文章信息
- 安静, 洪林巍
- AN Jing, HONG Linwei
- 二维斑点追踪技术评价前驱糖尿病患者的左心房功能
- Evaluation of Left Atrial Function in Patients with Prediabetes by Two-Dimensional Speckle Tracking Echocardiography
- 中国医科大学学报, 2019, 48(7): 619-623, 628
- Journal of China Medical University, 2019, 48(7): 619-623, 628
-
文章历史
- 收稿日期:2019-04-15
- 网络出版时间:2019-07-15 10:54
2. 辽宁中医药大学 附属医院超声科, 沈阳 110032
2. Department of Ultrasound, The Affiliated Hospital of Liaoning University of Traditional Chinese Medicine, Shenyang 110032, China
前驱糖尿病(prediabetes, PD)是指存在葡萄糖代谢障碍, 但尚未达到Ⅱ型糖尿病的诊断标准[1]。由于PD发展为糖尿病的风险极高, 而心血管并发症是糖尿病致死和致残的主要原因, 因而早期监测PD患者的心脏功能, 进而积极干预并早期预防糖尿病及心血管事件的发生, 具有重要的临床意义。研究[2]表明, Ⅱ型糖尿病患者左心室舒张功能减低, 而PD患者左心室舒张功能是否已受累目前尚不明确。由于左心房功能与左心室舒张功能相互影响、相互依赖, PD患者左心房功能是否受损亦未证实。
传统超声心动图通过测量心房容积并计算心房射血分数来评估心房功能, 易受心房负荷的影响, 只能间接反映心房心肌的功能。而二维斑点追踪技术可测量心房心肌的应变和应变率, 直接反映心房心肌的形变, 不依赖于心房负荷和几何形态假设, 可全面、客观地评价整个心动周期内心房心肌的储备功能、通道功能和泵功能。本研究旨在采用二维斑点追踪技术检测左心房心肌纵向应变和应变率评价PD患者的左心房功能, 并探讨左心房功能与空腹血糖(fasting plasma glucose, FPG)、口服葡萄糖耐量试验(oral glucose tolerance test, OGTT)和糖化血红蛋白(glycosylated hemoglobin, HbA1c)水平之间的关系, 为临床早期检测PD患者的心脏功能、早期制定干预方案及判断预后提供理论依据。
1 材料与方法 1.1 研究对象选择2018年1月至2018年12月我院诊断为PD的患者60例作为PD组, 其中男35例, 女25例; 平均年龄(55.7±8.1)岁。PD的诊断标准[3]: 5.6 mmol/L < FPG < 7.0 mmol/L和(或) 7.8 mmol/L < OGTT < 11.1 mmol/L和(或) 5.7% < HbA1c < 6.4%。排除标准:糖尿病或使用糖尿病药物; 既往心肌梗死; 既往冠状动脉介入治疗或溶栓治疗; 高血压、心脏瓣膜病、先天性心脏病、心律失常、缺血或出血性脑血管病病史; 慢性阻塞性肺疾病、慢性肺源性心脏病; 肝肾功能不全; 肿瘤; 自身免疫性疾病; 甲状腺功能异常症; 超声心动图图像质量欠佳等。
选择性别、年龄、一般临床状况匹配的FPG正常的健康成年人40例作为对照组, 其中男20例, 女20例; 平均年龄(56.5±8.3)岁。排除标准同PD组。
1.2 研究方法 1.2.1 收集一般临床资料常规测量身高、体质量, 计算体质量指数(body mass index, BMI)。在安静状态下测量3次血压, 并取平均值。
1.2.2 生化检验所有研究对象均禁食12 h, 于次日早晨空腹抽取肘静脉血, 采用标准方法检测FPG、血肌酐、总胆固醇和甘油三酯水平等, 并立即检测FPG及HbA1c。采用葡萄糖氧化酶法(Glamour2000自动生化分析仪, 上海科华生物工程有限公司)检测FPG; 采用高压液相法(Variant Ⅱ血红蛋白检测仪, 上海Bio-Rad公司)检测HbA1c;采用标准方法检测OGTT。
1.2.3 超声心动图采用Philips IE33超声诊断仪, S5-1探头, 频率2~4 MHz。嘱患者左侧卧位, 同步连接体表心电图。采集多普勒静态图像, 以及胸骨旁左心室长轴切面、心尖四腔心切面和心尖两腔心切面连续3个心动周期的动态图像。采集时注意各动态切面心内膜清晰显示。二维帧频约56~85帧/s。
1.2.3.1 常规超声心动图参数根据美国超声心动图学会指南[4], 测量左心室舒张末容积(left ventricular end-diastolic volume, LVEDV)、左心室射血分数(left ventricular ejection fraction, LVEF)、二尖瓣舒张早期血流速度(mitral early diastolic flow velocity, mitral E)、二尖瓣舒张晚期血流速度(mitral late diastolic flow velocity, mitral A)、三尖瓣反流峰值速度(tricuspid regurgitation peak velocity, TRPV)、二尖瓣环间隔部位舒张早期峰值速度(mitral annulus early diastolic velocity at septal wall of left ventricle, mitral sept e')、二尖瓣环侧壁部位舒张早期峰值速度(mitral annulus early diastolic velocity at lateral wall of left ventricle, mitral lat e'), 并计算mitral E/A、二尖瓣环舒张早期运动速度平均值(mitral average e')和mitral E/e'。
采用双平面Simpson法测量左心房容积, 包括二尖瓣开放前左心房最大容积(left atrial maximum volume, LAVmax); 心电图p波前左心房容积, 即左心房收缩前容积(left atrial pre-contraction volume, LAVp); 二尖瓣关闭前左心房最小容积(left atrial minimum volume, LAVmin)。并根据体表面积校正LAVmax, 获得左心房容积指数(left atrium maximum volume index, LAVI)。根据左心房容积计算左心房射血分数, 左心房整体射血分数(left atrial total ejection fraction, LAtotalEF) = (LAVmax-LAVmin) / LAVmax; 左心房主动射血分数(left atrial active ejection fraction, LAactiveEF) = (LAVp-LAVmin) / LAVp; 左心房被动射血分数(left atrial passive ejection fraction, LApassiveEF) = (LAVmax-LAVp) / LAVmax。
1.2.3.2 二维斑点追踪技术参数通过Qlab工作站进行脱机分析, 观察左心室心尖四腔心切面图像, 于收缩末期手动勾画左心房心内膜边界, 软件自动生成感兴趣区域(regions of interest, ROI), 手动调整ROI宽度, 使其与左心房心肌厚度一致, 软件自动逐帧追踪左心房心肌运动, 得到左心房心肌的整体纵向应变-时间曲线, 调整基线使左心室舒张末期时左心房纵向应变为0, 分别测量左心房储备期纵向应变(left atrial longitudinal strain during reservoir phase, LASr)和应变率(left atrial longitudinal strain rate during reservoir phase, LASRr)、左心房通道期纵向应变(left atrial longitudinal strain during conduit phase, LAScd)和应变率(left atrial longitudinal strain rate during conduit phase, LASRcd)以及左心房收缩期纵向应变(left atrial longitudinal strain during contraction phase, LASct)和应变率(left atrial longitudinal strain rate during contraction phase, LASRct)。见图 1。
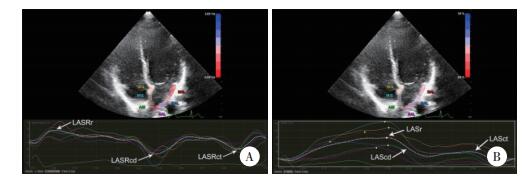
|
| A, longitudinal strain; B, longitudinal strain rate. 图 1 二维斑点追踪技术测量左心房纵向应变和应变率 Fig.1 Two-dimensional speckle tracking technique for measuring the left atrial longitudinal strain and strain rate |
1.3 统计学分析
采用SPSS 23.0统计学软件进行分析。计量资料以x±s表示, 组间比较采用独立样本t检验; 计数资料以百分比表示, 组间比较采用χ2检验。P < 0.05为差异有统计学意义。
2 结果 2.1 一般临床特征的比较2组比较, 一般特征如年龄、性别以及BMI等无统计学差异(P > 0.05)。PD组FPG、总胆固醇、低密度脂蛋白胆固醇、HbA1c均高于对照组(P < 0.05)。见表 1。
| Clinical characteristic | PD group (n = 60) | Control group (n = 40) | P |
| Age (year) | 55.7±8.1 | 56.5±8.3 | 0.500 |
| Male [n (%)] | 35(58) | 20(50) | 0.470 |
| Body surface area (m2) | 1.71±0.15 | 1.72±0.17 | 0.740 |
| BMI (kg/m2) | 23.8±3.0 | 22.5±3.3 | 0.140 |
| Heart rate (beat/min) | 67.8±7.9 | 65.0±7.3 | 0.510 |
| SBP (mmHg) | 124.8±12.8 | 126.9±14.5 | 0.430 |
| DBP (mmHg) | 76.7±9.6 | 78.8±8.9 | 0.620 |
| FPG (mmol/L) | 6.91±1.38 | 5.36±1.26 | 0.002 |
| LDL-c (mmol/L) | 3.23±0.79 | 2.73±0.85 | 0.001 |
| TG (mmol/L) | 1.45±0.71 | 1.40±0.86 | 0.770 |
| TC (mmol/L) | 5.05±0.71 | 4.33±0.81 | 0.030 |
| HDL-c (mmol/L) | 1.15±0.29 | 1.17±0.27 | 0.530 |
| HbA1c (%) | 6.20±0.80 | 4.30±0.90 | 0.010 |
| BMI, body mass index; HR, heart rate; SBP, systolic blood pressure; DBP, diastolic blood pressure; FPG, fasting plasma glucose; LDL-C, low-density lipoprotein cholesterol; TG, triglyceride; TC, total cholesterol; HDL-C, high-density lipoprotein cholesterol; HbA1c, glycated hemoglobin. | |||
2.2 左心室功能的比较
左心室收缩功能比较: 2组间LVEDV、LVEF无统计学差异(P > 0.05)。左心室舒张功能比较: 2组间LAVI、mitral A及TRPV无统计学差异(P > 0.05)。与对照组比较, PD组mitral E、mitral sept e'、mitral lat e'、mitral average e'和mitral E/A显著减低(P < 0.05), mitral E/e'显著增大(P < 0.05)。见表 2。
| Parameter | PD group (n = 60) | Control group (n = 40) | P |
| LVEDV (mL) | 48.29±4.32 | 48.00±3.47 | 0.710 |
| LVEF (%) | 61.89±3.74 | 63.24±4.31 | 0.110 |
| LAVI (mL/m2) | 30.40±2.55 | 28.51±2.10 | 0.290 |
| TRPV (m/s) | 0.23±0.06 | 0.21±0.08 | 0.230 |
| Mitral E (m/s) | 0.65±0.16 | 0.73±0.18 | 0.010 |
| Mitral A (m/s) | 0.71±0.16 | 0.69±0.13 | 0.370 |
| Mitral E/A | 0.94±0.28 | 1.13±0.33 | 0.002 |
| Mitral sept e' (cm/s) | 4.94±2.04 | 7.44±2.42 | 0.010 |
| Mitral lat e' (cm/s) | 6.17±1.40 | 9.13±1.52 | 0.006 |
| Mitral average e' (cm/s) | 5.64±1.71 | 8.32±1.89 | 0.009 |
| Mitral E/e' | 11.53±2.39 | 8.87±2.64 | 0.010 |
| LVEDV, left ventricular end-diastolic volume; LVEF, left ventricular ejection fraction; mitral E, mitral early diastolic flow velocity; mitral A, mitral late diastolic flow velocity; TR, tricuspid regurgitation velocity; mitral septal e', mitral septal annular early diastolic velocity; mitral lateral e', mitral lateral annular early diastolic velocity. | |||
2.3 左心房功能的比较
2组比较, LAVmax、LAVp和LAVmin无统计学差异(P > 0.05), LAtotalEF、LAactiveEF和LApassiveEF无统计学差异(P > 0.05)。与对照组相比, PD组LAScd和LASRcd减低(P < 0.05)。2组比较, LASr、LASRr、LASct和LASRct无统计学差异(P > 0.05)。见表 3。
| Parameter | PD group (n = 60) | Control group (n = 40) | P |
| LAVmax (mL) | 52.52±8.45 | 48.41±9.04 | 0.15 |
| LAVp (mL) | 35.84±6.36 | 35.43±5.83 | 0.42 |
| LAVmin (mL) | 17.41±4.37 | 18.72±4.89 | 0.22 |
| LAtotalEF (%) | 50.72±9.33 | 53.12±8.17 | 0.09 |
| LAactiveEF (%) | 35.85±6.78 | 36.53±7.94 | 0.13 |
| LApassiveEF (%) | 25.91±9.65 | 24.36±6.81 | 0.54 |
| LASr (%) | 27.48±6.88 | 26.75±5.84 | 0.31 |
| LASRr (s-1) | 1.42±0.45 | 1.40±0.52 | 0.44 |
| LAScd (%) | 14.88±5.37 | 16.02±4.74 | 0.01 |
| LASRcd (s-1) | -1.20±0.31 | -1.41±0.47 | 0.02 |
| LASct (%) | 12.34±4.01 | 11.94±3.68 | 0.19 |
| LASRct (s-1) | -1.81±0.52 | -1.74±0.47 | 0.26 |
| LAVmax, left atrial maximum volume; LAVp, left atrial pre-contraction volume; LAVmin, left atrial minimum volume; LAtotalEF, left atrial total ejection fraction; LAactiveEF, left atrial active ejection fraction; LApassiveEF, left atrial passive ejection fraction; LASr, left atrial longitudinal strain during the reservoir phase; LASRr, left atrial longitudinal strain rate during the reservoir phase; LAScd, left atrial longitudinal strain during the conduit phase; LASRcd, left atrial longitudinal strain rate during the conduit phase; LASct, left atrial longitudinal strain during the contraction phase; LASRct, left atrial longitudinal strain rate during the contraction phase. | |||
2.4 相关性分析
PD患者中, HbA1c与LAScd呈负相关(r = -0.69, P < 0.001), HbA1c与LASRcd呈正相关(r = 0.57, P < 0.001), 见图 3。PD患者中, FPG、OGTT与LAScd、LASRcd均无显著相关性(P > 0.05)。
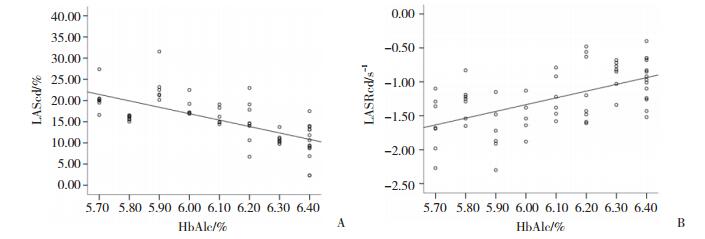
|
| A, correlation of HbA1c level with LAScd; B, correlation of HbA1c level with LASRcd. 图 2 PD患者中HbA1c与LAScd、LASRcd的相关性 Fig.2 Correlation of HbA1c level with LAScd and LASRcd in the PD patients |
3 讨论
糖尿病已成为全球最普遍的慢性病之一, 且心血管并发症已成为Ⅱ型糖尿病患者死亡的首要原因[5]。由于PD发病隐匿, 且极易发展为糖尿病, 因而早期评价PD患者的心脏功能, 进而早期进行积极的临床干预具有重要的临床意义[6]。
研究[7-8]表明, 糖尿病患者心肌发生病理性变化, 即心肌内糖蛋白胶原纤维沉积、心肌间质纤维化, 进而导致心肌变性僵硬, 从而导致左心室舒张功能减低。本研究发现, PD患者虽然存在糖代谢异常, 并未达到糖尿病的诊断标准, 但是PD患者左心室舒张功能也已经受损。左心房功能与左心室舒张功能相互影响、相互依赖, 然而目前PD患者左心房功能是否受损尚不明确。
传统超声心动图通过测量心房容积并计算心房射血分数来评估心房功能, 但易受心房负荷的影响, 只能间接反映心房心肌的功能[9]。本研究采用传统超声心动图测量左心房容积并计算射血分数来评价PD患者的左心房功能, 但与对照组相比无统计学差异。二维斑点追踪技术可以实时追踪左心房心肌内回声斑点的空间运动, 定量分析左心房心肌的形变能力及运动特征, 不受相邻心肌节段运动的干扰, 无角度依赖性, 因而可以更加准确、早期反映左心房心肌在整个心动周期不同时相的功能[10]。
左心房功能包括: (1)储备功能, 左心室收缩期, 肺静脉血汇入左心房, 此时左心房起到储备血液的作用; (2)通道功能, 左心室舒张早期, 二尖瓣开放, 左心房血通过二尖瓣流入左心室, 此时左心房起到传导血流的作用; (3)泵功能, 左心室舒张晚期, 左心房心肌自身收缩, 将左心房内血液进一步排入左心室, 此时左心房起到把血液主动泵入左心室的作用[11]。本研究发现, PD患者通道功能减低, 其可能原因为左心室舒张功能减低, 导致左心室舒张压升高, 进而影响左心房被动排空, 从而影响左心房通道功能。研究[12]表明, 与FPG和OGTT相比, HbA1c在诊断PD时具有更高的敏感度。本研究发现, PD患者中HbA1c与左心房通道功能密切相关, 而与FPG和OGTT无显著相关性, 表明左心房通道功能可早期检测PD患者心脏功能, 可以敏感反映患者病情。
综上所述, PD患者左心房通道功能和左心室舒张功能均减低, 且左心房通道功能与HbA1c水平有关。临床上应密切关注PD患者, 及时给予临床干预, 并进行密切随访。
| [1] |
ABDI H, HOSSEINPANAH F, AZIZI F, et al. Screening for dysglycemia:a comment on classification and diagnosis of diabetes in American Diabetes Association standards of medical care in diabetes-2016[J]. Arch Iran Med, 2017, 20(6): 389. |
| [2] |
AMERICAN DIABETES ASSOCIATION. 2. Classification and diagnosis of diabetes:standards of medical care in diabetes-2019[J]. Diabetes Care, 2019, 42(Suppl 1): S13-S28. DOI:10.2337/dc19-S002 |
| [3] |
BUGGEY J, HOIT BD. Left atrial strain:measurement and clinical application[J]. Curr Opin Cardiol, 2018, 33(5): 479-485. DOI:10.1097/HCO.0000000000000537 |
| [4] |
CARRIS NW, MAGNESS RR, LABOVITZ AJ. Prevention of diabetes mellitus in patients with prediabetes[J]. Am J Cardiol, 2019, 123(3): 507-512. DOI:10.1016/j.amjcard.2018.10.032 |
| [5] |
DE GREGORIO C, DATTILO G, CASALE M, et al. Left atrial morphology, size and function in patients with transthyretin cardiac amyloidosis and primary hypertrophic cardiomyopathy-comparative strain imaging study[J]. Circ J, 2016, 80(8): 1830-1837. DOI:10.1253/circj.CJ-16-0364 |
| [6] |
DI PINO A, MANGIAFICO S, URBANO F, et al. HbA1c identifies subjects with prediabetes and subclinical left ventricular diastolic dysfunction[J]. J Clin Endocrinol Metab, 2017, 102(10): 3756-3764. DOI:10.1210/jc.2017-00954 |
| [7] |
FREIRE CM, MOURA AL, BARBOSA MDE M, et al. Left ventricle diastolic dysfunction in diabetes:an update[J]. Arq Bras Endocrinol Metabol, 2007, 51(2): 168-175. DOI:10.1590/S0004-27302007000200005 |
| [8] |
KARAKURT A, YILDIZ C, YILDIZ A, et al. Early detection strain/strain rate and time to strain/strain rate abnormalities for left atrial mechanical function in hypertensive patients[J]. Acta Cardiol, 2019, 74(2): 141-151. DOI:10.1080/00015385.2018.1475031 |
| [9] |
LANG RM, BADANO LP, MOR-AVI V, et al. Recommendations for cardiac chamber quantification by echocardiography in adults:an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging[J]. Eur Heart J Cardiovasc Imaging, 2015, 16(3): 233-270. DOI:10.1093/ehjci/jev014 |
| [10] |
LEUNG M, PHAN V, LEUNG DY. Endothelial function and left ventricular diastolic functional reserve in type 2 diabetes mellitus[J]. Open Heart, 2014, 1(1): e000113. DOI:10.1136/openhrt-2014-000113 |
| [11] |
MARTINEZ LC, SHERLING D, HOLLEY A. The screening and prevention of diabetes mellitus[J]. Prim Care, 2019, 46(1): 41-52. DOI:10.1016/j.pop.2018.10.006 |
| [12] |
POULSEN MK, HENRIKSEN JE, DAHL J, et al. Left ventricular diastolic function in type 2 diabetes mellitus:prevalence and association with myocardial and vascular disease[J]. Circ Cardiovasc Imaging, 2010, 3(1): 24-31. DOI:10.1161/CIRCIMAGING.109.855510 |
 2019, Vol. 48
2019, Vol. 48




