2. 福建医科大学附属第一医院神经外科, 福州 350005;
3. 烟台警备区门诊部, 烟台 264000
2. Department of Neurosurgery, The First Affiliated Hospital of Fujian Medical University, Fuzhou 350005, Fujian, China;
3. Hospital of Yantai Military Garrison, Yantai 264000, Shandong, China
烟雾病是以双侧颈内动脉末端慢性进行性狭窄或闭塞为特征,并继发引起颅底异常血管网形成的一种少见的脑血管疾病。这种颅底异常血管网在脑血管造影图像上形似“烟雾”,被称之为“烟雾状血管”。因此,1969年日本学者Suzuki及Takaku将该病称之为“烟雾病”[1]。烟雾病的治疗方法有保守治疗(随访观察、药物治疗)及手术治疗。手术治疗的术式多种多样,可分为介入手术与开颅手术。根据目前可获得的文献资料来看,介入手术治疗烟雾病效果不理想[2,3,4]。目前最常用的开颅手术术式为直接脑血管重建手术(即颅内-外血管直接搭桥术)及间接脑血管重建手术(包括脑-硬膜-血管融合术、脑-颞肌贴敷术、脑-肌肉-血管融合术及大网膜移植术等)[5,6,7]。烟雾病患者临床表现多变,手术方式多样,每个患者的文化背景、心理素质等也不尽相同。个体化治疗对烟雾病患者来讲至关重要。因此,本研究回顾性分析2010~2013年烟雾病患者临床资料,对不同临床分型、影像学分期烟雾病患者的治疗方法及策略进行总结,为规范烟雾病的临床诊治提供参考。 1 资料和方法 1.1 一般资料
2010年4月~2013年12月苏州大学附属常熟市第一人民医院及福建医科大学附属第一医院收治的烟雾病患者39例,全部患者均通过脑CT血管成像(CTA)或数字减影血管造影(DSA)确诊为烟雾病。男15例,女24例,平均(30.4±2.1)岁(11~56岁)。根据1990年Matsushima等提出的分型标准[7],临床分型如下:以短暂性脑缺血发作(TIA)起病9例(Ⅰ型:TIA型;Ⅱ型:频发TIA型);以脑梗死起病合并短暂性脑缺血发作或短暂性脑缺血发作起病合并脑梗死共20例(Ⅲ型:TIA-脑梗死型;Ⅳ型:脑梗死-TIA型);以脑梗死起病5例(Ⅴ型:脑梗死型);脑出血型患者共5例(Ⅵ型:脑出血型)。其中首发或合并癫疒 间 患者8例。
根据1969年Suzuki和Takaku提出的烟雾病血管造影的分期标准[1],影像学分期如下,Ⅰ期:颈内动脉末端狭窄(n=0);Ⅱ期:产生烟雾状血管,远端动脉扩张(n=5);Ⅲ期:烟雾状血管增多(n=13);Ⅳ期:烟雾状血管减少,远端动脉不显影(n=11);Ⅴ期:烟雾状血管极少,主要动脉分支消失(n=8);Ⅵ期:烟雾状血管消失,大脑主要靠颈外动脉供血(n=2)。 1.2 手术治疗
脑实质内出血急诊入院的患者,术前经头颅CT证实脑内出血,CTA提示为烟雾病,急诊手术行颅内血肿清除+去骨瓣减压术,同时将硬膜翻转贴敷、颞肌贴敷(脑-硬膜-肌肉血管融合术)。择期手术的患者,予术前评估包括头颅CT、MRI、DSA以及头颅CT灌注(CTP)。根据上述影像学评估、血流动力学评估资料制定手术方案。围手术期管理:适当的静脉补液,结合术中控制血压维持于正常或稍高水平,使用神经保护剂,维持氧饱和度;围手术期预防癫疒 间 治疗,控制血糖,控制血压于基础值或稍高水平。 1.3 术后随访
术后1周内复查CTA或DSA,再次验证吻合血管的通畅性。术后1周内复查CTP,检测脑血流动力学变化情况。体格检查:检测患者的智力和语言表达情况,运动和感觉情况。电话随访是否有缺血或出血发作。半年内复查DSA,了解侧支循环形成情况,复查CTP。 1.4 统计学处理 采用SPSS19.0软件,计量数据以 ±s 表示,独立样本t检验,检验水准(α)为0.05。 2 结 果 2.1 治疗情况
39例患者中5例为脑实质内出血急诊入院,急诊行颅内血肿清除+去骨瓣减压+脑-硬膜-肌肉血管融合术。其余34例为择期手术患者,包括:6例患者因受体或供体血管较纤细,无法进行颞浅动脉-大脑中动脉(STA-MCA)吻合,选择脑-硬膜-肌肉血管融合术;28例患者接受综合手术治疗(STA-MCA吻合+脑-硬膜-肌肉血管融合术),4例患者首次手术半年后行对侧综合手术治疗。本组患者平均随访时间(21.3±3.1)个月(7~44个月)。 2.2 临床疗效
原有TIA发作者29例,其中21例术后未再发生手术侧的TIA发作,原有神经功能障碍从术后第2天即有改善;8例在术后短期内仍有与手术侧半球相关的TIA发作,随访发现其发作间期不断延长(6例在10 d后,2例在1个月后不再发作)。术前有神经功能障碍的患者25例,术后均有不同程度的恢复。出血型患者5例,随访至今,未再有出血。其中有2例合并手术侧脑内小动脉瘤者,术中未处理动脉瘤,术后6个月随访发现动脉瘤消失。本组无术后新发脑梗病例;首发或合并癫疒 间 的8例患者,经围手术期抗癫疒 间 治疗,术后无再发癫疒 间 ;但1例术前无癫疒 间 的患者,术后第2天出现癫疒 间 发作,加大抗癫疒 间 药物剂量后未有再次发作。 2.3 影像及血流动力学复查结果
接受综合手术治疗的28例患者中,27例患者术后1周内复查了CTA,1例复查DSA,显示吻合血管全部通畅(图 1)。均于术后1周内复查CTP,以对侧为参照,分析脑血流量(CBF)、脑血容量(CBV)、平均达峰时间(TTP)数据,结果表明:脑-硬膜-肌肉血管融合术11例,术后1周脑血流灌注情况与术前相比差异无统计学意义;综合手术治疗组28例,手术侧半球血流灌注情况较术前明显改善(表 1);其中有1例单侧手术患者,术后双侧半球血供均有明显改善(图 2)。
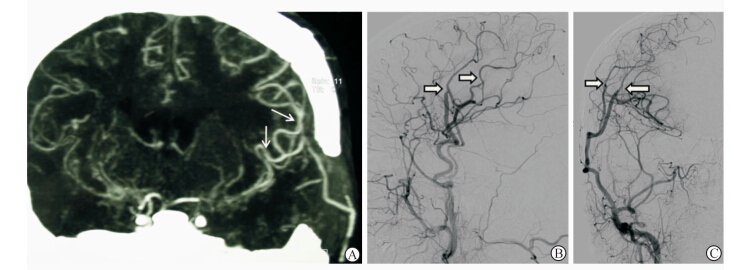 | 图 1 术后1周头颅CTA或DSA复查 Fig 1 CTA/DSA images at one week post-operation A: CTA one week post-operation demonstrated that the two STA-MCA anastomoses were in good patency (white arrow); B-C: DSA images of ECA (posteroanterior view and lateral view) demonstrated that the two STA-MCA anastomoses were in good patency (white hollow arrow) |
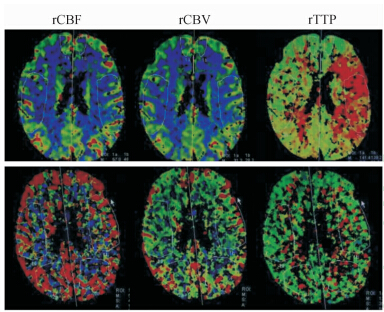 | 图 2 术后1周头颅CTP复查 Fig 2 CTP image at 1 week post-operation CTP imaging showed a significant increase of the rCBF and rCBV,but a decrease of rTTP after the operation (upper row: pre-operation; lower row: 1 week post-operation) |
|
|
表 1 间接脑血管重建组、综合手术治疗组患者术前及术后1周CTP检查结果 Tab 1 CTP data pre- and one week post-operationin patients treated by indirect bypass surgery or combined (indirect + direct) bypass surgery |
本组39例患者中有32例患者半年后复查头颅CTP及头颅CTA/DSA(另外7例患者术后临床状况恢复良好,拒绝进一步检查)。术后6个月CTP结果:脑-硬膜-肌肉血管融合术治疗组脑血流灌注情况较术前改善,差异有统计学意义(P<0.05);综合手术治疗组术侧脑血流灌注情况较术后1周时进一步改善(P<0.05,表 2)。 头颅CTA/DSA显示吻合口均通畅,其中19例颞浅动脉较手术前增粗;间接手术形成的脑膜中(副)动脉、颞中深动脉、蝶腭动脉均与皮质动脉形成不同程度的吻合,并相应地较术前明显增粗(表 3)。
|
|
表 2 间接脑血管重建组、综合手术治疗组患者术前及术后6个月时CTP检查结果 Tab 2 CTP data pre- and six months post-operation in patients treated by indirect bypass surgery or combined bypass surgery |
|
|
表 3 术后6个月时综合手术治疗组血管直径的变化 Tab 3 Vessel diameter changes at pre- and 6 months post-operation in patients treated by combined bypass surgery (n=27) |
烟雾病的治疗方法主要包括一般治疗、药物治疗、手术治疗,目前尚无Ⅰ级、Ⅱ级的循证医学证据指明选择药物治疗或手术治疗具体指征[8,9]。具体治疗措施包括,(1)一般治疗:以密切观察病情变化为主,同时应避免可能加重病情的危险因素,如应忌辛辣、高脂饮食,儿童患者注意避免其严重的哭闹[10,11];(2)药物治疗:包括合并症的治疗、对症治疗以及针对危险因素的治疗,如血管扩张剂、抗凝药、溶纤维蛋白药、抗溶纤维蛋白药、抗癫疒 间 药等;(3)手术治疗:包括间接、直接脑血管重建及综合手术(间接+直接)。
结合既往文献及本组患者临床实践经验,我们总结了不同临床分型烟雾病的如下治疗策略。(1)临床分型Ⅰ型的患者TIA或RIND发作每个月≤2次,无神经功能障碍,头颅CT/MRI无阳性发现,影像学分期常对应为Ⅰ或Ⅱ期。若CTP检查提示Ⅰ型患者的脑血流灌注情况无明显异常,可选择上述非手术治疗方法;若CTP检查提示存在脑血流灌注受损,建议选择手术治疗。(2)Ⅱ~Ⅴ型患者均存在不同程度的脑灌注不足或灌注储备功能受损[12,13]。对于这部分患者,术前应根据患者的临床表现、影像学及脑血流动力学评估结果制定手术策略,具体手术方式参照文献[14]。本组手术指征如下:脑缺血相关的神经功能障碍;反复缺血发作或进展性神经功能发育迟缓;额叶和(或)枕叶CBF下降,或CT提示额叶和(或)枕叶脑萎缩;一过性肢体乏力或低血压;持续性病情进展;CVR下降;首次手术后仍有反复的TIA或卒中发作。(3)Ⅵ型:为出血型或无法归纳于Ⅰ~Ⅴ型的患者,脑出血急性期应根据患者临床状况、血肿量及部位选择保守治疗、脑血肿清除术、脑室外引流术或去骨瓣减压术。脑出血恢复后的颅内外血管重建手术随访可预防再出血,因目前尚无设计完善的大规模临床RCT试验而存在争议,文献报道结果不一[15,16]。我们的经验是术前评估发现存在下列潜在脑出血风险的患者建议手术治疗:存在颅内动脉瘤、微小动脉瘤;MRI-T2可见微小出血灶;脉络膜前动脉或后交通动脉处出现异常分支且分支扩张;以脑出血为首发临床症状,但有脑缺血证据或CBF、CVR下降证据者。本组5例Ⅵ型患者随访至今,未再有出血。其中有2例合并手术侧脑内小动脉瘤者,术中未处理动脉瘤,术后6个月随访发现动脉瘤消失。Ni等[17]2012年也报道了类似现象的病例。而且CTP提示Ⅵ型患者术后脑血流灌注情况改善,术后发生缺血性卒中风险降低。
影像学分期与治疗策略:Ⅰ期为影像学仅出现颈内动脉末端狭窄,这部分患者常无明显临床症状,临床不易发现。因此,Ⅰ期患者建议随访,必要时予药物治疗(降血脂、控制血压、血糖等)。Ⅱ期以上患者常有临床症状而就诊,应根据患者的临床表现、影像学及脑血流动力学评估结果制定手术策略。对于Ⅱ期以上患者我们的治疗策略是:(1)通常情况下行STA-MCA吻合,根据术前评估结果必要时可行STA-MCA+STA-ACA或PCA吻合;对于STA-ACA或PCA吻合困难的病例,可采用大骨瓣开颅或在额部、枕部多处钻孔行间接吻合的方法代替STA-ACA或PCA吻合。(2)首选直接+间接脑血管重建的综合术式,只有供体/受体血管条件差,直接血管吻合困难时,才考虑间接血管吻合。(3)缺血型患者血管条件允许时行双搭桥;供体/受体血管不佳以及出血型患者单搭桥。(4)Ⅴ期及Ⅵ期的患者,影像学上可见颅内外自发吻合血管(如MMA分支、STA分支向颅内形成自发吻合)应予保护完好。根据颅内外自发吻合血管范围,个体化设计皮瓣、骨窗及硬膜的翻转贴敷(图 3、图 4)。
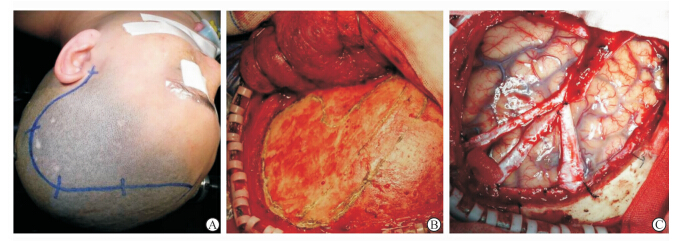 | 图 3 影像学Ⅲ期患者个体化手术方案设计 Fig 3 Individually designed surgical procedures for a radiographic stage Ⅲ moyamoya disease patient A: Position and incision,a modified pterional approach was adopted; B: The bone window was designed individually to ensure the integrity of the MMA; C: The MMA trunk and its main branches were preserved intact and incised on both sides,resulting in dura mater strips with a width of 0.5-1.0 cm. Then radial incisions were made on the remaining part of the dura mater. After the hemostasis,the dura mater was flipped over and spread over the bone window |
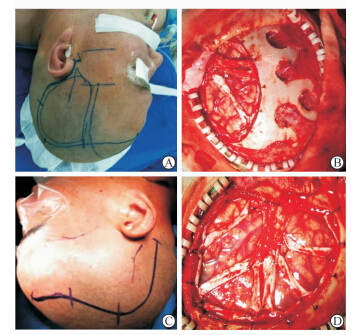 | 图 4 影像学Ⅴ、Ⅵ期患者个体化手术方案设计 Fig 4 Individually designed surgical procedures for a radiographic stage Ⅴ & Ⅵ moyamoya disease patient A-B: a radiographic stage Ⅴ patient; C-D: another radiographic stage Ⅴ patient. After pre-operative analysis of DSA image,we designed the skin incision,bone window and dura incision individually,so as to protect anastomoses formed pre-operatively |
综上所述,烟雾病临床表现多变,手术方式多样,必须根据患者不同的临床分型、影像学分期,采取不同的治疗方案,才能使患者最终获益。
4 利益冲突
所有作者声明本文不涉及任何利益冲突。
| [1] | Suzuki J,Takaku A.Cerebrovascular “moyamoya” disease:Disease showing abnormal netlike vessels in base of brain [J].Arch Neurol,1969,20:288-299. |
| [2] | Drazin D,Calayag M,Gifford E,Dalfino J,Yamamoto J, Boulos A S.Endovascular treatment for moyamoya disease in a Caucasian twin with angioplasty and Wingspan stent [J].Clin Neurol Neurosurg,2009,111:913-917. |
| [3] | El-Hakam L M,Volpi J,Mawad M,Clark G. Angioplasty for acute stroke with pediatric moyamoya syndrome [J].J Child Neurol,2010,25:1278-1283. |
| [4] | Khan N,Dodd R,Marks M P,Bell-Stephens T,Vavao J,Steinberg G K.Failure of primary percutaneous angioplasty and stenting in the prevention of ischemia in Moyamoya angiopathy [J].Cerebrovasc Dis,2011,31:147-153. |
| [5] | Research Committee on the Pathology and Treatment of Spontaneous Occlusion of the Circle of Willis; Health Labour Sciences Research Grant for Research on Measures for Infractable Diseases.Guidelines for diagnosis and treatment of moyamoya disease (spontaneous occlusion of the circle of Willis)[J].Neurol Med Chir (Tokyo),2012,52:245-266. |
| [6] | Kuroda S,Houkin K.Bypass surgery for moyamoya disease:concept and essence of sugical techniques[J].Neurol Med Chir (Tokyo),2012,52:287-294. |
| [7] | Matsushima T,Fukui M,Kitamura K,Hasuo K,Kuwabara Y,Kurokawa T.Encephalo-duro-arterio-synangiosis in children with moyamoya disease[J].Acta Neurochir (Wien),1990,104:96-102. |
| [8] | Jin S C,Oh C W,Kwon O K,Hwang G,Bang J S,Kang H S,et al.Epilepsy after bypass surgery in adult moyamoya disease [J].Neurosurgery,2011,68:1227-1232. |
| [9] | Fung L W,Thompson D,Ganesan V.Revascularisation surgery for paediatric moyamoya:a review of the literature [J].Child Nerv Syst,2005,21:358-364. |
| [10] | Smith E R,Scott R M.Spontaneous occlusion of the circle of Willis in children:pediatric moyamoya summary with proposed evidence-based practice guidelines.A review[J].J Neurosurg Pediatr,2012,9:353-360. |
| [11] | Fujimura M,Tominaga T.Lessons learned from moyamoya disease:outcome of direct/indirect revascularization surgery for 150 affected hemispheres [J].Neurol Med Chir (Tokyo),2012,52:327-332. |
| [12] | Guzman R,Lee M,Achrol A,Bell-Stephens T,Kelly M,Do H M,et al.Clinical outcome after 450 revascularization procedures for moyamoya disease.Clinical article[J].J Neurosurg,2009,111:927-935. |
| [13] | Narisawa A,Fujimura M,Tominaga T.Efficacy of the revascularization surgery for adult -onset moyamoya disease with the progression of cerebrovascular lesions [J].Clin Neurol Neurosurg,2009,111:123-126. |
| [14] | Xu B,Song D L,Mao Y,Gu Y X,Xu H,Liao Y J,et al.Superficial temporal artery-middle cerebral artery bypass combined with encephalo-duro-myo-synangiosis in treating moyamoya disease:surgical techniques,indications and midterm follow-up results[J].Chin Med J (Engl),2012,125:4398-4405. |
| [15] | Derdeyn C P.Direct bypass reduces the risk of recurrent hemorrhage in moyamoya syndrome,but effect on functional outcome is less certain [J].Stroke,2014,45:1245-1246. |
| [16] | Miyamoto S,Yoshimoto T,Hashimoto N,Okada Y, Tsuji I,Tominaga T,et al.Effects of extracranial-intracranial bypass for patients with hemorrhagic moyamoya disease:results of the Japan Adult Moyamoya Trial[J].Stroke,2014,45:1415-1421. |
| [17] | Ni W,Xu F,Xu B,Liao Y,Gu Y,Song D.Disappearance of aneurysms associated with moyamoya disease after STA-MCA anastomosis with encephaloduro myosynangiosis[J].J Clin Neurosci.2012,19:485-487.. |
 2014, Vol. 35
2014, Vol. 35


