2. 山东第一医科大学第一附属医院(山东省千佛山医院),山东 济南 250014;
3. 山东医学高等专科学校,山东 济南 250000
2. The First Affiliated Hospital of Shandong First Medical University & Shandong Provincial Qianfoshan Hospital, Jinan 250014 China;
3. Shandong Medical College, Jinan 250000 China
甲状旁腺功能亢进症(Hyperparathyropathy,HPT)是由于甲状旁腺分泌甲状旁腺激素(PTH)过多,继而导致钙磷代谢紊乱,并累及多个器官和系统的一种常见内分泌性疾病。甲状腺功能亢进按照其病因可以分为原发性甲状旁腺功能亢进症(PHPT)和继发性甲状旁腺功能亢进症(SHPT)。
PTH的分泌主要受血清钙、磷、骨化三醇(1,25-二羟维生素D3)及成纤维细胞生长因子23(fibroblast growth factor 23,FGF23)调节。在生理条件下,血清钙磷水平受机体负反馈调节,该调解机制在PHPT和SHPT中继续发挥其作用[1]。在慢性肾病(CKD)中,低浓度骨化三醇和低钙血症共同刺激甲状旁腺分泌PTH,并导致甲状旁腺增生和SHPT;PHPT病因主要是甲状旁腺腺瘤,2种HPT病程发展到一定阶段均需要手术。MIBI显像一直是手术前的常规检查,特别是在甲状旁腺微创切除之前。关于血清钙磷水平、甲状旁腺激素变化与MIBI显像阳性的关系有很多讨论,但结论不一。本研究旨在探讨HPT患者血清钙磷水平、甲状旁腺激素与MIBI显像阳性的可能关系,以及HTP血清钙磷水平与甲状旁腺激素的相关性。
1 材料与方法 1.1 研究对象回顾性分析2017年9月—2019年9月共234例行99Tcm-MIBI SPECT/CT显像的临床怀疑HPT患者资料,原发性甲状旁腺功能亢进共62人,年龄29~75岁(中位数52.5岁),男21人,女41人,继发性甲状旁腺功能亢进共172人,年龄13~71岁(中位数46岁),男100人,女72人。纳入标准:①甲状旁腺激素高于正常值;②术前进行甲状旁腺99Tcm-MIBI SPECT/CT显像;③血液生化检查为MIBI显像前1周内的;④手术病理资料齐全;⑤继发性甲状旁腺功能亢进病因均为慢性肾脏病。
1.2 显像方法采用GE公司的Infinia Hawkeye4,采用低能高分辨准直器,静脉注射740 Mbq 99Tcm-MIBI(北京原子高科股份有限公司),放射性药物标记按其说明书进行。患者取仰卧位,充分暴露颈前区域,分别于注射后15 min(早期相)和120 min(延迟相)进行扫描。两期采集参数相一致,放大倍数为1.00,矩阵64 × 64。延迟相采集结束进行SPECT断层采集及CT扫描,CT扫描参数:电压140 kV,电流2.5 mA,扫描层厚5.0 mm。SPECT/CT图像融合程序为仪器自带软件。
1.3 99Tcm-MIBI平面显像及SPECT/CT断层融合显像结果判定标准MIBI显像结果由2位核医学科主治及以上医师以视觉判定方式共同阅片,诊断意见不同时讨论获得一致结果。平面显像延迟期可见甲状旁腺区结节状放射性浓聚即判定为阳性,断层融合显像发现甲状旁腺区软组织密度影伴放射性浓聚即判定为阳性,双时相显像结果以断层融合显像结果为准。
1.4 血清生化检查正常血清PTH水平为10.0~65.0 pg/mL,血清总钙水平为2.25~2.75 mmoL/L,血清磷水平为0.87~1.45 mmol/L,高于正常值判定阳性。
1.5 统计学处理采用SPSS 23.0软件处理数据。各生化检查值均不符合正态分布,统计描述采用中位数,两组间比较采用Mann-Whitney U检验。采用二分类的Logistic回归分析99Tcm-MIBI显像结果的影响因素,筛选出影响因素后行Spearman相关性分析,并绘制ROC诊断曲线计算最大曲线下面积和自变量的Cut-off值。绘制血清钙、磷与PTH的散点图并行相关性分析。
2 结 果 2.1 PHPT组与SHPT组血清钙、磷、PTH的统计学分析PHPT和SHPT分别为62例和172例,PHPT和SHPT2组MIBI显像结果阴性分别为14例和1例(图1),PHPT和SHPT2组MIBI显像结果阳性分别为48例和171例(图2),2组PTH水平分别为210.93(122.60~529.20)pg/mL和1842.50(1342.50~2345.00) pg/mL,2组间差异有统计学意义(Z = −10.83,P = 0.000),SHPT组显著高于PHPT组;2组血清钙水平分别为2.86(2.65~3.15)mmol/L和2.43(2.32~2.58)mmol/L,2组间差异有统计学意义(Z = −7.52,P = 0.000),PHTP组显著高于SHPT组;2组血清磷水平分别为0.80(0.64~1.03)mmol/L和2.26(1.97~2.63)mmol/L,2组间差异有统计学意义(Z = −10.15,P = 0.000),PHTP组显著低于SHPT组(表1)。
|
|
表 1 临床特征和实验室结果 Table 1 Clinical characteristics and laboratory results |
|
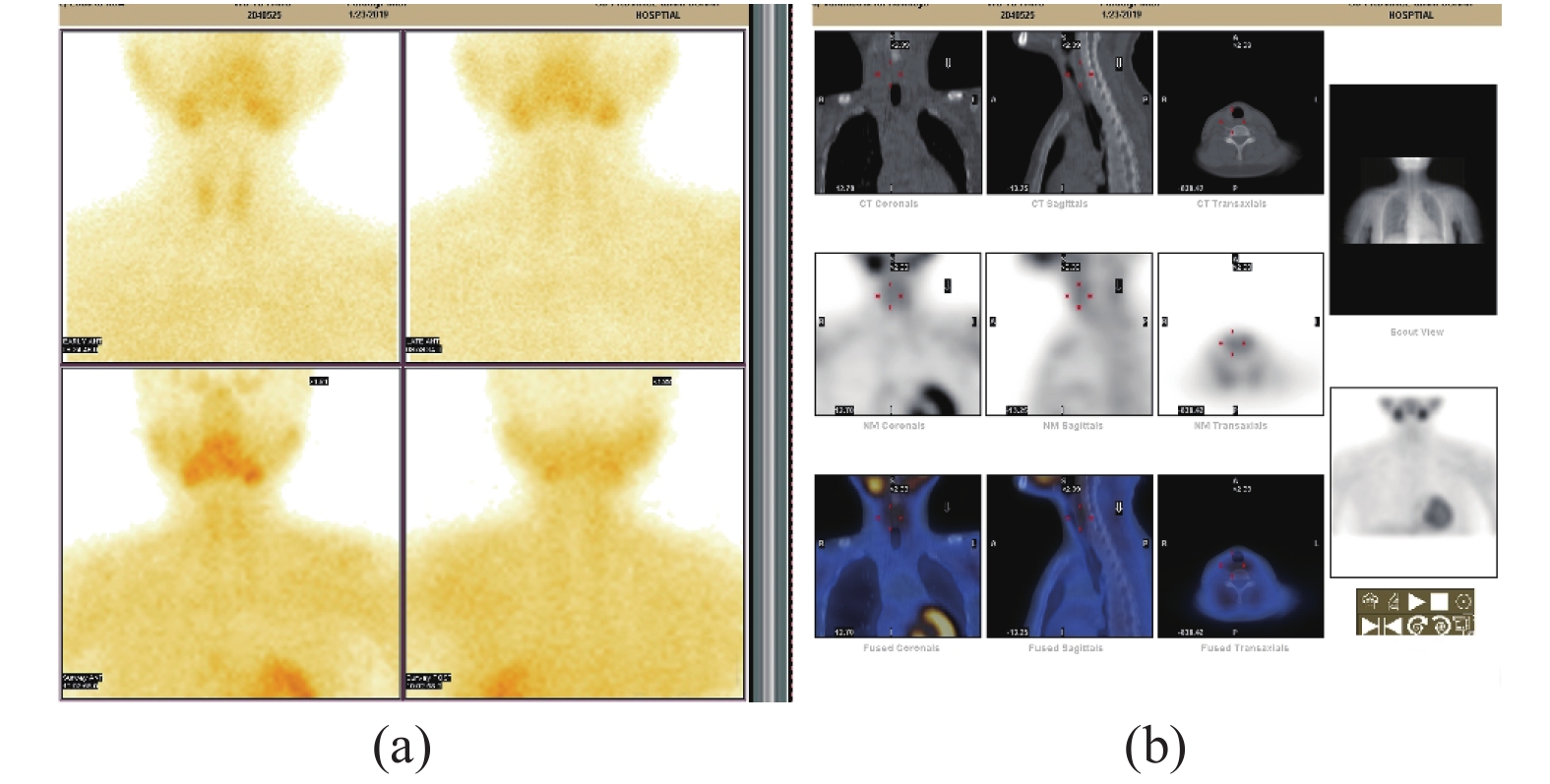
图 1 a 平面显像:早期及延迟相甲状腺两叶均未见放射性核素浓聚灶。b断层融合显像,甲状腺两叶均未见放射性核素浓聚灶,术后病理证实为甲状腺微小乳头状肿瘤 Figure 1 a:Planar imaging:In the early and delayed phase,no radionuclide concentration foci in both thyroid lobes. b:Tomographic fusion imaging:no radionuclide concentration foci in both thyroid lobes. Postoperative pathology confirmed thyroid micropapillary tumors. |
|
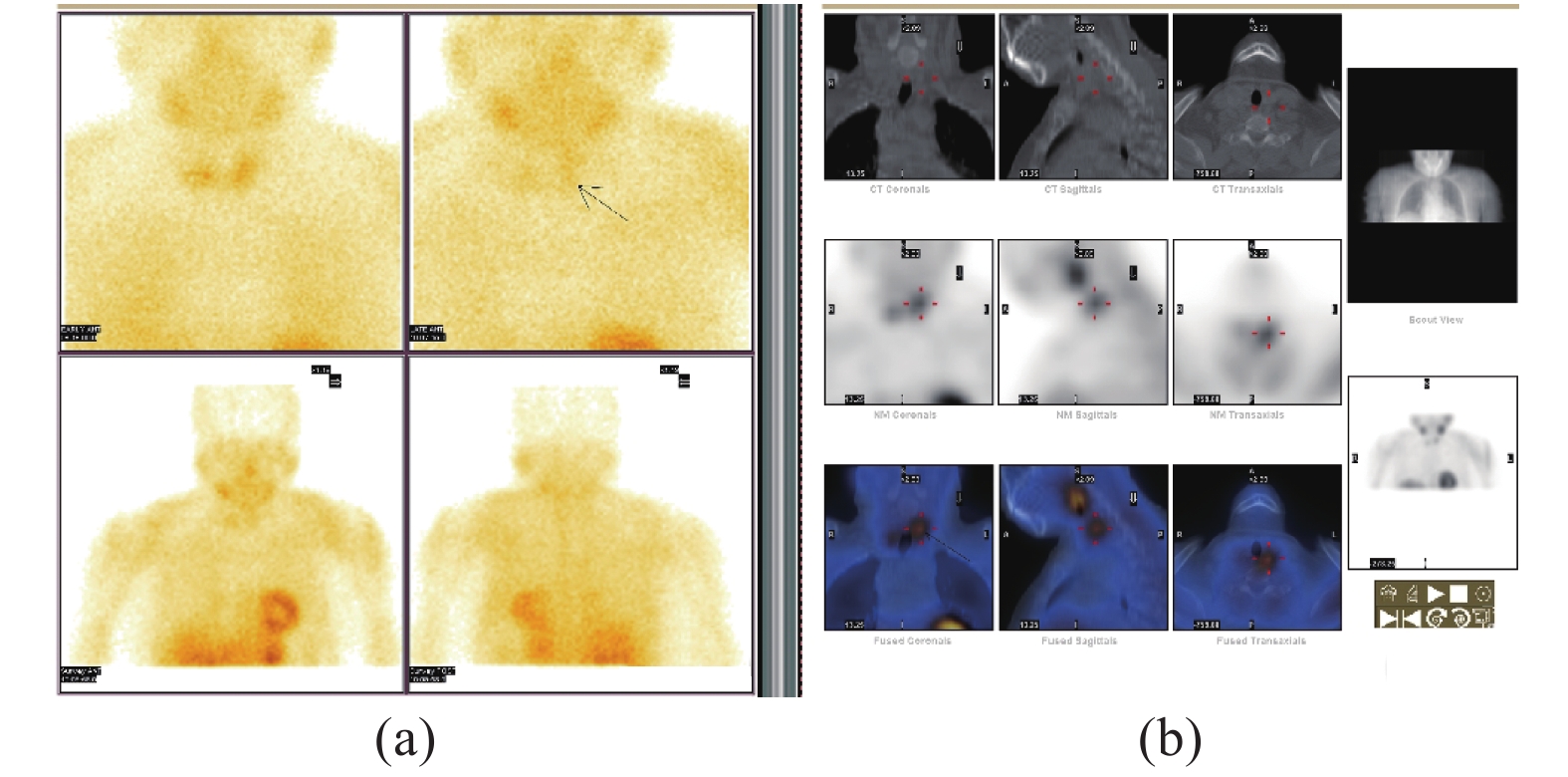
图 2 a 平面显像:早期及延迟相甲状腺左叶中上极放射性核素浓聚灶。b断层融合显像,可见甲状腺左叶中上极放射性核素浓聚灶,术后病理证实为左叶中上极甲状旁腺腺瘤。 Figure 2 a:Planar imaging:In the early and delayed phase,radionuclide concentration foci in the middle and upper pole of the left lobe of the thyroid gland. b:Tomographic fusion imaging:radionuclide concentration foci in the middle and upper pole of the left lobe of the thyroid gland. Postoperative pathology confirmed middle and upper pole of the left parathyroid adenoma. |
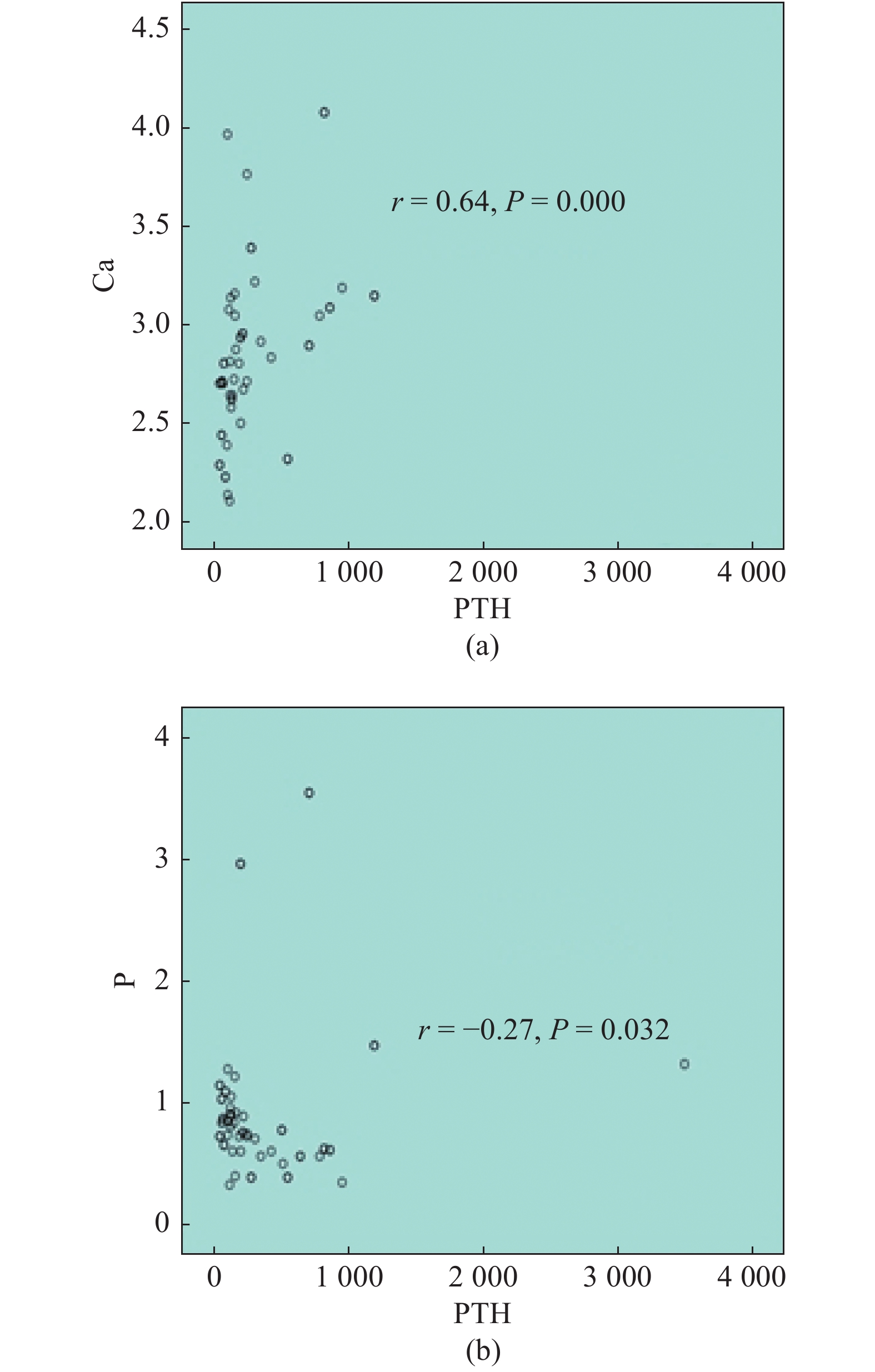
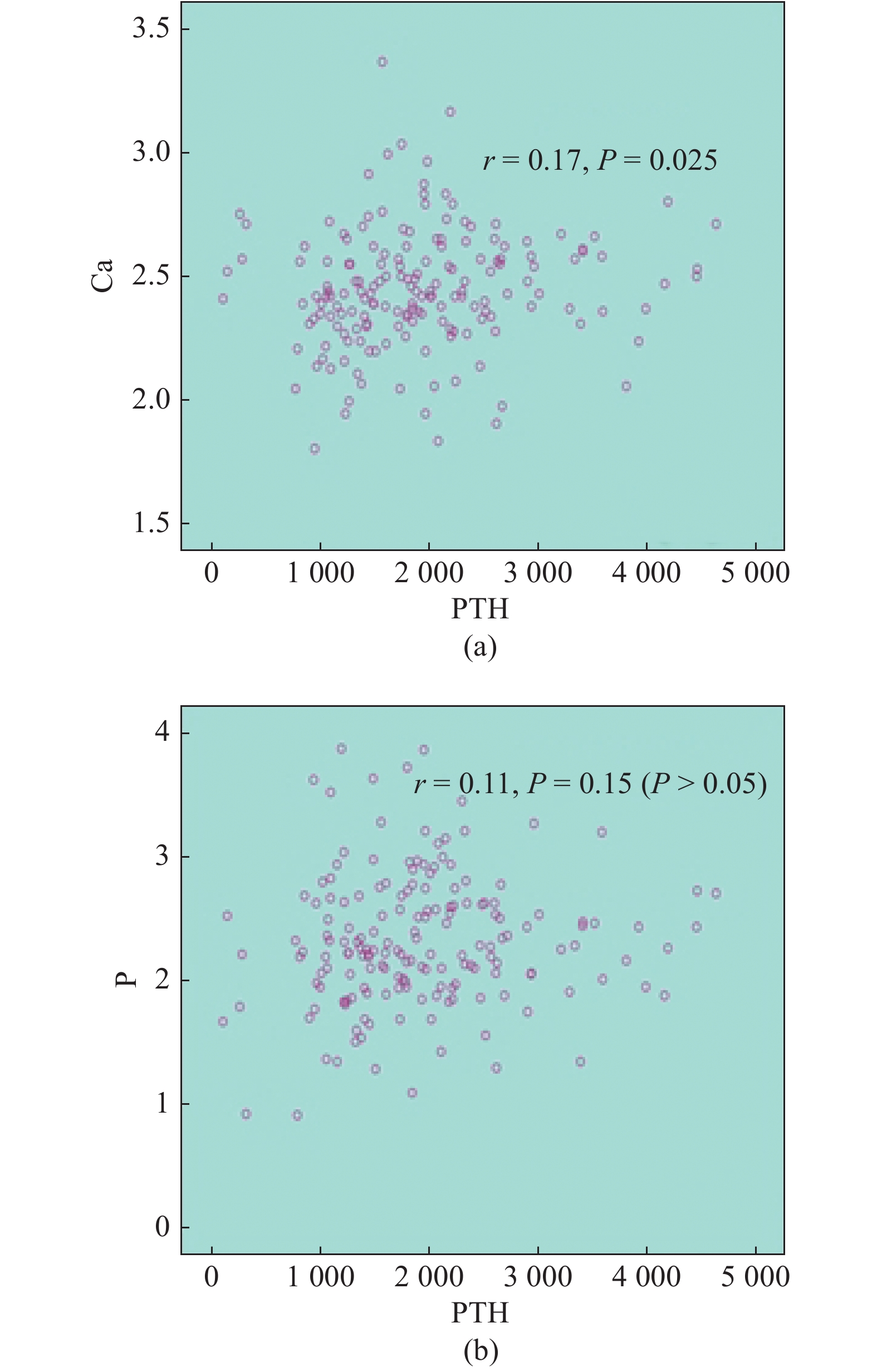
PHPT组中PTH与血清钙、磷的相关系数分别为r = 0.64和r = −0.27(图3);SHPT组中PTH与钙的相关系数r = 0.17,PTH与血清磷无相关性(图4)。
|
图 3 a 原发组血清钙水平与PTH的相关性b原发组血清磷水平与PTH的相关性 Figure 3 a: Correlation between serum calcium level and PTH in PHPT group. b: Correlation between serum phosphorus level and PTH in PHPT group |
|
图 4 a继发组血清钙水平与PTH的相关性b继发组血清磷水平与PTH的相关性 Figure 4 a:Correlation between serum calcium level and PTH in SHPTgroup. b: Correlation between serum phosphorus level and PTH in SHPT group |
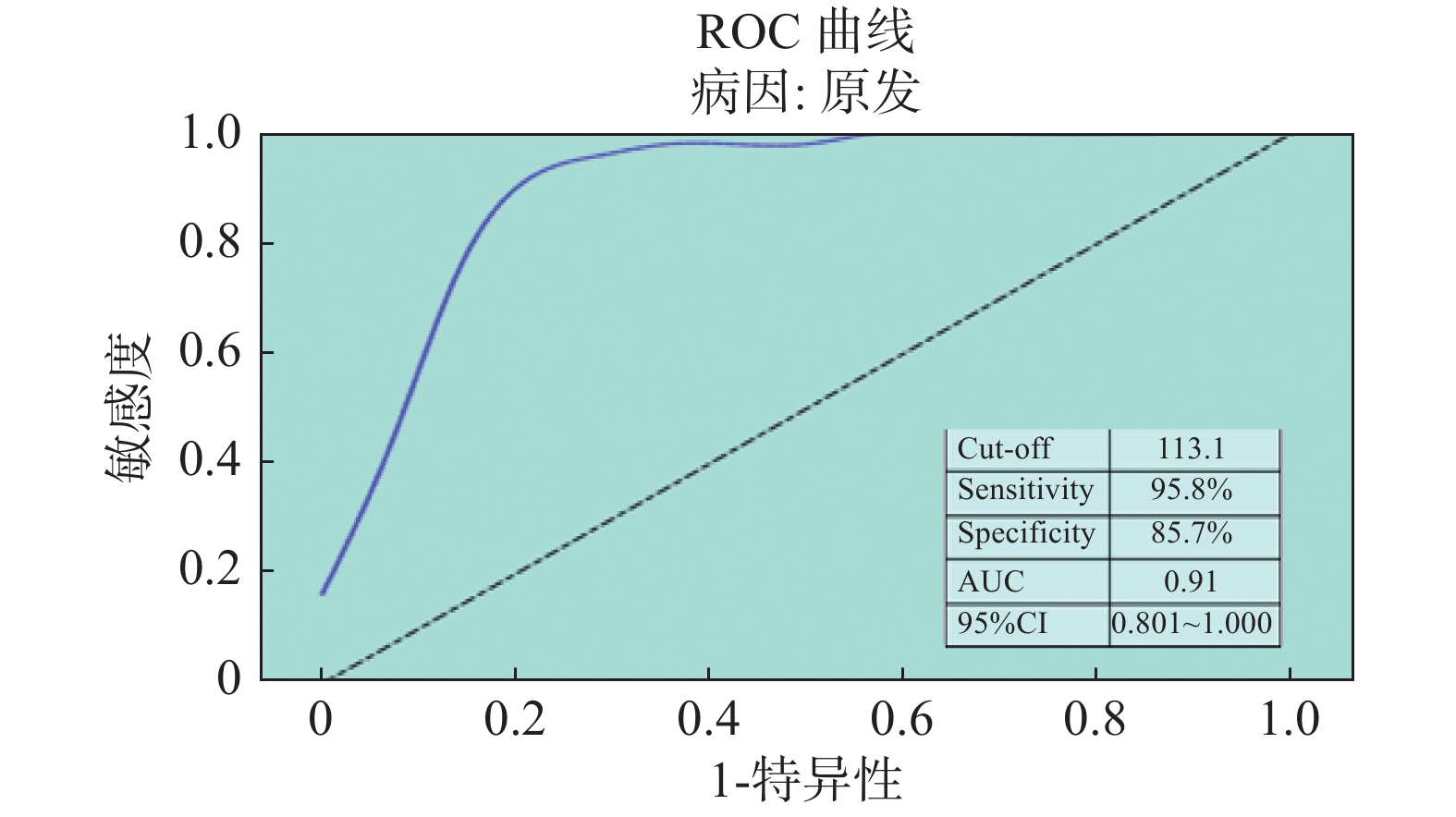
将年龄、性别、PTH值、钙值、磷值作为自变量,99Tcm-MIBI显像结果作为应变量行Logistic回归分析,PHPT组经筛选得出影响因素为PTH(OR:1.012,95%CI:1.002~1.023),行相关性分析,得出r = 0.60 (P = 0.000),SHPT组无相关因素。绘制PHPT组99Tcm-MIBI影像显像结果ROC曲线,对应最大曲线下面积0.91,计算Cutoff值为113.1 pg/mL (图5)。PHPT组血清PTH水平低于113.1 pg/mL:MIBI显像结果阴性12例,MIBI显像结果阳性2例;血清PTH水平高于113.1 pg/mL:MIBI显像结果阴性2例,MIBI显像结果阳性46例。
|
图 5 PHPT组的ROC曲线 Figure 5 ROC curve of PHPT group |
99Tcm-MIBI是一种脂溶性的放射性示踪剂,通过简单扩散聚集于血运丰富、代谢活跃及富含线粒体组织细胞内[2]。多药耐药相关蛋白和P-糖蛋白参与体内外源性和内源性化合物的清除,保护机体免受毒素侵害[3],而浓聚于线粒体的机制目前尚不清楚。在MIBI双时相显像中,与正常甲状腺相比,甲状旁腺细胞因线粒体含量多、P-糖蛋白表达少所以对MIBI高摄取、低洗脱[4]。
MIBI显像阳性结果与HPT生化参数、腺体体积大小和组织病理学的相关性,一直是研究分析的热点。国内外大量研究认为血清PTH水平与MIBI显像呈正相关,但也有部分研究认为两者间并无相关性。本研究发现血清PTH水平为PHPT组MIBI显像的影响因素,并且两者间呈中度正相关,而SHPT组未发现影响因素,分析其原因可能是本研究SHTP组病因均为慢性肾脏病,PTH水平受血清钙磷及骨化三醇等多种因素交互影响;PHPT组病因主要为甲状旁腺腺瘤,经研究表明,磷脂/钙依赖的胆碱激酶的上调已被证明与甲状旁腺激素的自主分泌有关[5]。2组中均有一部分患者PTH水平升高而MIBI显像阴性,分析其原因主要为:①病灶体积太小[6];②部分腺瘤内嗜酸性细胞占比多,对显像剂清除较快[7];③高功能甲状旁腺细胞内线粒体太少,其中腺瘤或增生甲状旁腺体积太小是最常见的原因。有研究证实,甲状旁腺病变体积大小是影响MIBI显像最主要的因素,血清PTH水平与病变腺体体积呈正相关(r = 0.782,P < 0.001) [8],Monzen等[9]报道SPECT/CT融合显像可以检出甲状旁腺腺瘤的最大直径为0.6 cm。
目前,尚未发现血清钙水平与MIBI显像结果之间具有直接正相关,可能是因为血清钙的变化范围很小,受骨化三醇和甲状旁腺激素共同调节,它们都会影响肠道钙吸收、骨形成和骨吸收以及尿钙排泄。本研究亦显示,SHPT组血清钙与PTH相关性明显低于PHPT组,考虑可能与服用钙剂、活性维生素D3及透析液钙浓度等多种因素有关[10]。
综上,本研究发现PHPT血清PTH水平与MIBI显像结果具有一定相关性而血清钙磷水平与MIBI显像无直接相关性;当PTH水平超过113.1 pg/mL时,MIBI显像阳性可能性更大,说明血清PTH水平对MIBI显像阳性具有重要预测价值。SHPT组MIBI显像阴性病例太少,后续将扩大样本量进一步研究。
| [1] |
Madeo B, De Vincentis S, Repaci A, et al. The calcium-to-phosphorous (Ca/P) ratio in the diagnosis of primary hyperparathyroidism and hypoparathyroidism: a multicentric study[J]. Endocrine, 2020, 68(3): 679-687. DOI:10.1007/s12020-020-02276-7 |
| [2] |
余会丽. 99Tcm-MIBI双时相显像联合血清PTH检测诊断原发性甲状旁腺功能亢进症的价值
[J]. 河南医学研究, 2020, 29(1): 146-147. Yu HL. The value of 99Tcm-MIBI dual-phase imaging combined with serum PTH detection in the diagnosis of primary hyperparathyroidism [J]. Henan Med Res, 2020, 29(1): 146-147. DOI:10.3969/j.issn.1004-437X.2020.01.075 |
| [3] |
Hendrikse NH, Kuipers F, Meijer C, et al. In vivo imaging of hepatobiliary transport function mediated by multidrug resistance associated protein and P-glycoprotein
[J]. Cancer Chemother Pharmacol, 2004, 54(2): 131-138. DOI:10.1007/s00280-004-0793-2 |
| [4] |
Robin P, Klein R, Gardner J, et al. Quantitative analysis of technetium-99m-sestamibi uptake and washout in parathyroid scintigraphy supports dual mechanisms of lesion conspicuity[J]. Nucl Med Commun, 2019, 40(5): 469-476. DOI:10.1097/mnm.0000000000000996 |
| [5] |
Ishizuka T, Kajita K, Kamikubo K, et al. Phospholipid/Ca2+-dependent protein kinase activity in human parathyroid adenoma
[J]. Endocrinol Jpn, 1987, 34(6): 965-968. DOI:10.1507/endocrj1954.34.965 |
| [6] |
李帝, 张琳, 邓大平. 99Tcm-MIBI SPECT/CT显像在原发性甲状旁腺功能亢进症诊断中的价值讨论
[J]. 中国辐射卫生, 2019, 28(2): 194-197. Li D, Zhang L, Deng DP. Discussion on the value of 99Tcm -MIBI single photon emission computed tomography/computerized tomography in the diagnosis of primary hyperparathyroidism [J]. Chin J Radiol Health, 2019, 28(2): 194-197. DOI:10.13491/j.issn.1004-714X.2019.02.022 |
| [7] |
Suh HY, Na HY, Park SY, et al. The usefulness of maximum standardized uptake value at the delayed phase of Tc-99m sestamibi single-photon emission computed tomography/computed tomography for identification of parathyroid adenoma and hyperplasia[J]. Medicine, 2020, 99(28): e21176. DOI:10.1097/md.0000000000021176 |
| [8] |
王静, 朱玉春, 蔡国强, 等. 甲状旁腺病灶重量对99Tcm-MIBI显像诊断灵敏度的影响
[J]. 国际放射医学核医学杂志, 2020, 44(6): 352-358. Wang J, Zhu YC, Cai GQ, et al. The influence of parathyroid lesion weight on diagnostic sensitivity of 99Tcm-MIBI imaging [J]. Int J Radiat Med Nucl Med, 2020, 44(6): 352-358. DOI:10.3760/cma.j.cn121381-201903012-00037 |
| [9] |
周建立, 王健, 朱富强. 甲状旁腺功能亢进症患者血清PTH水平与99Tcm-MIBI SPECT/CT双时相显像的相关性研究
[J]. 中国临床医学影像杂志, 2020, 31(3): 171-174. Zhou JL, Wang J, Zhu FQ. Correlation between serum PTH level and 99Tcm-MIBI SPECT/CT dual-phase imaging in patients with hyperparathyropathy [J]. J China Clin Med Imag, 2020, 31(3): 171-174. DOI:10.12117/jccmi.2020.03.006 |
| [10] |
卢元, 胡晓舟, 张瑾, 等. 维持性血液透析患者继发性甲状旁腺功能亢进相关因素分析[J]. 实用医学杂志, 2015, 31(16): 2684-2687. Lu Y, Hu XZ, Zhang J, et al. Analysis of related factors of secondary hyperparathyroidism in maintenance hemodialysis patients[J]. J Pract Med, 2015, 31(16): 2684-2687. DOI:10.3969/j.issn.1006-5725.2015.16.031 |




