2. 第二军医大学长征医院超声诊疗科, 上海 200003;
3. 金华市中心医院泌尿外科, 金华 321000;
4. 永康市人民医院泌尿外科, 金华 321300
2. Department of Ultrasound, Changzheng Hospital, Second Military Medical University, Shanghai 200003, China;
3. Department of Urology, Jinhua Central Hospital, Jinhua 321000, Zhejiang, China;
4. Department of Urology, People's Hospital of Yongkang, Jinhua 321300, Zhejiang, China
上尿路梗阻是泌尿系统的常见疾病,轻则尿液淤积,如未能及时发现、及时处置可因积液加重而引起肾功能异常。常规超声检查已经成为初步检查和评估上尿路梗阻的方法,但易受肠内气体和体型肥胖的干扰,或因病灶较小而诊断价值受限[1,2]。随着薄层扫描和螺旋扫描技术的问世,在经静脉造影辅助下的尿路增强CT成像(CT urography, CTU)提升了上尿路及膀胱微小病灶的发现能力[3,4]; 水成像技术为磁共振评价尿路梗阻提供了新方法,即磁共振尿路成像法(magnetic resonance urography, MRU),对揭示尿路梗阻的平面和程度具有较高敏感性[5,6]。CTU、MRU克服了常规超声易受肠管气体、腹壁脂肪肥厚的干扰以及病灶微小难以显示的不足,但是并未改变上尿路梗阻病例经常需要实施超声引导下经皮穿刺肾盂造瘘引流的临床现状[7 ,8,9]。
章建全等[10] 于2007年成功建立了经皮穿刺上尿路顺行造影超声检查的诊断方法,这是超声造影在血管外应用的一种新探索,对诊断上尿路的梗阻平面和梗阻程度比常规超声价值大得多,但尚未与MRU进行全面对照研究。如将经血管和血管外两种途径的超声造影结合起来,建立血管内外同步进行的双重超声造影成像新平台(dual contrast-enhanced ultrasound, DCEUS),用于上尿路梗阻的综合诊断,并尝试与CTU及MRU进行对照,将有可能提升和扩大超声影像技术在上尿路梗阻性疾病诊治中的应用能力与价值。
2008年9月至2012年5月在金华市中心医院和第二军医大学长征医院经彩色多普勒超声检查发现合并肾积水的上尿路梗阻患者147例,男72例,女75例,年龄7~87岁,平均(52.9±15.8)岁,中位年龄55岁。最终确定的梗阻病因分别为输尿管肿瘤42例、输尿管结石16例、输尿管良性狭窄44例、外源性压迫22例、先天发育异常13例、创伤性狭窄10例。依据本课题申报金华市科技局重点项目资助时获准的方案(编号2008-3-005),所有患者在外科治疗前均采取超声引导下经皮穿刺肾盂造瘘引流术,以缓解局部症状,改善肾功能。穿刺前或穿刺后3 d内完成MRU、CTU检查,2~4周内完成手术治疗并取得术后病理诊断。本研究经以上两所医院医学伦理委员会批准,所有患者均签署知情同意书。
应用Siemens Sequoia 512彩色多普勒成像仪,4V1探头(频率1.0~4.0 MHz),采用CPS-Cadence造影平台,造影频率 1.5~2.5 MHz。造影剂为六氟化硫气体冻干粉(SonoVue, Bracco, Italy),按操作说明现场制成5 mL造影剂原液备用。
常规超声检查明确肾盂和输尿管扩张的程度及范围,选择适当的体位和穿刺路径,常规消毒麻醉后,在超声引导下经皮穿刺扩张的肾盂。经穿刺针吸尽尿液,如尿液混浊疑合并感染时以灭菌生理盐水冲洗至色清。取配制好备用的造影剂原液0.5 mL,加入50 mL无菌生理盐水中。切换至CPS模式,经肾盂留置导管向肾盂内轻缓地注入造影剂溶液,连续观察肾盂、输尿管、膀胱的显影过程,并录像,重点分析梗阻的平面(梗阻所在尿路中的相对位置)和程度(完全性和不完全性)。造影结束后,吸尽尿路中的造影剂,并用生理盐水反复冲洗至造影剂回声明显减弱,需持续引流者则留置肾盂引流管。
取配制好备用的造影剂溶液2 mL经肘正中静脉团注,在CPS模式下观察尿路梗阻部位处及其邻近组织血流灌注情况,重点判断梗阻部位是否有肿瘤性因素存在(内生肿瘤或外在肿瘤压迫),对肿瘤性病灶可重复注射造影剂仔细观察其生长范围与浸润深度。
通常先行上尿路直接造影,再行经静脉超声造影,若需重点判定脏器的血供情况或肿瘤浸润范围,则先行经血管造影,再行上尿路直接造影。根据实际需要,对2种途径造影可以重复追加造影剂,直至诊断结束。
在进行肾盂穿刺造瘘术前或术后3 d内,由泌尿外科经治医师负责每例患者的MRU、CTU检查申请,并追踪、汇总检查结果。
DCEUS影像表现由2位高年资介入超声医师分析和判断,MRU、CTU影像由1位高年资影像科医师分析和判读。超声医师和影像医师在相互不知情的情况下独立诊断。最终以术中所见和(或)术后病理为金标准,计算3种影像诊断准确率,并进行统计学比较。
采用SPSS 16.0统计软件作统计分析,采用χ2检验比较3种影像方法诊断率的差异。
如表 1所示,在诊断上尿路梗阻平面时,DCEUS的准确率达100% (147/147),MRU的准确率为98.0% (144/147)。二者在输尿管上段和中段梗阻的判断上能力相同,但是在判断输尿管下段梗阻时,DCEUS优于MRU,MRU有3例漏诊。在诊断上尿路梗阻程度时,DCEUS的准确率为98.6% (145/147),明显优于MRU的89.8% (132/147)。至于梗阻程度,二者对完全梗阻的判断准确率相同; 对不完全梗阻,虽然DCEUS也有误判,但是明显优于MRU (P<0.01)。
| 表1 DCEUS与MRU诊断上尿路 梗阻平面和梗阻程度的比较 Tab 1 Comparison of DCEUS and MRU in diagnosing the level and severity of upper urinary tract obstruction |
如表 2所示,DCEUS对梗阻病因的诊断符合率总体上逊于对梗阻平面和梗阻程度的诊断。虽然DCEUS与CTU的总准确率十分接近,但是从目前数据看,在肿瘤的定性判断上DCEUS略逊于CTU。
| 表2 DCEUS与CTU诊断上尿路梗阻病因的比较 Tab 2 Comparison of DCEUS and CTU in diagnosing causes of upper urinary tract obstruction |
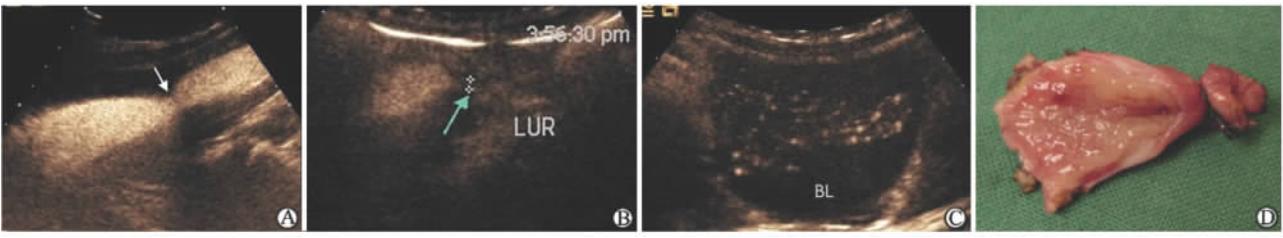
上尿路超声造影示梗阻平面以上输尿管扩张,其内充满造影剂强回声,梗阻段呈现不规则充填缺损(不完全梗阻)或造影剂强回声突然截断(完全梗阻)。经静脉超声造影示梗阻段腔内低回声团或增厚管壁回声呈不同程度增强(图 1)。
 | 图1 输尿管末端微小癌的经静脉CEUS及手术标本图 Fig 1 Intravenous CEUS of micro-carcinoma at the ureteral oriffice and surgical specimen A: The distal ureteral hypoechoic solid lesion shows no blood signal (arrow); B: Baseline sonogram before CEUS(arrow); C: CEUS sonogram, the lesion is diffusely enhanced (arrow); D: MRU, right ureter is markedly dilated, without signal on the end segment (arrow); E: Surgical specimen. CEUS: Contrast-enhanced ultrasonography; MRU: Magnetic resonance urography |
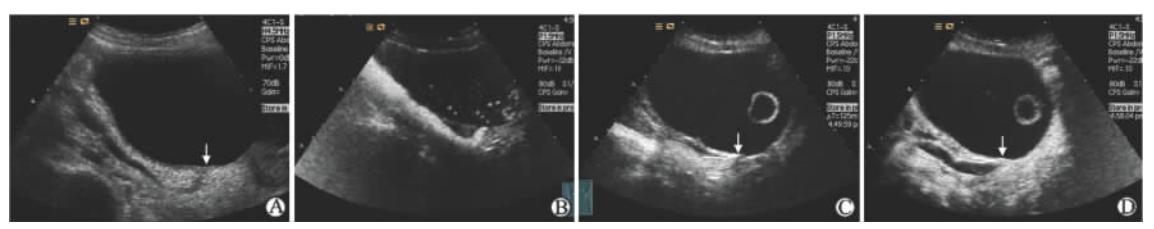
上尿路超声造影示梗阻以上输尿管扩张,梗阻段呈充填缺损或截断。经静脉超声造影示狭窄段及其周围结构未见异常增强回声(图 2)。
 | 图2 输尿管上段结石致肾积水上尿路腔CEUS Fig 2 Upper urinary tract CEUS of hydronephrosis caused by upper ureteral calculus 1: SonoVue in renal fistula; 2: SonoVue in renal collecting system and upper ureter; 3: Intraluminal filling defect on the upper ureter (calculus site); 4: SonoVue in the following ureter. CEUS: Contrast-enhanced ultrasonography |
上尿路超声造影示梗阻以上输尿管扩张,扩张程度视梗阻程度及病程长短不同而异,可表现为均匀扩张或粗细不均。经静脉超声造影示狭窄段及周围结构未见异常增强回声(图 3、图 4)。
 | 图3 输尿管中段生理性狭窄与良性病理性狭窄CEUS声像图及手术标本图Fig 3 CEUS of physiological stricture and pathological stricture of the middle ureter and surgical specimen A: Upper urinary tract CEUS shows the 2nd physiological stricture (arrow); B: Upper urinary tract CEUS shows that the ureter was seriously narrowed (arrow); C: SonoVue shows in bladder(BL)-the ureter was incompletely obstructed; D: Surgical specimen, the markedly thickened ureteral wall. Pathologic diagnosis reveales segmental submucous inflammation and fibroplasias. CEUS: Contrast-enhanced ultrasonography; LUR: Lower ureter |
 | 图4 输尿管下段良性狭窄DCEUS检查 Fig 4 DCEUS of the lower ureteral benign strictureA: Gray-scale sonogram, the ureter is dilated and the end segment becomes narrowed (arrow); B: Upper urinary tract CEUS, the ureter is dilated and the ureteral opening is narrow; C, D: Intravenous CEUS, no solid lesion at the narrow site (arrow). DCEUS: Dcul contrast-enhanced ultrasonography; CEUS: Contrast-enhanced ultrasonography |
上尿路超声造影示梗阻以上输尿管扩张,梗阻段突然变细或闭塞,管壁仍连续。经静脉超声造影示腔外实性团回声增强,输尿管壁回声未见明显增强(图 5)。
 | 图5 外在性压迫致输尿管积水DCEUS检查Fig 5 DCEUS of hydronephrosis caused by extrinsic compressionA: Upper-middle ureter is markedly dilated (open arrow), lumen near the second physiological stricture disappeares and a hypoechoic lesion is found (closed arrow); B: Intravenous CEUS, the lesion is outside the ureter and the ureter is sharply compressed (arrow); C: Upper urinary tract CEUS, the compressed segment shows weak signal of SonoVue (closed arrow), and the following ureter shows obvious signal (open arrow)-incompletely obstructed. DCEUS: Daul contrast-enhanced ultrasonography; CEUS: Contrast-enhanced ultrasonography |
表现为输尿管结构或走行异常,巨输尿管症表现为上尿路超声造影示输尿管全段极度扩张扭曲,输尿管远端近膀胱入口狭窄(图 6); 完全性重复肾之上位输尿管开口可在膀胱或者膀胱外(图 7)。
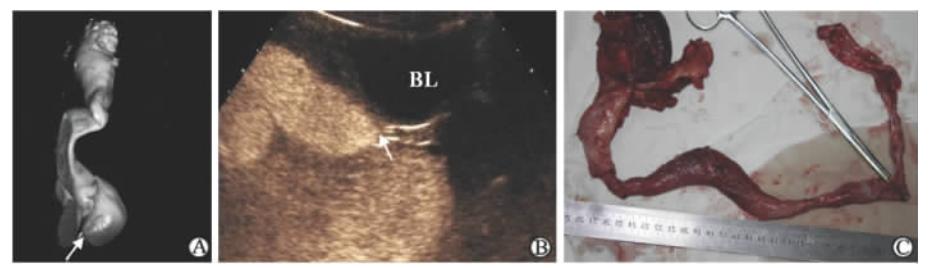 | 图6 巨输尿管症输尿管腔CEUS、MRU及手术标本图Fig 6 Upper urinary tract CEUS, MRU and sample of megaureterA: MRU 3D dimensional reconstruction, the whole ureter is extremely dilated and twisted, and the arrow is the obstructed site; B: Upper urinary tract CEUS, the whole ureter is extremely dilated and twisted, and SonoVue is never showed in bladder (BL)-the lower ureter is completely obstructed; C: Operative sample, right megaureter. CEUS: Contrast-enhanced ultrasonography; MRU: Magnetic resonance urography |
 | 图7 完全性重复肾输尿管腔CEUS Fig 7 Upper urinary tract CEUS of complete duplication of kidney A: Confirmed complete duplication of kidney, 1=mild hydronephrosis of the upper kidney, 2=mild hydronephrosis of the lower kidney; B: MRU, renal collecting system is dilated, without typical performance of complete duplication of kidney, and with weak signal of ureter; C: Ureter CEUS through the lower renal pelvis, the lumen of ureter (arrow) is large and SonoVue flow into the bladder easily; D: Ectopic opening of the upper ureter but still to bladder, the lumen of ureter is small and SonoVue flows into bladder slowly, consistent with ectopic ureteral orifice and stenosis. 1=SonoVue from upper ureter, 2=SonoVue from lower ureter, 3=Lower ureter. CEUS: Contrast-enhanced ultrasonography; MRU: Magnetic resonance urography |
发生在输尿管支架撤离后、输尿管成型术后和回肠代膀胱术后。医源性狭窄的表现符合一般良性狭窄。输尿管与回肠吻合口漏时可见造影剂从输尿管腔渗漏至吻合口外的腔隙内(图 8)。
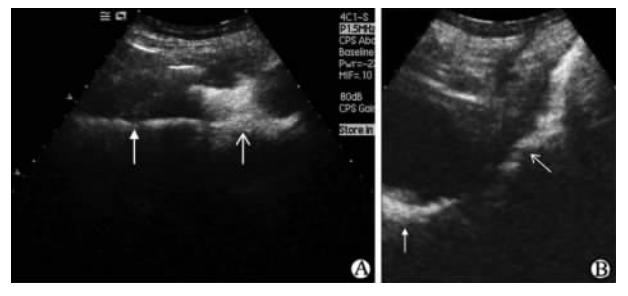 | 图8 回肠代膀胱术后输尿管回肠吻合口漏CEUS A: Ureter (closed arrow)-ileum(open arrow) anastomotic stoma is normal, SonoVue flows into ileum from ureter; B: Anastomotic leakage occurs and SonoVue leaks into the surrounding tissue space around ileum (closed arrow), which is drained by the abdominal drainage tube (open arrow) |
所有147例患者经皮肾盂穿刺均无出血、尿漏、感染播散及穿刺针道肿瘤细胞种植等并发症,在上尿路双重超声造影过程中均无局部疼痛、发热感等主诉。4例晚期肿瘤患者因死亡失访,其余患者经1~6个月的超声随访,均未见迟发并发症。
超声造影剂投予到胆道、尿路、输卵管、胃肠道等血管外管道状结构的管腔增强显像亦已显示出良好的安全性和诊断效果[10,11,12,13,14,15,16]。其中上尿路顺行造影超声检查对上尿路梗阻具有确切的诊断价值,尤其适用于上尿路梗阻需要进行肾造瘘引流的状态下。但是这种方法主要针对尿路腔的狭窄评估,对梗阻的病因诊断与鉴别,尤其是肿瘤性梗阻的评价能力尚显不足。为进一步发挥超声影像技术在上尿路梗阻诊治中的优势,提升其应用能力,我们在前期的上尿路顺行超声造影基础上,联合使用经静脉超声造影,开展上尿路梗阻平面、梗阻程度及梗阻病因的DCEUS诊断研究。
黄品同等[17] 曾采用在口服糊状胃腔造影剂辅助下经静脉注射SonoVue微泡进行胃双重超声造影检查,评估其对胃癌分期的能力。本研究所指的上尿路双重超声造影与之有本质区别,因为所用的造影剂只有一种,而且既可经血管应用又可血管外使用,造影条件一致性极好,可在2种造影途径之间迅速、灵活切换,并可根据需要随时追加造影剂的用量,延续造影过程,直至满足诊断需要。此外,即便有潜在的肾、输尿管破裂也无惧SonoVue微泡造影剂会增加不良反应。
面对众多可选用的上尿路影像学检查方法, 为何要建立和研究DCEUS技术呢?常规超声虽然操作简单,但干扰因素较多。常规CT和MRI虽然空间和密度分辨率较好,但对梗阻程度的判断有缺陷。经静脉尿路造影(IVU)和CTU均因使用X线造影剂而需要充分考虑肾功能急性损伤和对造影剂过敏的风险,当患肾功能降低或肾盂内积液较多致肾盂内静止压高于尿液的排泌压时,造影剂不能进入患侧肾盂,令IVU和CTU失去诊断价值。MRU是静态图像且尿路以外富含水分的胃肠液、膀胱尿液和腹腔积液同样被突显,可干扰甚至遮盖上尿路的显影。逆行尿路造影操作受技术和输尿管解剖因素等限制,有较高的操作失败率和并发症。经皮肾盂穿刺顺行上尿路X线造影图像清晰,诊断率高,但是除了具有X线辐射影响外,需要借助超声引导穿刺和X线成像等多种影像设备,步骤烦琐,牵涉的人力和物力较多。本研究提出的DCEUS技术可使肾盂穿刺过程及超声造影诊断一气呵成,毕上尿路顺行造影和经静脉微循环造影于一役,可对上尿路梗阻作出定位和定性诊断,减少检查环节,提高检诊效率。但是其应用前景如何,终究取决于它的综合诊断能力高低。
经肾盂引流管注射SonoVue造影剂,利用其良好的超声反射能力,动态观察造影剂在尿路中的流动走向、中断与否,以获知尿路的梗阻部位以及梗阻程度,方法简洁,能够生成对比良好的上尿路声像图,是DCEUS的核心之一,其特殊价值在于判断梗阻的平面和梗阻的程度,并显示输尿管的真实走行。本组病例所有上尿路梗阻平面均经DCEUS正确显示,其中包括受肾功能影响静脉肾盂造影不能显影的25例患者。结果表明,DCEUS和MRU在输尿管上段和中段梗阻的判断上能力相同,而在判断输尿管下段梗阻时,DCEUS优于MRU,后者存在漏诊,这可能与膀胱内尿液MR信号掩盖输尿管下段信号有关。对于完全尿路梗阻,DCEUS和MRU的判断准确率均达100%,显现出尿液完全不能跨越梗阻部位,造影剂微泡也不能通过梗阻处。而对于不完全梗阻,虽然DCEUS也有误判但是仍明显优于MRU。这种差异的原因可能是即便尿路狭窄很严重,但仍留有潜在的缝隙,MRU检查时采取的是自然静息状态,而DCEUS检查时有注射的压力存在,可使得造影剂微泡在压力驱动下透过狭窄的缝隙下行,因此出现DCEUS对不完全性梗阻的诊断符合率高于MRU。
对不完全性梗阻的高诊断率使得DCEUS备受临床重视,因为恶性肿瘤导致的输尿管严重狭窄但不完全梗阻病例,可借助放置输尿管内金属支架解决尿液的正常引流问题[18],对良性输尿管狭窄暂不宜手术干预的患者也具有重要的治疗效果[19,20]。支架能否成功置入取决于导丝能否通过狭窄段,运用DCEUS技术可预先获得输尿管成角、肿瘤堵塞或压迫、管腔严重纤维化所导致的输尿管是否已完全梗阻等重要信息,为订制支架规格,制定放置支架的方案提供客观依据,以减少失败率[21] 。
我们发现对于上尿路梗阻的病因诊断,DCEUS与CTU的总准确率高度接近。通过显示梗阻部位以及周围结构的微循环灌注,经静脉CEUS提高了超声对微小隐匿肿瘤的检出[22],本组5例输尿管肿瘤表现为管壁增厚型,常规超声不能鉴别良恶性,CEUS显示增厚的管壁呈不均匀增强,有恶性倾向,得到术后病理的证实。CEUS的另一优点是可增强显示肿瘤的真实境界以及浸润的广度和深度。但是从病因构成看,在肿瘤和良性狭窄的判断上DCEUS尚有不足。此外,对部分上尿路梗阻不严重,临床不需要行肾盂穿刺引流进行治疗的病例,经皮穿刺上尿路顺行超声造影即为一种有创的检查方法,需要慎行。
DCEUS的潜在并发症来自于经皮肾盂穿刺过程和造影剂两方面。穿刺可能并发肾脏出血和尿漏,因此穿刺时使用彩色多普勒超声引导,以避开肾脏血管,更要避免损伤输尿管。穿刺前对所有患者均行凝血功能检查,遇凝血酶原时间明显延长者则暂缓实施穿刺造瘘术,尤需注意患者是否有拜阿司匹林、华法林、氯吡格雷、红景天、丹参等活血化瘀药物的服用史,这类药物导致的凝血功能障碍在目前常用的凝血检查项目中难以反映出来。遇肾盂大量积液,压力过高或合并感染时,先吸尽尿液并以生理盐水充分冲洗,然后再放置引流导管,如此可避免感染播散。SonoVue的血管途径应用是安全的,在尿路途径应用时只需重点关注局部刺激症状,结果表明无论是在DCEUS过程中还是结束后,均未发现明显的不良反应。
上尿路双重超声造影是一种安全、高效的超声造影检查过程,对上尿路梗阻性疾病可作出精确的定位和准确的定性诊断,尤其对于严重梗阻患者,因与经皮穿刺肾盂造瘘术结合在一起,具有微创诊治兼备的优势。
所有作者声明本文不涉及任何利益冲突。
| [1] | Dana A, Hélénon O.[Urinary tract imaging:conventional radiology and ultrasound][J].J Radiol, 2004, 85(2 Pt 2):169-170. |
| [2] | Meola M, Petrucci I, Giovannini L, Colombini E, Villa A.[Ultrasound and color Doppler imaging for kidney and urinary tract tumors][J].G Ital Nefrol, 2012, 29:452-466. |
| [3] | Razavi S A, Sadigh G, Kelly A M, Cronin P.Comparative effectiveness of imaging modalities for the diagnosis of upper and lower urinary tract malignancy:a critically appraised topic[J].Acad Radiol, 2012, 19:1134-1140. |
| [4] | Chlapoutakis K, Theocharopoulos N, Yarmenitis S, Damilakis J.Performance of computed tomographic urography in diagnosis of upper urinary tract urothelial carcinoma, in patients presenting with hematuria:systematic review and meta-analysis[J].Eur J Radiol, 2010, 73:334-338. |
| [5] | Semins M J, Feng Z, Trock B, Bohlman M, Hosek W, Matlaga B R.Evaluation of acute renal colic:a comparison of non-contrast CT versus 3-T non-contrast HASTE MR urography[J].Urolithiasis, 2013, 41:43-46. |
| [6] | Lee K S, Zeikus E, DeWolf W C, Rofsky N M, Pedrosa I.MR urography versus retrograde pyelography/ureteroscopy for the exclusion of upper urinary tract malignancy[J].Clin Radiol, 2010, 65:185-192. |
| [7] | Baishya R K, Dhawan D R, Jagtap J, Sabnis R, Desai M R.Percutaneous nephrostomy under ultrasound guidance[J].Indian J Nephrol, 2011, 21:67. |
| [8] | Penbegul N, Hatipoglu N K, Bodakci M N, Atar M, Bozkurt Y, Sancaktutar A A, et al.Role of ultrasonography in percutaneous renal access in patients with renal anatomic abnormalities[J].Urology, 2013, 81:938-942. |
| [9] | PenbegÜl N, Tepeler A, Sancaktutar A A, Bozkurt Y, Atar M, Yildirim K, et al.Safety and efficacy of ultrasound-guided percutaneous nephrolithotomy for treatment of urinary stone disease in children[J].Urology, 2012, 79:1015-1019. |
| [10] | 章建全, 孟 进, 季秀凤, 陈佳彬, 肖 燕.经皮穿刺上尿路顺行造影超声检查及其临床意义[J].中国超声医学杂志, 2007, 23:469-472. |
| [11] | Valentini A L, De Gaetano A M, Minordi L M, Nanni G, Citterio F, Viggiano A M, et al.Contrast-enhanced voiding US for grading of reflux in adult patients prior to antireflux ureteral implantation[J].Radiology, 2004, 233:35-39. |
| [12] | Claudon M, Cosgrove D, Albrecht T, Bolondi L, Bosio M, Calliada F, et al.Guidelines and good clinical practice recommendations for contrast enhanced ultrasound (CEUS)-update 2008[J].Ultraschall in Med, 2008, 29:28-44. |
| [13] | 章建全, 陈佳彬, 刘 灿, 蔡清萍, 陈学云.经皮经肝穿刺胆道超声造影的方法及临床意义[J].中华超声影像学杂志, 2008, 24:513-516. |
| [14] | 张艳玲, 许尔蛟, 郑荣琴, 任 杰, 苏中振.经皮二维胆道超声造影的临床应用[J].中国医学影像技术, 2011, 27:1205-1208. |
| [15] | 章建全, 黄海鸣, 杨玉华.口服SonoVue胃腔超声造影诊断价值的初步评价[J].第二军医大学学报, 2007, 28:863-866. Zhang J Q, Huang H M, Yang Y H.Diagnostic value of oral SonoVue in contrast-enhanced ultrasound examination of stomach:a preliminary study[J].Acad J Sec Mil Med Univ, 2007, 28:863-866. |
| [16] | 宋家琳, 章建全, 赵皓珺, 盛建国, 卢 峰.非血管超声造影指导下穿刺引流上消化道瘘的初步尝试[J].第二军医大学学报, 2010, 31:753-755. Song J L, Zhang J Q, Zhao H J, Sheng J G, Lu F.Values of non-vascular contrast-enhanced ultrasound in guiding percutaneous drainage of upper gastrointestinal fistulas[J].Acad J Sec Mil Med Univ, 2010, 31:753-755. |
| [17] | 黄品同, 李艳萍, 赵雅萍, 黄福光, 杨勇明, 郑志强, 等.超声双重造影对胃癌术前T分期的价值[J].中华超声影像学杂志, 2008, 17:33-36. |
| [18] | Blaschko S D, Deane L A, Krebs A, Abdelshehid C S, Khan F, Borin J, et al.In-vivo evaluation of flow characteristics of novel metal ureteral stent[J].J Endourol, 2007, 21:780-783. |
| [19] | Benson A D, Taylor E R, Schwartz B F.Metal ureteral stent for benign and malignant ureteral obstruction[J].J Urol, 2011, 185:2217-2222. |
| [20] | López-Huertas H L, Polcari A J, Acosta-Miranda A, Turk T M.Metallic ureteral stents:a cost-effective method of managing benign upper tract obstruction[J].J Endourol, 2010, 24:483-485. |
| [21] | Barbalias G A, Liatsikos E N, Kalogeropoulou C, Karnabatidis D, Siablis D.Metallic stents in gynecologic cancer:an approach to treat extrinsic ureteral obstruction[J].Eur Urol, 2000, 38:35-40. |
| [22] | Drudi F M, Di Candio G, Di Leo N, Malpassini F, Gnecchi M, Cantisani V, et al.Contrast-enhanced ultrasonography in the diagnosis of upper urinary tract urothelial cell carcinoma:a preliminary study[J].Ultraschall Med, 2013, 34:30-37. |
 2014, Vol. 35
2014, Vol. 35


