文章信息
- 张嵚垚, 胡美荣, 孙佳莹, 马淑梅
- ZHANG Qinyao, HU Meirong, SUN Jiaying, MA Shumei
- CHA2DS2-VASc评分对ST段抬高型心肌梗死患者直接PCI术后发生无复流和长期预后的预测价值
- Predictive value of the CHA2DS2-VASc score on the no-reflow phenomenon and long-term prognosis in patients with STEMI after primary percutaneous coronary intervention
- 中国医科大学学报, 2021, 50(4): 356-361
- Journal of China Medical University, 2021, 50(4): 356-361
-
文章历史
- 收稿日期:2020-04-23
- 网络出版时间:2021-04-07 15:10
2. 中国医科大学附属盛京医院 心功能科, 沈阳 110004
2. Department of Cardiac Function, Shengjing hospital of China Medical University, Shengyang 110004, China
目前ST段抬高型心肌梗死(ST-segment elevation myocardial infarction,STEMI) 患者最有效的治疗策略仍是直接经皮冠状动脉介入治疗(percutaneous coronary intervention,PCI),尽快恢复罪犯血管的血流灌注挽救坏死的心肌至关重要。然而,术后的并发症尤其是无复流降低了治疗效果,严重影响患者的预后[1]。有研究[2]表明约5%~10%患者术后会出现无复流现象,寻找一个能够对STEMI患者发生无复流和预后进行危险分层的指标至关重要。CHA2DS2-VASc评分广泛应用于评估非瓣膜性房颤患者发生卒中的风险[3],其包括充血性心力衰竭、高血压、年龄,、卒中或短暂性脑缺血发作、女性、糖尿病和周围血管疾病。评分的组成与动脉粥样硬化、血管痉挛和微血管功能障碍有关,这与无复流和主要不良心血管事件(major adverse cardiovascular events,MACE) 的危险因素相重叠[4]。本研究拟探讨CHA2DS2-VASc评分对STEMI患者直接PCI术后发生无复流现象和长期预后的预测作用。
1 材料与方法 1.1 研究对象连续纳入2017年1月至2018年12月于中国医科大学附属盛京医院行直接PCI治疗的402例STEMI患者。纳入标准: 符合STEMI诊断,参照2015年急性STEMI诊断和治疗指南[5]。排除标准: 心源性休克、严重肝功能和肾功能不全、恶性肿瘤、血液系统疾病、全身免疫性疾病、发病时间 > 24 h。本研究获得中国医科大学附属盛京医院伦理委员会批准。
1.2 研究方法患者入院后立即抽取静脉血送至我院检验科完善血常规、肝肾功能、肌钙蛋白Ⅰ、氨基末端脑钠肽前体等指标的化验。所有PCI手术均由高年资的医师按照标准方法执行,影像记录速度为30帧/s。由2名对本研究不知情的高年资医生采用心肌梗死溶栓治疗(thrombolysis in myocardial infarction,TIMI) 血流分级判断血流灌注程度。
1.3 TIMI血流分级标准0级,造影剂无法通过血管闭塞处;1级,少量造影剂可通过病变处但不能充盈远端血管;2级,造影剂可以充盈远端血管但速度较慢;3级,造影剂可以快速、完全地填充远端血管。无复流现象定义为PCI开通罪犯血管后排除冠状动脉痉挛、血管夹层和血栓栓塞的情况下,TIMI血流分级仍≤2级[6]。
1.4 随访所有纳入患者均采用电话随访方法,所有患者均于2019年12月完成随访,记录MACE事件包括全因死亡、心肌缺血导致的再次血运重建和心力衰竭,中位随访时间为22 (16~28) 个月。
1.5 统计学分析采用SPSS 22.0软件进行统计分析,正态分布计量资料以x±s表示,组间比较采用t检验;非正态分布计量资料以M (P25~P75) 表示,组间比较采用Mann-Whitney U检验。计数资料以例(百分数) 表示,组间比较采用χ2检验。接受者操作特征(reciver operating characteristic,ROC)曲线分析确定CHA2DS2-VASc评分对于无复流现象和长期MACE的预测能力和最佳截断值。组间生存分析采用Kaplan-Meier生存曲线法,生存率比较采用log-rank检验。Logistic回归分析直接PCI术后发生无复流现象的独立危险因素,Cox比例风险模型评价CHA2DS2-VASc评分对于患者预后的影响。P < 0.05为差异有统计学意义。
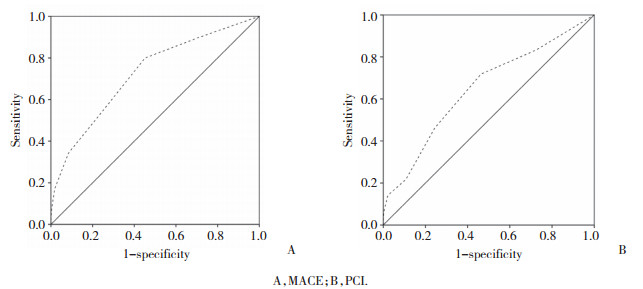
2 结果 2.1 最佳截断值ROC曲线分析结果显示,CHA2DS2-VASc评分预测STEMI患者直接PCI术后长期预后的最佳截断值为CHA2DS2-VASc≥3[曲线下面积(area under the curve,AUC) =0.723,95% CI: 0.656~0.791,P < 0.001],敏感度为70.3%,特异度为87.3%。根据最佳截断值将402例患者分为CHA2DS2-VASc < 3组和CHA2DS2-VASc≥3组,见图 1A。
|
| A, MACE; B, PCI. 图 1 CHA2DS2-VASc评分对于长期随访发生MACE和PCI术后无复流现象的ROC曲线 Fig.1 ROC curve of CHA2DS2-VASc score for MACE during long-term follow-up and for the no-reflow phenomenon |
2.2 2组基线资料比较
CHA2DS2-VASc≥3组患者年龄更大,女性更多,合并糖尿病、卒中或短暂性脑缺血发作和外周血管疾病的比例更高,舒张压和killip心功能分级更高,更易发生无复流。2组充血性心力衰竭史、收缩压和心率无统计学差异。CHA2DS2-VASc≥3组患者的糖化血红蛋白和氨基末端脑钠肽前体更高,而CHA2DS2-VASc < 3组患者肾小球滤过率估计值、中性粒细胞计数和血红蛋白值更高,见表 1。
| Variables | CHA2DS2-VASc < 3 (n = 287) | CHA2DS2-VASc≥3 (n = 115) | P |
| Age (x±s,year) | 56.26±10.89 | 68.02±9.81 | < 0.001 |
| Female sex [n (%)] | 36 (12.5) | 66 (57.4) | < 0.001 |
| Hypertension [n (%)] | 89 (31.0) | 83 (72.2) | < 0.001 |
| Diabetes mellitus [n (%)] | 44 (15.3) | 51 (44.3) | < 0.001 |
| History of stroke/TIA [n (%)] | 5 (1.7) | 40 (34.8) | < 0.001 |
| History of heart failure [n (%)] | 3 (1.0) | 1 (0.9) | 1.000 |
| Vascular disease [n (%)] | 29 (10.1) | 31 (27.0) | < 0.001 |
| SBP (x±s,mmHg) | 120.62±18.30 | 120.39±20.27 | 0.911 |
| DBP (x±s,mmHg) | 76.74±12.30 | 73.89±12.72 | 0.038 |
| Heart rate (x±s,beat/min) | 77.93±13.21 | 76.90±13.21 | 0.494 |
| Creatinine (x±s,μmol/L) | 71.76±19.29 | 69.32±22.72 | 0.276 |
| eGFR [x±s,ml/ (min·1.73m2)] | 99.11±21.10 | 89.39±27.25 | < 0.001 |
| TC (x±s,mmol/L) | 4.64±1.10 | 4.64±1.03 | 0.970 |
| LDL-C (x±s,mmol/L) | 2.97±0.94 | 2.94±0.86 | 0.728 |
| HDL-C (x±s,mmol/L) | 1.03±0.27 | 1.01±0.27 | 0.724 |
| Neutrophil (x±s,109/L) | 8.29±3.54 | 7.58±3.01 | 0.044 |
| Hemoglobin (x±s,g/L) | 144.63±14.23 | 131.35±16.00 | < 0.001 |
| Platelet (x±s,109/L) | 217.15±56.61 | 218.25±58.40 | 0.862 |
| Glycosylated hemoglobin (x±s,%) | 6.14±1.29 | 6.72±1.64 | < 0.001 |
| cTnⅠ (x±s,μg/L) | 0.15(0.02-0.89) | 0.21(0.02-1.3) | 0.590 |
| CK-MB (x±s,ng/mL) | 16(3.5- 47.3) | 16(3.1-70.0) | 0.831 |
| NT-pro BNP (x±s,pg/mL) | 140.5(67-417) | 331(113-915) | < 0.001 |
| Killip class [n (%)] | 0.005 | ||
| 1 | 238 (82.9) | 81 (70.4) | |
| > 1 | 49 (17.1) | 34 (29.6) | |
| No-reflow phenomenon [n (%)] | 42 (14.6) | 36 (31.3) | < 0.001 |
| eGFR,estimated glomerular filtration rate;TIA,transient ischemic attack;SBP,systolic blood pressure;DBP,diastolic blood pressure;TC,total cholesterol;HDL-C,high-density lipoprotein cholesterol;LDL-C,low density lipoprotein cholesterol;cTnⅠ,cardiac troponinⅠ;CK-MB,creatine kinase-myocardial band;NT-pro BNP,NT-pro brain natriuretic peptide. | |||
2.3 PCI
2组冠状动脉造影情况比较,CHA2DS2-VASc≥3组患者病变支数更多,术中更多使用替罗非班、血栓抽吸和球囊反搏,然而使用支架的平均直径要小于CHA2DS2-VASc < 3组。2组患者罪犯血管的分布情况和初始血流的TIMI分级无统计学差异,见表 2。
| Variables | CHA2DS2-VASc < 3 (n = 287) | CHA2DS2-VASc≥3 (n = 115) | P |
| Culprit vessel [n (%)] | 0.552 | ||
| LM | 1 (0.3) | 2 (1.7) | |
| LAD | 146 (50.9) | 60 (52.2) | |
| RCA | 48 (16.7) | 17 (14.8) | |
| LCX | 92 (32.1) | 36 (31.3) | |
| Multivessel disease [n (%)] | 131 (45.6) | 69 (60.0) | 0.009 |
| Initial TIMI flow grade [n (%)] | 0.680 | ||
| 0-1 | 232 (80.8) | 95 (82.6) | |
| ≥2 | 55 (19.2) | 20 (17.3) | |
| Stent length (x±s,mm) | 40.21±20.04 | 39.28±17.92 | 0.666 |
| Stent diameter (x±s,mm) | 3.27±0.44 | 3.15±0.44 | 0.019 |
| Tirofiban infusion [n (%)] | 121 (42.2) | 78 (67.8) | < 0.001 |
| Thrombus aspiration [n (%)] | 41 (14.3) | 26 (22.6) | 0.043 |
| IABP [n (%)] | 3 (1.0) | 7 (6.0) | 0.003 |
| LM,left main;LAD,left anterior descending;LCX,left circumflex;RCA,right coronary artery;IABP,intra-aortic balloon pump;MI,myocardial infarction;TIMI,thrombolysis in myocardial infarction;SD,standard deviation. | |||
2.4 无复流现象
ROC曲线结果显示,AUC为0.648 (95% CI: 0.578~0.718,P < 0.001),最佳截断值为CHA2DS2-VASc≥2,此时的敏感度为71.8%,特异度为53.7% (图 1B)。多因素分析结果显示,CHA2DS2-VASc≥3 (OR = 2.27,95% CI: 1.307~3.960,P = 0.004) 和肾小球滤过率估计值(OR = 0.99,95%CI: 0.98~1.00,P = 0.042) 为无复流的独立预测因子,见表 3。
| Variables | Unadjusted OR (95% CI) | P | Adjusted OR (95% CI) | P |
| CHA2DS2-VASc≥3 | 2.660 (1.59-4.44) | < 0.001 | 2.270 (1.31-3.96) | 0.004 |
| eGFR | 0.980 (0.97-0.99) | 0.001 | 0.990 (0.98-1.00) | 0.042 |
| Neutrophil | 1.060 (0.99-1.14) | 0.102 | - | - |
| Hemoglobin | 0.990 (0.98-1.01) | 0.359 | - | - |
| cTnⅠ | 1.040(1.01-1.08) | 0.011 | 1.030 (1.00-1.06) | 0.101 |
| CK-MB | 1.003 (1.00-1.01) | 0.038 | 1.001(1.00-1.01) | 0.364 |
| NT-pro BNP | 1.000 (1.00-1.00) | 0.015 | 1.000 (1.00-1.00) | 0.688 |
| killip > 1 | 2.530(1.46-4.38) | 0.001 | 1.596 (0.82-1.01) | 0.166 |
| CK-MB,creatine kinase-myocardial band;eGFR,estimated glomerular filtration rate;cTnⅠ,cardiac troponinⅠ;NT-pro BNP,NT-pro brain natriuretic peptide;CI,confidence interval. | ||||
2.5 主要不良心血管事件
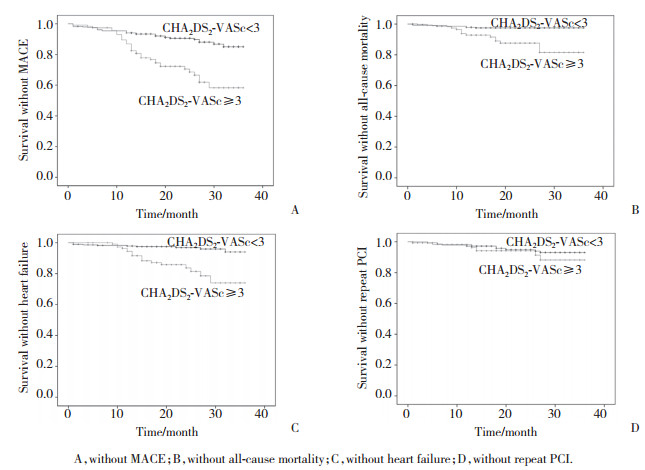
2组患者经中位随访时间22 (16~28) 个月的随访后所发生的不良事件如表 4所示。在MACE、心力衰竭和全因死亡发生率方面2组有统计学差异,但2组在再次血运重建方面并无统计学差异。Kaplan-Meier生存分析结果显示,评分高值组患者发生MACE、心力衰竭和全因死亡的风险远高于评分低值组(P均 < 0.001,图 2A、2B、2C),而2组患者再次血运重建风险却无统计学差异(P = 0.343,图 2D)。多因素Cox回归分析结果显示,血红蛋白、肾小球滤过率估计值、killip分级和CHA2DS2-VASc≥3均是发生MACE的独立预测因子,见表 5。
| Variables | CHA2DS2-VASc≤2 (n = 287) | CHA2DS2-VASc > 2 (n = 115) | P |
| All-cause mortality | 7 (2.4) | 14 (12.0) | < 0.001 |
| Cardiovascular mortality | 3 (1.0) | 10 (8.7) | < 0.001 |
| Heart failure | 11(3.8) | 15 (13.0) | 0.001 |
| Repeat PCI | 15 (5.2) | 8 (7.0) | 0.500 |
| MACE | 33 (11.5) | 37 (32.2) | < 0.001 |
|
| A, without MACE; B, without all-cause mortality; C, without heart failure; D, without repeat PCI. 图 2 2组患者的Kaplan-Meier生存分析 Fig.2 Kaplan-Meier survival analysis of the two groups |
| Variables | Univariate HR (95% CI) | P | Multivariate HR (95% CI) | P |
| CHA2DS2-VASc≥3 | 3.16 (1.97-5.06) | < 0.001 | 1.88 (1.10-3.22) | 0.020 |
| eGFR | 0.98 (0.97-0.99) | < 0.001 | 0.99 (0.98-1.00) | 0.049 |
| Neutrophil | 1.03(0.97-1.10) | 0.357 | - | - |
| Hemoglobin | 0.97(0.95-0.98) | < 0.001 | 0.98 (0.96-1.00) | 0.048 |
| cTnⅠ | 0.97(0.94-1.04) | 0.582 | - | - |
| NT-pro BNP | 1.00(1.00-1.00) | < 0.001 | 1.00 (1.00-1.00) | 0.254 |
| killip > 1 | 2.91(1.79-4.71) | < 0.001 | 1.99 (1.16-3.41) | 0.013 |
| eGFR,estimated glomerular filtration rate;cTnⅠ,cardiac troponinⅠ;NT-pro BNP,NT-pro brain natriuretic peptide. | ||||
3 讨论
无复流现象是直接PCI术后的严重并发症之一,研究[7]表明无复流的发生可加重心肌缺血、扩大心肌梗死面积,增加心力衰竭的发生,是近期和远期不良预后的预测因子。目前无复流的病理生理机制尚未完全清楚,但认为与缺血-再灌注损伤、远端血管栓塞、微血管的结构与功能改变和神经功能紊乱等有关[8]。1项研究连续纳入428例非ST段抬高型心肌梗死患者,无复流组患者CHA2DS2-VASc评分要明显高于正常血流组,高CHA2DS2-VASc评分是无复流的独立预测因子,且最佳截断值为3时,敏感度为80.9%,特异度为74.6%[9]。MIRBOLOUK等[10]研究发现CHA2DS2-VASc评分可以独立预测无复流现象,且CHA2DS2-VASc≥2时敏感度为88%,特异度为67%。本研究同样发现CHA2DS2-VASc评分是无复流的独立预测因子但最佳截断值却为CHA2DS2-VASc≥3,敏感度为71.8%,特异度为53.7%。研究结果的不同可能由于本研究纳入的患者为亚洲人而MIRBOLOUK等[10]的研究多为欧美人。
既往有大量研究[11-13]表明CHA2DS2-VASc评分中的每个组成部分均对急性冠状动脉综合征患者预后有影响。PENG等[12]研究发现在院期间和远期的MACE发生随着CHA2DS2-VASc评分的增长而增长,并且CHA2DS2-VASc评分对于MACE具有独立预测价值。BOZBAY等[14]发现CHA2DS2-VASc评分高值组患者在院期间和长期死亡率更高。通过ROC曲线发现最佳截断值为CHA2DS2-VASc > 2 (AUC= 0.821,95% CI: 0.76~0.89,P < 0.001),敏感度为61.1%,特异度为82.8%。本研究同样证实CHA2DS2-VASc≥3是预测MACE的最佳截断值且敏感度为70.3%,特异度为87.3%。Kaplan-Meier生存分析结果显示,CHA2DS2-VASc≥3的STEMI患者发生全因死亡和心力衰竭的可能性更大,而再次血运重建发生率2组并无统计学差异。提示CHA2DS2-VASc评分可能更加适合作为STEMI患者直接PCI术后发生全因死亡和心力衰竭的危险分层标准,而对于再次血运重建的发生需要采取其他方法评估。
| [1] |
MORISHIMA I, SONE T, OKUMURA K, et al. Angiographic no-reflow phenomenon as a predictor of adverse long-term outcome in patients treated with percutaneous transluminal coronary angioplasty for first acute myocardial infarction[J]. J Am Coll Cardiol, 2000, 36(4): 1202-1209. DOI:10.1016/s0735-1097(00)00865-2 |
| [2] |
DURANTE A, CAMICI PG. Novel insights into an "old" phenomenon: the no reflow[J]. Int J Cardiol, 2015, 187: 273-280. DOI:10.1016/j.ijcard.2015.03.359 |
| [3] |
杨蕾, 高可, 付博文, 等. 血液生物标志物联合CHA2DS2-VASc评分对非瓣膜性心房颤动患者发生急性脑梗死的预测价值[J]. 中国医刊, 2020, 55(1): 31-35. DOI:10.3969/j.issn.1008-1070.2020.01.009 |
| [4] |
CHAN YH, YIU KH, LAU KK, et al. The CHADS2 and CHA2DS2-VASc scores predict adverse vascular function, ischemic stroke and cardiovascular death in high-risk patients without atrial fibrillation: role of incorporating PR prolongation[J]. Atherosclerosis, 2014, 237(2): 504-513. DOI:10.1016/j.atherosclerosis.2014.08.026 |
| [5] |
中华医学会心血管病学分会, 中华心血管病杂志编辑委员会. 急性ST段抬高型心肌梗死诊断和治疗指南[J]. 中华心血管病杂志, 2010, 38(8): 675-690. DOI:10.3760/cma.j.issn.0253-3758.2010.08.002 |
| [6] |
HUANG D, GAO W, WU R, et al. D-dimer level predicts in-hospital adverse outcomes after primary PCI for ST-segment elevation myocardial infarction[J]. Int J Cardiol, 2020, 305: 1-4. DOI:10.1016/j.ijcard.2020.02.010 |
| [7] |
FAJAR JK, HERIANSYAH T, ROHMAN MS. The predictors of no reflow phenomenon after percutaneous coronary intervention in patients with ST elevation myocardial infarction: a meta-analysis[J]. Indian Heart J, 2018, 70(Suppl 3): S406-S418. DOI:10.1016/j.ihj.2018.01.032 |
| [8] |
张嵚垚, 马淑梅. 冠状动脉无复流机制及预测的研究进展[J]. 医学综述, 2019, 25(22): 4473-4476, 4482. DOI:10.3969/j.issn.1006-2084.2019.22.021 |
| [9] |
BARMAN HA, KAHYAOGLU S, DURMAZ E, et al. The CHADS-VASc score is a predictor of no-reflow in patients with non-ST-segment elevation myocardial infarction[J]. Coron Artery Dis, 2020, 31(1): 7-12. DOI:10.1097/mca.0000000000000781 |
| [10] |
MIRBOLOUK F, GHOLIPOUR M, SALARI A, et al. CHA2DS2-VASc score predict No-reflow phenomenon in primary percutaneous coronary intervention in primary percutaneous coronary intervention[J]. J Cardiovasc Thorac Res, 2018, 10(1): 46-52. DOI:10.15171/jcvtr.2018.08 |
| [11] |
JHUND PS, MACINTYRE K, SIMPSON CR, et al. Long-term trends in first hospitalization for heart failure and subsequent survival between 1986 and 2003[J]. Circulation, 2009, 119(4): 515-523. DOI:10.1161/circulationaha.108.812172 |
| [12] |
PENG H, SUN Z, CHEN H, et al. Usefulness of the CHA2DS2-VASc score to predict adverse outcomes in acute coronary syndrome patients without atrial fibrillation undergoing percutaneous coronary intervention[J]. Am J Cardiol, 2019, 124(4): 476-484. DOI:10.1016/j.amjcard.2019.05.036 |
| [13] |
PANCHOLY SB, SHANTHA GP, PATEL T, et al. Sex differences in short-term and long-term all-cause mortality among patients with ST-segment elevation myocardial infarction treated by primary percutaneous intervention: a meta-analysis[J]. JAMA Intern Med, 2014, 174(11): 1822-1830. DOI:10.1001/jamainternmed.2014.4762 |
| [14] |
BOZBAY M, UYAREL H, CICEK G, et al. CHA2DS2-VASc score predicts in-hospital and long-term clinical outcomes in patients with ST-segment elevation myocardial infarction who were undergoing primary percutaneous coronary intervention[J]. Clin Appl Thromb Hemost, 2017, 23(2): 132-138. DOI:10.1177/1076029616646874 |
 2021, Vol. 50
2021, Vol. 50




