·编者按· Lindell教授曾任ICRP主席, 现为荣誉主委, Dunster教授曾任ICRP主委, 现也为荣誉主委, Valentin教授现为ICRP主委员会科学秘书。他们三人联合撰写的下面这篇通讯, 是一篇难得的报告, 它对我们了解ICRP的历史、辐射防护概念、政策的演变以及现行政策的实施, 均有巨大的指导作用, 从而可进一步加深对我国新的辐射防护基本安全标准的理解和认识。希望广大读者认真耐心地阅读此文, 定会受益匪浅。
The International Commission on Radiological Protection (ICRP) recently issued a review of its history, mode of operation, concepts, and current policies[1]. The present paper summarises that report. It is assumed that the reader is broadly familiar with the current Recommendations and Publications of the Commission.
2 History and affiliationICRP was established in 1928 as a Commission linked to the International Congresses of Radiology. Formally, its parent organisation is still the International Society of Radiology, but its field of work has widened from protection in medical radiology to all aspects of protection against ionising radiation. The Commission is supported by a number of international organisations and by many governments. It issues recommendations on the principles of radiation protection. Its recommendations form the basis for more detailed codes and regulations issued by other international organisations and by regional and national authorities.
The Commission is registered as an independent charity in the United Kingdom and is financed mainly by voluntary contributions from international and national bodies with an interest in radiological protection. Some additional funds accrue from royalties on the Commission's publications. Members' institutions also provide financial support to the Commission by making the members' time available without charge and, in some cases, contributing to their costs of attending meetings. Many of these institutions also provide substantial resources without charge to the Commission.
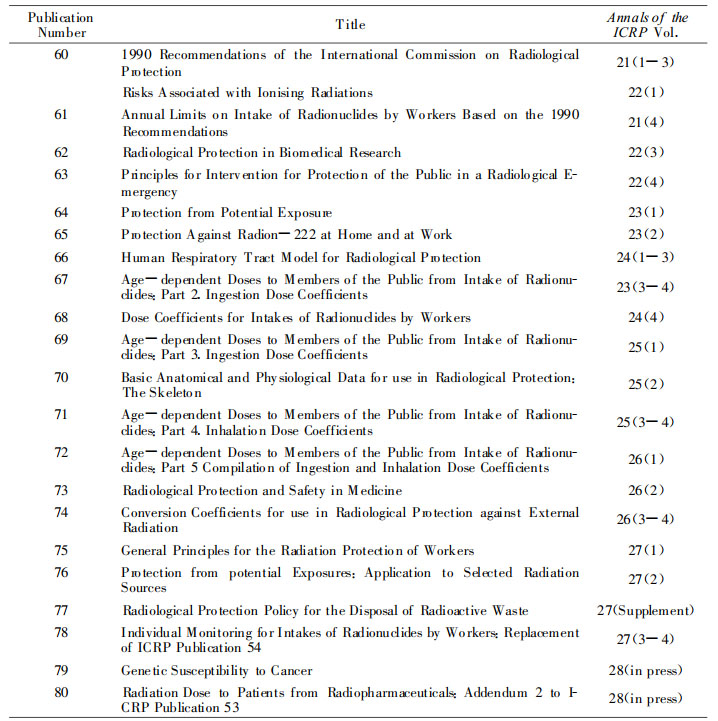
The Commission issued its first report in 1928. The first report in the current series, subsequently numbered Publication 1[2], contained recommendations adopted in September 1958. Subsequent general recommendations have appeared in 1964 as Publication 6[3], in 1966 as Publication 9[4], and in 1977 as Publication 26[5]. Publication 26 was amended and extended by a Statement in 1978[6] and further clarified and extended by a succession of Statements between 1980 and 1987[7, 8, 9, 10, 11]. The recommendations were completely revised and issued in 1991 as Publication 60[12]. Reports on more specialised topics have appeared as intermediate and subsequent Publication numbers. The more recent reports are listed in Table 1.
|
|
Table 1 Summary of ICRP Publications from Publication 60 Onwards |
The Commission has always been an advisory body. It offers its recommendations to regulatory and advisory agencies at international, regional, and national levels, mainly by providing guidance on the fundamental principles on which appropriate radiological protection can be based. The Commission does not aim to provide regulatory texts. Authorities need to develop their own texts in the context of their own regulatory structures. Nevertheless, the Commission believes that these regulatory texts should be developed from, and have aims that are broadly consistent with, its guidance. In addition, the Commission hopes that its advice is of help to management bodies with responsibilities for radiological protection in their own operations, to the professional staff whom they use as their advisers, and to individuals, such as radiologists, who have to make decisions about protection in the use of ionising radiation.
3 The Structure and Mode of Operation of the CommissionICRP is composed of a Main Commission and four standing Committees. The Commission consists of twelve members and a Chairman. They are elected by the Commission itself, under its rules, which are subject to the approval of the International Society of Radiology. The Committee members are appointed by the Commission, and each Committee is chaired by a Commission member. From 1962 to the present, 1998, there have been four Committees: Committee 1 on Radiation Effects, Committee 2 on Derived Limits, Committee 3 on Protection in Medicine, and Committee 4 on the Application of the Commission's Recommendations.
The Commission uses Task Groups and Working Parties to prepare reports to be discussed by the Committees and finally approved by the Commission. Task Groups are appointed by the Commission to perform a defined task, usually the preparation of a draft report. A Task Group usually contains a majority of specialists from outside the Commission's structure. Working Parties are set up by Committees, with the approval of the Commission, to develop ideas for the Committee, sometimes leading to a Task Group. The membership is usually limited to Committee members.
The Commission's secretariat is managed by a Scientific Secretary with a minimum of bureaucracy.
4 The Objectives of the Commission's RecommendationsThe main objective of the Commission's recommendations is to provide an appropriate standard of protection for man without unduly limiting the beneficial practices giving rise to radiation exposure.
This aim of providing an appropriate standard of protection, rather than the best possible standard regardless of costs and benefits, cannot be achieved on the basis of scientific concepts alone. Members of the Commission and its Committees have the responsibility for supplementing their scientific knowledge by value judgements about the relative importance of different kinds of risk and abothe balancing of risks and benefits. The Commission believes that the basis for such judgements should be made clear, so that readers can understand how the decisions have been reached.
5 QuantitiesThe absorbed dose is the radiation energy imparted per unit mass of an irradiated body. It is measured in joule per kilogram, a unit which is also called the gray (Gy). Multiplying the absorbed dose by appropriate weighting factors depending on the type of radiation, creates the equivalent dose in the relevant organ or tissue. By weighting the equivalent dose in each organ in proportion to the probability and severity of the harm done by radiation, and adding the weighted contributions from each organ to a total body dose, a third dose, the effective dose is obtained.
The effective dose is defined by the Commission as the sum of the equivalent doses in the principal tissues and organs in the body, each weighted by a tissue weighting factor, wT. This weighting factor takes account of the probability of fatal cancer, the probability of nonfatal cancer, weighted for severity, and the average length of life lost due to an induced cancer. A contribution for severe hereditary disorders is also included. Detriment, as used by the Commission, can be thought of as the probability of causing a level of total harm judged to be equivalent to one death that causes, on average, a loss of lifetime of 15 years. The committed effective dose is the sum of the committed equivalent doses each weighted by the appropriate tissue weighting factor.
In radiation protection it is usually the effective dose that is determined for comparison with dose limits or for assessments of risks. Both the equivalent dose and the effective dose are also measured in joule per kilogram, but in these cases the unit is called the sievert (Sv). For x rays and gamma rays the absorbed and equivalent doses in gray and sievert are numerically equal.
In publications before Publication 60, the Commission defined a mean quality factor, Q, for spectra of mixed values of linear energy transfer. In addition, the Commission stated that it was permissible to use approximate values for Q and provided tables of values[5]. In Publication 60[12], the Commission replaced the dose equivalent defined at a point by the equivalent dose, derived by weighting the mean absorbed dose in an organ or tissue by the radiation weighting factor, wR. This factor was an updated value of the previous permissible approximation for Q, but now became the definitive weighting factor.
Doses in organs within the body cannot be measured directly, so practical quantities, measurable outside the body, are needed. For radiation fields outside the body, measurable quantities, called operational quantities, have been recommended by the International Commission on Radiation Units and Measurements. These quantities were specified before the introduction of the radiation weighting factor, and use quality factors (related to linear energy transfer) rather than radiation weighting factors. Nevertheless, they still provide a set of field quantities that, in most practical situations, adequately reflect the protection quantities used by ICRP[13].
For sources inside the body, the relevant measurable quantity is the activity of radioactive material taken into the body, the intake. This material causes a continuing distribution of equivalent doses within the body. The time integral of the resulting equivalentdose rate is called the committed equivalent dose. The integration time is 50 years for an adult and from the time of intake to age 70 years for children.
In source-related assessments, the individual doses have to be supplemented by information on the number of people exposed. The simplest quantity to reflect both the dose and the number of people is the collective dose. The collective effective dose may sometimes be used as a measure of the expected collective harm, the radiation health detriment.
The collective dose is most useful when the individual doses are all of much the same magnitude and are all delivered in times not greatly exceeding a few years. If the distribution of individual doses covers many orders of magnitude and the time distribution covers centuries, the simple collective dose is less useful because it aggregates too much diverse information. It is then better to present partially disaggregated data in the form of blocks of collective dose each covering a narrower range of individual dose and a narrower range of time.
6 The Biological Basis of the Commission's PolicyThere are two types of harmful radiation effects to be protected against. High doses will cause inevitable harm, the deterministic effects, which do not appear if the dose does not exceed a threshold value. The primary protection policy is then to prevent high doses. Both low and high doses may cause stochastic, i.e. randomly occurring, effects (cancer and hereditary disorders). At low doses, of the order of those caused by natural sources of radiation, these effects will occur only with a small probability, which is judged by the Commission to be in proportion to the dose.
This proportionality (the linear, non-threshold dose-response relationship) has characteristics that facilitate the administration of radiation protection. For example, it makes it possible to consider each source and exposure separately from other sources and exposures-the probability of harm per unit dose will always be the same. However, the probabilistic nature of the stochastic effects makes it impossible to make a clear distinction between 'safe' and 'dangerous', a fact that causes problems in explaining the control of radiation risks.
The major policy implication of a non-threshold relationship for stochastic effects is that some finite risk must be accepted at any level of protection. Zero risk is not an option. This leads to the basic system of protection which has three components.
(1) the justification of a practice, which implies doing more good than harm,
(2) the optimisation of protection, which implies maximising the margin of good over harm, and
(3) the use of dose limits, which implies an adequate standard of protection even for the most highly exposed individuals.
A simple proportional relationship also has some important practical implications. It allows.
(a) doses within an organ or tissue of the body to be averaged over that organ or tissue,
(b) doses received at different times to be added, and
(c) doses received from one source to be considered independently of the doses received from other sources.
These practical aspects are of overwhelming importance in radiological protection because of the complexity of the dose distributions in both time and space and because of the ubiquitous presence of natural sources of radiation.
7 ConceptsThe Commission makes a distinction between what it calls practices and intervention. A practice is a human activity that is undertaken by choice but which increases the overall exposure. For that reason, practices have to be controlled so that additional doses are appropriately restricted. Intervention is an action against radiation exposures that already exist, for the purpose of reducing the exposures. Both practices and intervention are justified when they cause more good than harm.
The main protection principle in both cases is that protection should be optimised, i.e. all doses should be kept as low as reasonably achievable, economic and social factors being taken into account. For equity reasons (because those who are exposed are not necessarily those who gain by a practice) some dose or risk limitation is necessary to prevent the optimised situation from being one where a few individuals receive inappropriately high doses. In addition to source-related constraints for this purpose, various levels for actions are recommended (levels for intervention, for recording, for investigation, etc.).
The Commission also differentiates between three types of exposure: occupational exposure, which is the exposure incurred at work, and principally as a result of work; medical exposure, which is principally the exposure of persons as part of their diagnosis or treatment; and public exposure, which comprises all other exposures. A distinction is also drawn between source-related assessments, which are concerned with the exposures resulting from a single source and individual-related assessments, which deal with the exposure of a single individual from many sources.
The process of the optimisation of protection involves some degree of balancing of detriments and benefits. Unless the individual detriments are small, this process raises ethical problems of inequity when the detriments and benefits accrue to different people, as is usually the case. It is in order to limit this inequity that the Commission recommends the use of source-related constraints, aimed at excluding from the process of optimisation any protection options that would involve individual doses above the selected constraint.
Over the years there has been confusion over the meaning of the Commission's dose limits. The Commission now regards these as being close to the point where the doses from the sources to which the dose limits apply result in a level of risk that, if continued, could legitimately be described as unacceptable for those sources in normal circumstances. Compliance with dose limits is then a necessary, but not a sufficient, condition for complying with the Commission's recommendations. A dose limit is not a measure of the degree of rigour implied by the recommendations. That should be judged by the overall impact of the system of protection, of which the optimisation of protection is the most onerous and effective component. It must be remembered that dose limits do not apply to medical exposure.
Particular confusion has been caused by the dose limit for public exposure. This limit applies to the doses from (i.e. attributable to) deliberate practices and, within these practices, from those radiation sources that can reasonably be controlled by human actions. The value selected is less than the total dose from all sources, many of which are natural sources that cannot be controlled, e.g. the dose from natural potassium in the body or from cosmic rays at ground level. This position, while logical, is not easily explained. The presence of doses from natural sources of radiation does not justify the doses from controllable sources. It is proper to control these sources, even if the doses are less than the background doses from uncontrolled natural sources. However, this background does provide a useful basis for comparisons.
As with practices, the justification of intervention requires that the intervention should do more good than harm. Intervention is justified if the reduction of exposures and thus of radiation induced detriment is sufficient to offset the costs, risks, and social disadvantages of the actions (countermeasures) that comprise the intervention. The decision to intervene is made easier by the selection of intervention levels of averted dose linked to specified actions. The Commission has recommended ranges of such intervention levels[14, 15]
All these concepts relate to situations in which the dose has already occurred or will occur in the future. However, there are many situations in which an exposure (and thus a dose) is not certain to occur and may have only a small probability of occurring. Such exposures are called potential exposures. The detriment associated with a potential exposure of an individual can be expressed as the product of the conditional detriment, given that the dose has occurred, and the probability of the dose being delivered.
Even for an individual potential exposure, the aggregation implied by this product may be excessive. For example, an event with a high probability of causing a dose that, if incurred, would carry a low probability of death and an event with a low probability of causing a high dose carrying a certainty of death may have the same potential detriment as given by this product. But the two events may not be judged to be of equal importance.
Reference levels are values of measured quantities above which some specified action or decision should be taken. They include recording levels, above which a result should be recorded, lower values being ignored; investigation levels, above which the cause or the implications of the result should be examined; intervention levels (of dose averted by a defined remedial action), above which the remedial action should be considered; and, more generally, action levels above which some specified action should be taken. The use of these levels can avoid unnecessary or unproductive work and can help in the effective deployment of resources.
8 The Quantitative Basis for Risk EstimatesThe Commission bases its recommendations on risk estimates derived from several sources. Direct evidence on deterministic effects on humans is obtained from observations on individuals who have been exposed to high doses by accident or intentionally in radiotherapy. For stochastic effects no direct cause-effect relation can be observed and assessments on risks to humans must be based on epidemiological studies with statistical methods. Because these effects are no different from cancers and hereditary disorders from other causes, statistical limitations prevent significant observations at low doses. The epidemiological information therefore has to be supplemented by inference from radiobiological research on mechanisms for stochastic effects.
The information on which the Commission bases its quantitative estimates of the probability of stochastic effects comes primarily from epidemiological studies of human populations. However, cancer and hereditary disorders are common in man and the detection and quantification of small increases depends on two features of the study. One is the statistical power of the study, which relates to the size of the population studied and the level of risk to detect. As information is sought at lower and lower doses, the statistical power ceases to be adequate and no conclusions can be drawn about the presence or absence of effects. The other limitation of low-dose epidemiological studies is the inability to control for confounding factors, such as tobacco use, where slight differences between exposed and comparison groups can be much more significant than the anticipated radiation risk.
9 The Structure of the System of ProtectionBecause of the complexity of radiological protection and of the need to achieve a consistency across a wide range of applications, the Commission has established a formal System of Protection. The main aim of this system is to encourage a structured approach to protection.
The principal subdivisions in the system are summarised as follows:
· Practices that increase the exposure of people or the number of people exposed;
· Intervention that decreases the exposures from existing sources;
· Source related and individual related assessments;
· Classification of types of exposure into occupational exposure, medical exposure and public exposure;
· Justification of a practice, optimisation of protection, and dose limits;
· Justification of intervention and optimisation of the type and scale of intervention;
· Potential exposure and accident prevention;
· Emergency planning;
· Implementation of the recommendations by operating managements and regulators.
10 Problems of Interpretation and Application in ProtectionThe Commission's risk estimates are called 'nominal' because they relate to the continuous exposure of a nominal population of males and females with a typical age distribution. For populations with an age distribution very different from the nominal populations it may be desirable to use adjusted risk coefficients, but not to seek for different sets of radiation and tissue weighting factors because these would confuse the use of effective dose.
The borderline between practices and intervention is usually clear, but there are some difficult cases. The clearest differentiation is provided by the ability to choose whether to accept the sources and the consequent exposures. If that choice is still available, the exposure can usually be said to be due to a practice and steps to reduce doses are improvements to the practice, not intervention. If the choice does not exist because the sources and the exposures already exist, any action taken to reduce exposures is intervention. The decision to intervene is then made on the basis of the dose that can be averted.
In the early years of radiological protection, the limited control of exposures made it desirable to check for the occurrence of detectable effects in workers. Pre-employment and routine medical surveillance were integral parts of protection. In recent years, the medical needs have changed. As in any occupation, there is still a need for confirmation that workers are fit for their duties, but the normal level of radiation exposure is not now a factor that should influence the extent of the conventional occupational health surveillance. Exceeding a dose limit is an indication of a failure of managerial control but, unless the dose is much higher than the dose limit, does not call for medical action.
Some confusion has been caused by attempts to limit the definition of occupational exposure to annual doses above some value, often 1 mSv. This is not the Commission's intention. All exposures incurred at work are occupational, although the Commission intends that its recommendations on occupational exposure should apply only to those occupational exposures that can reasonably be regarded as the responsibility of the operating management. The decision to use individual monitoring or to require special training should be based on an assessment of the need, rather than on any estimates of current or future exposure.
Occupational exposures directly due to an accident can be limited only by the design of the plant and its protective features and by the provision of emergency procedures. Ideally, the aim should be to keep the doses within those permitted in normal conditions, but this may not always be possible in serious accidents.
In addition to the exposures resulting directly from the accident, there will be exposures of emergency teams during emergency and remedial action. The doses incurred are likely to be higher than in normal situations and should be treated separately from any normal doses. Emergencies involving significant exposures of emergency teams are rare, so some relaxation of the controls for normal situations can be permitted in serious accidents without lowering the long-term level of protection. This relaxation should not permit the exposures during the control of the accident and the immediate and urgent remedial work to give doses approaching thresholds of deterministic effects. Furthermore, life-saving actions can rarely be limited by dosimetric assessments. Once the emergency is under control, remedial work should be treated as part of the occupational exposure incurred in a practice.
11 The Need for Stability, Consistency, and ClarityThe Commission's recommendations are widely used by international and regional agencies, by national regulatory agencies, and by operating managements and their protection advisers. The time-scale on which these bodies can respond to a change in recommendations varies widely, but none of them welcomes frequent changes. The Commission recognises this and avoids making frequent changes in its principal recommendations. Intervals of not less than ten to fifteen years seem to be appropriate. There is also an expectation that the recommendations will be internally consistent. This is fairly straightforward in the principal recommendations but more difficult in the separate detailed guidance issued on specialised topics.
附中文摘要 这篇报告扼要地评述了国际放射防护委员会(ICRP)的历史、运作方式、概念和现行政策。它涉及到委员会建议书的目的, 采用的量, 委员会政策的生物学基础, 危险估计的定量学基础, 防护体系的结构, 有关该系统中解释和应用的某些问题, 以及委员会建议书所需具备的稳定性、一致性和清晰性。(陈兴安译)
| [1] |
IC RP. International Commission on Radiological Protection: History, Policies, Procedures[M]. Oxford: Elsevier Science Ltd, 1998.
|
| [2] |
ICRP (1959). Recommendations of the International Commission on Radiological Protection. ICRP Publication 1, Pergamon Press, Oxford. https://test.europepmc.org/abstract/MED/8684952
|
| [3] |
ICRP (1964). Recommendations of the International Commission on Radiological Protection. ICRP Publication 6, Pergamon Press, Oxford.
|
| [4] |
ICRP (1966). Recommendations of the International Commission on Radiological Protection. ICRP Publication 9, Pergamon Press, Oxford.
|
| [5] |
ICRP (1977). Recommendations of the International Commission on Radiological Protection. ICRP Publication 26, Annals of the ICRP 1(3), Pergamon Press, Oxford.
|
| [6] |
ICRP (1978). Statement from the 1978 Stockholm meeting. In: Annals of the ICRP 1(3), Pergamon Press, Oxford.
|
| [7] |
ICRP (1980). Statement from the 1980 Brighton meeting. In: Annals of the ICRP 4(3/4), Pergamon Press, Oxford.
|
| [8] |
ICRP (1984). Statement from the 1983 Washington meeting. In: Annals of the ICRP 4(3/4), Pergamon Press, Oxford.
|
| [9] |
ICRP (1985). Statement from the 1985 Paris meeting. In: Annals of the ICRP 15(3), Pergamon Press, Oxford.
|
| [10] |
ICRP (1987a). Statement from the 1987 Washington meeting. In: Annals of the ICRP 17(2/3), Pergamon Press, Oxford.
|
| [11] |
ICRP (1987b). Statement from the 1987 Como meeting. In: Annals of the ICRP 17(4), Pergamon Press, Oxford.
|
| [12] |
ICRP (1991a). 1990 Recommendations of the International Commission on Radiological Protection. ICRP Publication 60, Annals of the ICRP 21(1-3), Pergamon Press, Oxford.
|
| [13] |
ICRP (1995). Conversion Coefficients for use in Radiological Protection against External Radiation. ICRP Publication 74, Annals of the ICRP 26(3/4), Pergamon Press, Oxford.
|
| [14] |
ICRP (1991b). Principles for Intervention for Protection of the Public in a Radiological Emergency. ICRP Publication 63, Annals of the ICRP 22(4), Pergamon Press, Oxford.
|
| [15] |
ICRP (1993). Protection Against Radon-222 at Home and at Work. ICRP Publication 65, Annals of the ICRP 23(2), Pergamon Press, Oxford.
|