S,Oh J K,Seward J B,Reeder G S,Wright R S,et al.Left atrial volume:a powerful predictor of survival after acute myocardial infarction [J].Circulation,2003,107:2207-2212. |
| [21] | Calvo N,Mont L,Vidal B,Nadal M,Montserrat S,Andreu D,et al.Usefulness of transoesophageal echocardiography before circumferential pulmonary vein ablation in patients with atrial fibrillation:is it really mandatory? [J].Europace,2011,13:486-491. |
| [22] | Goswami K C,Yadav R,Rao M B,Bahl V K,Talwar K K,Manchanda S C.Clinical and echocardiographic predictors of left atrial clot and spontaneous echo contrast in patients with severe rheumatic mitral stenosis:a prospective study in 200 patients by transesophageal echocardiography[J].Int J Cardiol,2000,73:273-279. |
| [23] | Scherr D,Dalal D,Chilukuri K,Dong J,Spragg D,Henrikson C A,et al.Incidence and predictors of left atrial thrombus prior to catheter ablation of atrial fibrillation[J].J Cardiovasc Electrophysiol,2009,20:379-384. |
| [24] | Ayirala S,Kumar S,O'Sullivan D M,Silverman D I.Echocardiographic predictors of left atrial appendage thrombus formation[J].J Am Soc Echocardiogr,2011,24:499-505. |
| [25] | Doukky R,Khandelwal A,Garcia-Sayan E,Gage H.External validation of a novel transthoracic echocardiographic tool in predicting left atrial appendage thrombus formation in patients with nonvalvular atrial fibrillation[J].Eur Heart J Cardiovasc Imaging,2013,14:876-881. |
| [26] | Osranek M,Bursi F,Bailey K R,Grossardt B R,Brown R D Jr,Kopecky S L,et al.Left atrial volume predicts cardiovascular events in patients originally diagnosed with lone atrial fibrillation:three-decade follow-up [J].Eur Heart J,2005,26:2556-2561. |
| [27] | Brodde M F,Korporaal S J,Herminghaus G,Fobker M,Van Berkel T J,Tietge U J,et al.Native high-density lipoproteins inhibit platelet activation via scavenger receptor BI:role of negatively charged phospholipids[J].Atherosclerosis,2011,215:374-382. |
| [28] | Deguchi H,Pecheniuk N M,Elias D J,Averell P M,Griffin J H.High-density lipoprotein deficiency and dyslipoproteinemia associated with venous thrombosis in men[J].Circulation,2005,112:893-899. |
| [29] | Aschenberg W,Schlüter M,Kremer P,Schröder E,Siglow V,Bleifeld W.Transesophageal two-dimensional echocardiography for the detection of left atrial appendage thrombus[J].J Am Coll Cardiol,1986,7:163-166. |
| [30] | Omran H,Jung W,Rabahieh R,Wirtz P,Becher H,Illien S,et al.Imaging of thrombi and assessment of left atrial appendage function:a prospective study comparing transthoracic and transoesophageal echocardiography[J].Heart,1999,81:192-198. |
| [31] | Decker J M,Madder R D,Hickman L,Marinescu V,Marandici A,Raheem S,et al.CHADS(2) score is predictive of left atrial thrombus on precardioversion transesophageal echocardiography in atrial fibrillation[J].Am J Cardiovasc Dis,2011,1:159-165. |
| [32] | Wasmer K,Köbe J,Dechering D,Milberg P,Pott C,Vogler J,et al.CHADS(2) and CHA(2)DS (2)-VASc score of patients with atrial fibrillation or flutter and newly detected left atrial thrombus[J].Clin Res Cardiol,2013,102:139-144. |
 2014, Vol. 35
2014, Vol. 35


