文章信息
- 腹膜后肌周细胞瘤1例并文献复习
- Retroperitoneal Myopericytoma: A Case Report and Literature Review
- 肿瘤防治研究, 2018, 45(7): 510-511
- Cancer Research on Prevention and Treatment, 2018, 45(7): 510-511
- http://www.zlfzyj.com/CN/10.3971/j.issn.1000-8578.2018.18.0387
- 收稿日期: 2018-03-22
- 修回日期: 2018-04-15
2. 430079 武汉,湖北省肿瘤医院病理科
2. Department of Pathology, Hubei Cancer Hospital, Wuhan 430079, China
肌周细胞瘤是临床极少见血管周细胞源性肿瘤,多为良性,主要发生于肢体远端皮下软组织,发生于腹腔深部者罕见。且本例为腹膜后交界性潜在低度恶性肌周细胞瘤,现报道如下。
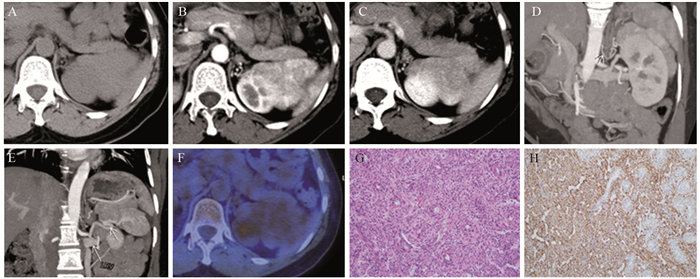
1 临床资料患者女,55岁,体检发现左上腹占位1月余,外院增强MR左上腹占位不排除副脾,患者行PET-CT检查提示左上腹肿块代谢稍高。患者自患病以来,神志清楚,精神尚可,食欲、睡眠一般,大小便正常,体力体重无明显改变。肿瘤标志物、血常规、生化检查阴性。CT表现:左上腹腹膜后脾旁大小约6.7 cm×4.5 cm软组织密度肿块,与脾脏及左肾上极分界欠清,平扫CT值约47 Hu,增强扫描动脉期明显不均匀强化,CT值约120 Hu,门脉期强化退出CT值约110 Hu,低于同层面脾脏密度,最大密度投影(maximum intensity projection, MIP)示肿瘤供血动脉来源于腹主动脉,MIP显示肿瘤引流血管汇入左肾静脉,见图 1A~E。PET/CT示病灶摄取,最大SUV约3.2,延迟显像最大SUV为3.6,见图 1F。术中所见:肿瘤位于腹膜后,靠近胰尾,上极与脾下极静脉相邻,下极与左肾上极粘连,周围无明显肿大淋巴结。行左上腹腹膜后肿物切除术。病理:切面灰白,卵圆形肌样细胞围绕血管同心圆状排列,核分裂可见,鉴于肿瘤位于深部、肿块较大,边界不清,应视为交界性潜在低度恶性肿瘤;免疫组织化学结果:SMA(弱+),H-caldesmon(+),Desmin(+),Bcl-2(+),CD117(-),DOG-1(-),CD34(-),S-100(-),HMB45(散+),Melan-a(-),TFE3(弱+),PCK(-),CD10(-),Ki-67(li: 2%),见图 1G~H。病理诊断:肌周细胞瘤。
|
| A: unenhanced computed tomography (CT) showed a soft tissue mass with irregular margin in the upper left retroperitoneum beside the spleen; B: arterial phase, the mass showed heterogeneous enhancement, similar to the spleen; C: portal phase, the mass showed weakening enhancement and the density was lower than the spleen(arrow); D: MIP showed that the mass had blood supplied by the abdominal artery(arrow); E: MIP showed the draining vein of the mass converged to the left renal vein; F: PET/CT showed the mass had slightly 18F-FDG uptake; G: Histopathological examination showed spindle-shaped myopericytic cells with characteristic concentric distribution(HE ×100); H: Immunohistochemistry(IHC) showed desmin staining was positive (×100) 图 1 腹膜后肌周细胞瘤患者CT、PET/CT、镜下及免疫组织化学图 Figure 1 Computed tomography, PET/CT, microscopic and IHC staining results of the retroperitoneal myopericytoma patient |
肌周细胞瘤(myopericytoma)是一种具有向血管周围肌样细胞或肌周细胞分化的软组织肿瘤,与血管球瘤、肌纤维瘤(病)、血管平滑肌瘤与肌周细胞瘤同属于血管周细胞肿瘤瘤谱。组织病理学特点:具有明显向血管周肌样细胞和肌周细胞分化趋势的卵圆形或梭形细胞围绕血管呈同心圆状排列,因此,2013年WHO软组织肿瘤分类将其归类于血管周细胞肿瘤而非血管肿瘤。免疫组织化学特点:SAM和H-caldesmon阳性,球细胞一般弥漫性表达,也可在血管灶性表达,Desmin局灶阳性,CD34局灶阳性,S-100蛋白阴性,角蛋白大部分阴性。
本病好发于成人,发生于小孩者少见[1]。好发部位以肢体远端皮下软组织多见,亦见发生于其他部位的报道[2-9],如阴茎、脊柱、心房、输尿管、颅内、肝门区、血管内、内听道、膀胱、舌根等身体各部位。病变常单发,多发少见。该肿瘤通常为良性,也有恶性的报道[10],手术应完整切除。本例患者无明显临床症状,术中所见肿块与左肾粘连,病理示肿瘤为交界性肿瘤有恶性潜能,术后6月复查未见肿瘤复发转移。
目前,关于肌周细胞瘤的研究多为个案报道,缺少大样本回顾性分析。结合文献报道,总结肌周细胞瘤的影像学表现特点如下:单发,多发罕见;病灶边缘大多清晰;血供丰富强化明显,密度均匀或不均匀;与周围组织表现为粘连,少见侵犯与转移。本例肿瘤表现为软组织肿块与左肾上极粘连,供血动脉源于腹主动脉,增强扫描动脉期强化明显,类似于脾脏强化,延迟期强化退出。文献所述临床表现如下:无临床症状、局部肿块伴或不伴疼痛、肿块占位效应继发相应症状。该病例主要与下列疾病相鉴别:(1)副脾:发病部位、平扫密度及动脉期强化方式相似,但静脉期强化方式与脾脏表现不符;(2)肾癌:发病部位及强化方式相似,但邻近肾皮质结构完整;(3)嗜铬细胞瘤:血供丰富特点符合,但没有明显坏死。
肌周细胞瘤临床少见,影像学表现缺乏特异性,术前难以正确诊断,最终诊断依靠病理。临床治疗主要以手术切除为主,恶性者需辅助放疗及化疗,但疗效尚不确切,需更多临床病例研究证实,应注意随访。
| [1] | Mentzel T, Dei Tos AP, Sapi Z, et al. Myopericytoma of skin and soft tissues: clinicopathologic and immunohistochemical study of 54 cases[J]. Am J Surg Pathol, 2006, 30(1): 104–13. DOI:10.1097/01.pas.0000178091.54147.b1 |
| [2] | Hunter JB, O'Connell BP, Chow WN, et al. Myopericytoma of the Internal Auditory Canal[J]. Otol Neurotol, 2017, 38(2): e5–e7. DOI:10.1097/MAO.0000000000001281 |
| [3] | Rodriguez D, Cornejo KM, Sadow PM, et al. Myopericytoma tumor of the glans penis[J]. Can J Urol, 2015, 22(3): 7830–3. |
| [4] | Cianciulli TF, Lax JA, Saccheri MC, et al. Primary benign myopericytoma of the left atrium[J]. J Echocardiogr, 2016, 14(3): 130–1. DOI:10.1007/s12574-016-0285-5 |
| [5] | Nagai T, Kamimura T, Itou K, et al. Myopericytoma in urinary bladder: a case report[J]. J Med Case Rep, 2017, 11(1): 46. DOI:10.1186/s13256-017-1226-2 |
| [6] | Chen Z, Liang W. Myopericytoma occurrence in the liver and stomach space: imaging performance[J]. BMC Cancer, 2017, 17(1): 143. DOI:10.1186/s12885-017-3146-3 |
| [7] | Rubino S, De Berardinis R, Colombo D, et al. Myopericytoma of the tongue base: A case report[J]. Acta Otorrinolaringol Esp, 2017, pii: S0001-6519(17)30177-2. |
| [8] | Oliveira RC, Velasco R, Santos GR, et al. Intracranial myopericytoma: a tumour in a rare location[J]. BMJ Case Rep, 2018, 2018, pii: bcr-2017-223111. |
| [9] | Peters K, Caracciolo JT, Henderson-Jackson E, et al. Myopericytoma/myopericytomatosis of the lower extremity in two young patients: a recently designated rare soft tissue neoplasm[J]. Radiol Case Rep, 2017, 13(1): 275–80. |
| [10] | Patrick A, Soares-de-Almeida L, Heinz K. Malignant Myopericytoma: Report of a New Case and Review of the Literature[J]. Am J Dermatopathol, 2016, 38(4): 307–11. DOI:10.1097/DAD.0000000000000463 |
 2018, Vol. 45
2018, Vol. 45


