2. 郑州大学医学院, 河南 郑州 450052
2. College of Medicine, Zhengzhou University, Zhengzhou 450052, China
核质转运(nucleocytoplasmic transport, NCT) 作为真核细胞的基本生命活动之一, 对细胞生理和病理过程都至关重要。该过程与货物蛋白(cargo protein) 携带的出入核信号(nuclear export signal, NES; nuclear localization signal, NLS)、货物蛋白和核质转运受体的修饰、Ran蛋白、核孔蛋白等因素密切相关。核质转运异常会造成货物蛋白在细胞中发生错误定位从而破坏其正常生理功能, 进而引发各种疾病, 如神经退行性疾病、癌症和炎症等[1, 2]。目前, 全球有4 700多万人受到神经退行性疾病的影响, 随着人口老龄化形势的日益严峻, 这一数字还会增加。在常见的神经退行性疾病中, 肌萎缩脊髓侧索硬化症(amyotrophic lateral sclerosis, ALS)、前额颞叶痴呆(frontotemporal dementia, FTD)、亨廷顿舞蹈症(Huntington's disease, HD)、脊髓小脑共济失调(spinocerebellar ataxias, SCAs)、阿尔茨海默症(Alzheimer's disease, AD) 等疾病的致病机制都和核质转运异常直接相关[3-5]。本文在PubMed、Springer和EBSCO等数据库中进行了20年来关于核质转运与神经退行性疾病的文献检索, 综述了核质转运异常在神经退行性疾病发病机制中的作用, 揭示核质转运异常可能是神经退行性疾病的共同致病机制, 但具体调控机制并不相同, 从而为神经退行性疾病潜在治疗药物靶标提供依据。
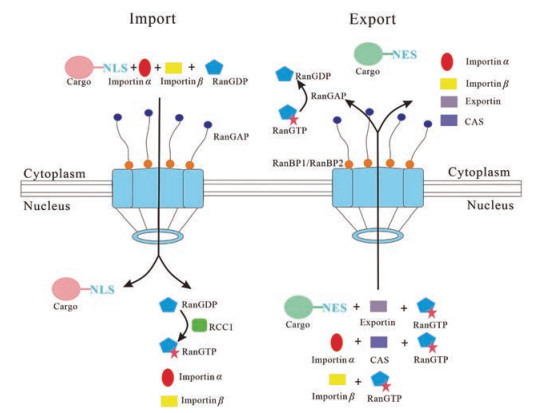
1 核质转运过程的生物学基础货物蛋白的核质转运需要穿过核膜(nuclear envelope, NE) 上具有分子筛功能的核孔复合体(nuclear pore complex, NPC)。NPC是一种大型蛋白复合物, 由30多种(500~1 000多个) 核孔蛋白(nucleoporins, Nups) 构成[6]。货物蛋白出入细胞核的方式主要有两种, 一种是分子量小于40~50 kDa的小分子物质以被动扩散的方式通过NPC; 而另外一种是分子量超过此范围或直径大于6 nm的生物大分子则需核质转运受体和RanGTP [Ran (ras-related nuclear protein) in complex with GTP] 介导的主动运输通过NPC[7-9]。货物蛋白出入细胞核的结构基础是自身的出入核信号(NES和NLS)。货物蛋白通过出入核信号与核质转运受体结合, 才能以货物-核质转运受体蛋白复合体的形式出入细胞核[10]。而核质转运受体在货物蛋白的核质转运过程中发挥了决定性的作用。Karyopherin是一类与核孔主动运输有关的核质转运受体蛋白家族, 包括importin α (karyopherin α, KPNA) 和importin β (karyopherin β, KPNB) 两个家族。Importin α能够识别经典NLS, 但没有穿梭功能, 需要由importin β携带入核。Importin α一端连接被运载的货物蛋白, 另一端连接importin β形成货物蛋白和importin α/β蛋白复合物, 再与RanGDP (Ran in complex with GDP) 结合, 识别和结合核孔蛋白后, 进入细胞核。随后, 在细胞核内的染色体浓缩调节因子[regulator of chromosome condensation 1, RCC1; 或称Ran鸟苷酸交换因子, guanine nucleotide exchange factor (GEF) for Ran, RanGEF] 的作用下, RanGDP转换成RanGTP (Ran in complex with GTP), 使得importin α和货物蛋白分别从蛋白复合物中解离, 完成货物蛋白的入核, 这个过程称之为importin α/β经典入核途径。进入细胞核的importin α在输出蛋白细胞凋亡敏感性蛋白(cellular apoptosis susceptibility, CAS) 的协助下返回胞浆[11]。Importin β具有穿梭核膜的功能, 除了结合importin α外, 还可结合非经典NLS (比如脯氨酸-酪氨酸NLS, PY-NLS) 或NES。Importin β和RanGTP结合返回细胞质进入下一轮运输。在Ran GTPase激活蛋白(Ran GTPase activating protein, RanGAP) 和核孔蛋白(Ran binding protein 1/2, RanBP1/2) 的帮助下, 使进入细胞质的RanGTP水解转换成RanGDP[12], 进入下一轮的运输(图 1)。以下将分别从不同类型的神经退行性疾病出发, 阐述核质转运异常对这类疾病致病机制的影响。
|
Figure 1 Classic nucleocytoplasmic transport mechanisms. Left: Importin α/β mediated import; Right: Export. In the presence of RanGTP, exportins bind NES containing protein as cargo or importin α into the cytoplasm. NLS: Nuclear localization signal; NES: Nuclear export signal; RanGDP: Ran in complex with GDP; RanGTP: Ran in complex with GTP; RCC1: Regulator of chromosome condensation 1; CAS: Cellular apoptosis susceptibility; RanGAP: Ran GTPase activating protein; RanBP1/2: Ran binding protein 1/2 |
ALS是一种进行性运动功能丧失的致死性神经退行性疾病[13, 14]。目前, 越来越多的证据表明ALS与另外一种表现为言语障碍及行为异常的神经退行性疾病FTD在临床表现、病理机制及基因遗传上有很多关联[15-17]。ALS和FTD共同的发病基因主要有第9号染色体开放阅读框72基因(chromosome 9 open reading frame 72, C9orf72) 和UBQLN2, 其中C9orf72基因突变的发病率更高, 高达80%左右, 而RNA结合蛋白TDP-43 (TAR DNA-binding protein 43) 和RNA结合蛋白FUS (fused in sarcoma) 是ALS和FTD病理学包涵体的主要组成成分[18]。下文将分别从共同发病基因C9orf72以及共同包涵体组成成分TDP-43和FUS三个方面阐述ALS/FTD疾病的核质转运异常。
2.1 C9orf72基因对ALS/FTD疾病核质转运的影响位于9号染色体开放阅读框72基因(C9orf72) 非编码区的GGGGCC (G4C2) 六核苷酸重复序列(hexanucleotide repeat expansion, HRE) 异常扩增被认为是导致遗传性ALS及FTD的重要致病因素[16]。在C9orf72突变的ALS/FTD果蝇模型中发现, 细胞核膜结构遭到破坏, 导致RNA在核内异常聚集[19]。HRE RNA具有神经毒性, 抑制正常的入核转运(import) 却增强出核功能(export)[20]。在表达HRE的果蝇模型、C9orf72 ALS患者诱导性多能干细胞和患者组织中均发现, RanGAP蛋白(人类RanGAP1蛋白) 高度亲和HRE RNA, 调控RanGTP在细胞核的浓度, 进而影响核质转运过程, 而过表达RanGAP蛋白能够有效抑制C9orf72 HRE诱发的细胞毒性[20]。另有研究表明, RanGEF (又称RCC1, 和RanGAP蛋白作用相反) 的核质分布浓度在C9orf72 ALS/FTD患者的成纤维细胞中受到影响[21], 这一结果在果蝇模型中也得到了验证[22]。同样, 敲低RanGEF蛋白能够拯救C9orf72 HRE诱发的神经退行性症状。在偶发性的FTD和C9orf72 ALS/FTD患者组织中, importin α (KPNA4) 异常聚集在细胞质, 并且表达量下调[23], 而过表达入核蛋白importin α或敲低出核蛋白exportin或改造出入核信号均能改善神经退行性症状[20]。
研究表明, 核孔复合物NPC的结构蛋白NUP50和NUP153功能丧失能够增加果蝇的神经退行性症状, 但NUP107、NUP160和NUP98-96功能缺失后抑制果蝇的神经退行性症状, mRNA出核复合物TREX (transcription-export) 中的成分REF1 (RNA and export factor binding protein 1) 功能缺失后也能够部分缓解神经退行性症状[24]。编码核孔复合物NPC结构蛋白的GLE1基因在ALS患者细胞内发生突变, 影响mRNA出核[24-26], 而且该基因在HD疾病中也被报道影响核质转运[27]。在ALS和FTD疾病模型中, RanGAP1、NUP205和NUP107等核孔蛋白也发生了异位[16, 28-30], 这说明核孔蛋白对于货物蛋白的出入核至关重要。另有研究表明, HRE RNA影响跨膜核孔蛋白POM121 (nuclear pore membrane protein 121) 在核内的表达, 进而影响NUP133、NUP107和NUP50等其他核孔蛋白表达水平, 从而改变核转运通路导致细胞死亡[31]。
HRE虽然插入到了C9orf72中的内含子中, 但是正义链和反义链都可作为模板翻译, 形成poly-GA (甘氨酸-丙氨酸)、poly-GR (甘氨酸-精氨酸)、poly-GP (甘氨酸-脯氨酸)、poly-PR (脯氨酸-精氨酸) 和poly-PA (脯氨酸-丙氨酸) 5种二肽重复蛋白(dipeptide repeat proteins, DPRs), 而这些不同多肽重复会结合包括Nup54和Nup98的核孔蛋白, 改变Ran GTPase细胞定位, 从而导致核质运输障碍[20, 32-38]。在表达GR和PR重复二肽的C9orf72 ALS模型中会形成应激颗粒(stress granules, SGs), 14种不同的Nups都会错误定位在SGs中, 从而破坏核质转运, 通过使用药物或者遗传操控可以减少SGs, 拯救核质转运的功能[39, 40]。最近研究表明, poly-GR和poly-PR可能通过应激等机制间接影响核质转运过程[41]。
综上所述, 在C9orf72 ALS/FTD动物模型和患者来源的神经细胞中, 核质运输障碍是细胞毒性的关键驱动力, 是ALS/FTD疾病发生和发展的重要原因。另外, 转运蛋白功能可能依赖于不同的细胞类型, 而神经细胞可能对核转运缺陷更敏感。有意思的是, 核转运蛋白还具有其他功能如蛋白伴侣作用, 能够减轻C9orf72诱发的毒性作用或在FUS和TDP-43形成的聚集体中发挥作用。
2.2 TDP-43蛋白的异常定位对ALS/FTD疾病的影响TDP-43蛋白是一种泛素化表达的多功能DNA和RNA结合蛋白, 由TARDBP基因编码, 大小为43 kDa, 在健康人群细胞内主要分布在细胞核, 在ALS和FTD患者中异常分布于细胞质并形成聚集体[42]。TDP-43蛋白在细胞质的异常聚集是导致95% ALS和45% FTD患者的主要原因[43-45]。而实际上, TDP-43胞质异常定位和聚集体的形成也是其他神经退行性疾病包括HD、AD和帕金森病(Parkinson's disease, PD) 的典型特征, 表明核质转运异常是这类疾病的共有特征[46-52]。
TDP-43含有一条经典的富含精氨酸、赖氨酸的NLS (classic NLS, cNLS) 信号, 其入核过程主要由异二聚体importin α1/β1介导[53, 54]。在ALS或额颞叶变性(frontotemporal lobe degeneration, FTLD) 患者中, TDP-43的cNLS虽然没有发生突变, 但是该入核信号缺失后会导致SGs的形成[55, 56], 这说明NLS在TDP-43入核和SGs形成过程中起到了重要作用。研究表明, 下调转运因子CAS和核质转运受体karyopherin β1后, 能够引起TDP-43在细胞质的异常聚集。此外, TDP-43和KPNA相互作用, 但仅下调单个的karyopherin α并不影响TDP-43的核转运, 这表明TDP-43是通过经典NLS进入细胞核, 且多个karyopherin α共同发挥作用。TDP-43包含一条富含亮氨酸的NES但不依赖exportin 1 (XPO1, 也被称作chromosomal maintenance 1, CRM1) 途径出核[57]。研究表明, 采用XPO1出核抑制剂[选择性核输出抑制剂(selective inhibitor of nuclear export, SINE)] 能够适度延长ALS/FTD模型中神经细胞的存活时间, 并减轻ALS大鼠模型的运动症状, 但对TDP-43核内水平影响不大, 而过表达出核蛋白比如XPO1、XPO7、NXF1 (nuclear RNA export factor 1) 都能够促使TDP-43出核, 这说明并不是某一单独出核蛋白调控TDP-43核转运, 而是多个蛋白联合作用或者也可能是以被动转运为主[58, 59]。TDP-43在细胞质异常聚集会募集importin α和Nup62等多种核转运受体和核孔蛋白, 造成RanGAP1、Ran、Nup107、importin α1、importin α3等蛋白的异常定位, 导致KPNA在细胞核内的耗竭, 从而引起TDP-43和KPNAs定位失调和功能异常的恶性循环, 进而造成细胞死亡[49, 60-62], 这在C9orf72 ALS/FTD和偶发性FTD脑组织中也有发现[22]。在FTLD-TDP患者脑组织中发现, 和正常组相比, CAS和karyopherin α2 (KPNA2) 表达量降低, 说明TDP-43的细胞质异常聚集还可能和CAS和KPNA2的减少有关[53]。在C9orf72 ALS/FTD果蝇模型中, G4C2或DPRs积累会引起TDP-43的胞质错位和聚集[61]。最新研究表明, TDP-43细胞定位可能还和第136赖氨酸的类泛素蛋白修饰SUMO (small ubiquitin-like modifier) 有关, 提示致病蛋白的蛋白后修饰在核定位过程中也起到了一定的作用[63]。
2.3 FUS蛋白的异常定位对ALS/FTD疾病的影响FUS是一种与TDP-43类似的RNA结合蛋白, 大小为53 kDa, 属于核蛋白, 其突变会导致ALS和FTD的发生[64]。大约一半的ALS和FTD的FUS突变都发生在NLS区域, 从而破坏FUS正常的细胞核定位和胞质聚集体的形成[65], 这表明核质转运异常是导致疾病发生或发展的主要原因。FUS的入核过程是通过transportin-1 (TNPO1)/karyopherin β2 (KPNB2) 识别其自身的脯氨酸酪氨酸入核信号(PY-NLS) 进行的[64-68]。FUS-NLS发生突变、TNPO1结合能力减弱以及FUS入核减少均具有致病性, 可导致ALS早期发作和疾病的快速发展[64, 69, 70]。有证据表明, ALS和FTD患者的入核蛋白包括importin β1和importin β2在大脑和脊髓中均发生异常表达和定位[53, 66, 67]。在神经细胞模型和转染的人类细胞模型中, 下调或抑制TNPO1均能导致FUS的异常定位, 从而被募集到SGs中[64]。此外, 在FTD-FUS患者中FUS双甲基化缺失, 取而代之的是无或单甲基化[65], 另外, FUS PY-NLS发生突变, 都会破坏FUS和TNPO1的结合, 从而抑制核质转运过程[69-72]。研究表明, FUS蛋白C端酪氨酸残基526的磷酸化能够改变TNPO1和FUS的相互作用, 从而影响FUS入核过程[73]。此外, 鉴于importin β型核输入受体还有蛋白伴侣的作用, TNPO1不仅介导FUS的入核, 而且可抑制FUS液相和SGs的形成[65]。XPO1是否负责FUS的出核还存在争议, 但是下调XPO1或Nup154 (与人类Nup155同源) 的表达水平可以减少FUS形成的胞质SGs和FUS诱发的细胞毒性[59, 74]。最近的研究表明, 和TDP-43一样, FUS也有2条XPO1介导的出核信号, 但并没有发挥作用, 而且出核过程不依赖于XPO1、RNA结合和mRNA出核过程, 这说明FUS的出核也可能依赖于被动运输[63]。
3 HDHD是一种多聚谷氨酰胺(polyglutamine, polyQ) 疾病, 主要症状包括以舞蹈症为特征的运动障碍、认知功能受损及精神行为异常。亨廷顿基因(huntingtin, htt, IT15) 1号外显子存在的高度多态CAG重复序列异常扩增是导致亨廷顿舞蹈病发生的原因, 该基因编码含多聚谷氨酰胺htt蛋白在细胞核内聚集是HD的典型症状[75]。目前, 关于htt蛋白核质转运的研究主要集中在以下3个方面:
3.1 出入核信号对于htt蛋白核质转运的影响Htt包含2条importin β2依赖的PY-NLS (典型特征是含有R-X5-PY基团, 下游8~15个氨基酸包括疏水基团或碱性基团, 两条信号氨基酸位点分别为174~207和1 182~1 190) 和1条富含亮氨酸的CRM1/exportin依赖的出核信号HIV-1 Rev-like NESs (LX2-3LX2-3LXL)[75-77]。研究表明, htt蛋白N端前17位氨基酸(N17), 作为经典的富含亮氨酸和疏水基团的出核信号, 调控htt蛋白的聚集体和毒性, 将出核信号保守序列突变后, 可增加htt的核内聚集[78-81]。在HD小鼠模型中, htt蛋白N端第13位和第16位(Ser-13和Ser-16) 丝氨酸位点磷酸化能够抑制全长htt蛋白的毒性和多肽片段诱发的聚集体[82], 这可能是Ser-13和Ser-16磷酸化水平与htt的细胞定位有关[83-85]。与该研究不同的是, 在HD的非神经细胞HEK293模型和原代小鼠皮质神经细胞模型中, 突变第4、7和14位亮氨酸和第11位苯丙氨酸均能促进htt入核和聚集体的形成, 但突变Ser-13和Ser-16后(包括拟磷酸化突变成天冬氨酸和抗磷酸化突变成丙氨酸) 均未有显著改变[79]。这可能是由于丝氨酸磷酸化受IκB激酶(inhibitor of nuclear factor kappa-B kinase, IKK) 和酪蛋白激酶(casein kinase 2, CK2) 调控, 而这些酶的有效性和选择性太差而不能作为有效的磷酸化方法。大多数研究采用SD (丝氨酸突变成天冬氨酸) 和SA (丝氨酸突变成丙氨酸) 方法用来模拟磷酸化和去磷酸化, 而不同的细胞和动物模型的实验背景以及表达条件的不同, 容易导致实验结果的差异。利用合成蛋白质模拟真实状态的磷酸化过程可以避免此类问题, 研究表明半合成的单或双磷酸化Ser-13和Ser-16位点的htt [正常htt和致病蛋白htt (mutant htt, mhtt)] 均能够抑制聚集体的形成, 同时促进mhtt进入细胞核[86]。
3.2 核质转运受体和核孔蛋白对htt核质转运的调控研究表明, htt入核受到importin β和TNPO1核转运受体的调控, 出核受到出核蛋白1 (exportin 1) 和抑制剂leptomycin B的影响[76]。突变htt能够引起核质运输一般性损伤[27, 87]。在不同的HD模型中, 包括果蝇、小鼠、诱导性多能干细胞(induced pluripotent stem cells, iPSC) 和患者组织, 都检测到核孔复合物NPC的病理现象, 如Nup62、Nup88、GLE1以及RanGAP1的异常定位和聚集, 从而导致核内Ran蛋白梯度降低, 改变核质蛋白的分布[87]。过表达Nups蛋白或采用小分子药物能够抑制突变htt和重复序列相关非ATG依赖的翻译产物(repeat associated non-ATG translation, RAN) 的毒性, 而过表达Ran或RanGAP1均能够减弱核质转运损伤[87], 起到神经保护作用。此外, RanGAP1和核蛋白Sec13更倾向于结合突变htt, 而入核蛋白受体importin β1、importin 4、importin 7和importin 9则结合野生型htt[27, 88-91]。研究表明, htt出核能力降低可能是导致核内聚集体形成的主要因素, htt蛋白的N端片段通过结合XPO1、核孔蛋白TPR进行核质转运, 而含多聚谷氨酰胺异常扩增的htt会破坏二者的相互作用和破坏核膜结构, 从而减少htt的出核和增加核内聚集[27, 92, 93]。
3.3 其他因素对htt核质转运的作用最近研究表明, 和C9orf72 ALS/FTD的六核苷酸重复序列一样, HD的CAG重复序列扩增也会产生4种其他重复多肽(polyAla、polySer、polyLeu和polyCys), 这些正反义链对神经细胞具有毒性作用[27, 94]。研究发现, RAN影响原代神经元的蛋白入核过程, 但具体机制并不明确[19, 94]。另有研究表明, HD脑中的胆固醇稳态受到破坏, 导致胆固醇和脂肪形成过程涉及的相关基因下调, 如固醇调节元件结合蛋白1和2 (SREBP1和SREBP2)。SREBPs是由无活性的内质网定位的前体合成的, 其成熟形式(mSREBPs) 是在SREBP前体转运到高尔基体经过蛋白水解产生的, 并与importin β结合而迅速导入核中。在HD小鼠模型的神经细胞以及HD患者细胞中, mSREBPs异常定位在细胞质。研究发现, 突变htt结合SREBP2/importin β复合体, 使之隔离在细胞质中[95]。最近在酵母模型系统中的全基因组筛选结果表明, 涉及神经变性的核糖体相关质量控制(RQC) 机制是Httex1-103Q核质分布的关键决定因素, RQC复合物的基因缺失会造成Httex1-103Q的核内聚集[96]。
4 SCAsSCAs是一组以常染色体显性遗传为特征, 临床表现以共济失调为主的神经系统遗传变性病。作为SCAs最常见的一种亚型, 脊髓小脑共济失调3型/马查多约瑟夫病(spinocerebellar ataxia type 3/Machado-Joseph disease, SCA3/MJD, 简称SCA3) 在我国SCAs人群中占比高达63%[97, 98], 也是一种多聚谷氨酰胺疾病。本文以SCA3为例, 揭示核质转运缺陷在SCAs致病机制中的影响。
SCA3其致病基因ATXN3编码的ataxin-3蛋白是含有多聚谷氨酰胺(polyQ) 的胞浆蛋白, 一般情况下, 健康人群polyQ重复序列数目在12~43之间, SCA3患者会增加至51~91之间[99]。而含有异常扩展polyQ的ataxin-3蛋白在各种致病因素的刺激下进入细胞核, 在核内募集其他多种组分包括转录因子、泛素蛋白酶、伴侣蛋白或RNA等形成核内包涵体(这是SCA3最重要的标志性病理特征), 从而导致核内转录异常、蛋白稳态失衡、能量代谢障碍、运输障碍等, 最终引起细胞凋亡[100-102]。因此, ataxin-3核质转运是SCA3最早期的病理变化, 是导致核内蛋白包涵体的形成、转录功能异常等致病过程中的关键因素。对于ataxin-3蛋白核质转运异常的相关研究, 最早是由德国Riess教授和美国Bonini教授的研究团队[103, 104]在1998年分别提出来的。在随后的20多年里, 大量证据表明, ataxin-3蛋白在核内异常定位, 会募集其他组分并诱发核内包涵体的形成, 导致核内正常生理功能失调[105], 该过程主要受到出入核信号、ataxin-3蛋白修饰和核质转运受体等因素的调控。目前关于ataxin-3蛋白核质转运的研究主要集中在以下3个方面:
4.1 出入核信号对于ataxin-3蛋白核质转运的影响目前, 已经鉴定出2条出核信号NES77、NES141和1条入核信号NLS273调控ataxin-3蛋白的出核和入核[106], 分别位于N端Josephin结构域(Josephin domain, JD) 和C端polyQ序列区(图 2)。

|
Figure 2 Schematic representation of ataxin-3 protein structure. Ataxin-3 consists of a globular N-terminal domain named Josephin domain (JD) with two nuclear export signals (NES) inside, followed by two Ub-interacting motifs (UIMs), a nuclear localization signal (NLS), and a flexible C-terminal tail with the polyglutamines tract. The third UIM only exists one alternative splice variant of ataxin-3 |
Ataxin-3的出核信号NES77 (IQVISNALKV) 是一段疏水序列, 符合Yx2–3Yx2–3YxY [其中Y代表Leu (L)、Ile (I)、Val (V)、Phe (F) 或者Met (M), x代表任意氨基酸] 富含亮氨酸典型出核信号的序列特征, 但只含1个亮氨酸。另外一个出核信号NES141 (ELISDTYLALFLAQLQQE) 包含5个亮氨酸, 但不符合富含亮氨酸典型出核信号的序列特征。出核转运受体CRM1主要结合富含亮氨酸和疏水基的出核信号, 而CRM1是否参与ataxin-3出核还存在争议, 可能还取决于ataxin-3蛋白N端的Josephin区域和泛素结合区[107], 最新研究表明, Ran蛋白在CRM1介导的出核过程中可能起重要作用[108]。Ataxin-3入核信号NLS273 (GTNLTSEELRKRRE) 是典型的含有连续的单簇碱性氨基酸R或K的入核信号序列, 而阻断该信号能够抑制ataxin-3进入细胞核。研究发现, 在SCA3小鼠模型中, 将外源的NLS连接到ataxin-3蛋白上(使更多的ataxin-3进入细胞核), 能够增加“有毒”包涵体的形成, 加重小鼠的疾病症状; 相反, 将NES融合到ataxin-3蛋白上(使更多的ataxin-3保留在细胞质内), 则有效地减少“有毒”包涵体的形成, 减轻小鼠的疾病症状[109]。
4.2 Ataxin-3蛋白修饰和所处的微环境决定其核质转运研究表明, 去泛素化、磷酸化和蛋白酶切割等修饰以及热应激、氧化应激等微环境决定ataxin-3蛋白的核质转运。根据Todi等[110]的报道, 突变ataxin-3蛋白JD区域的去泛素化酶活性位点第14位半胱氨酸(C14), 使ataxin-3去泛素化酶活性减弱, 能够阻止ataxin-3入核, 而第117位赖氨酸(K117) 则不参与ataxin-3核质转运。另有研究发现, 通过突变ataxin-3蛋白JD区域的第29位丝氨酸(S29)、泛素结合区域中的第340位(S340) 以及第352位丝氨酸(S352), 或加入CK2或糖原合成酶激酶3β (glycogen synthase kinase-3β, GSK3β) 抑制剂, 可以改变ataxin-3的磷酸化水平进而调控ataxin-3的核质转运和包涵体的形成[111], 而这一过程和NLS没有关联。大量证据表明ataxin-3蛋白能够被包括半胱天冬酶(caspase) 和Ca2+依赖的蛋白水解酶(calpain) 切割, 会产生含有NLS和异常扩增polyQ的ataxin-3小片段, 而该片段更易于进入细胞核加剧蛋白聚集体的形成, 比全长ataxin-3蛋白毒性更大, 因此突变ataxin-3的切割被认为是导致SCA3细胞毒性的关键因素[112-115]。此外, 热应激和氧化应激(包括过氧化氢处理) 均能够促进ataxin-3从细胞质进入细胞核, 可能受到JD区域的第111位丝氨酸(S111) 的调控, 但这一过程和去泛素化酶活性、CK2依赖的磷酸化以及NLS无关[116], 有证据表明Ran GDP/GTP浓度比降低、Nups的定位错误、importins/exportins的功能改变以及核膜完整性降低均能够影响氧化应激过程, 这也能很好地解释为什么氧化应激能够调控ataxin-3核转运[117]。
4.3 核质转运受体对ataxin-3核质转运的调控关于ataxin-3蛋白的核质转运受体的相关研究发现核质转运受体importin α4 (KPNA3) 和importin-13 (IPO13) 能够调控ataxin-3入核, 促使核内包涵体的形成进而加重疾病症状[109]。在SCA3果蝇模型和小鼠模型中, 下调importin α4或过表达XPO1能够缓解疾病症状并减少包涵体的形成。课题组前期研究[118]发现, 在SCA3细胞模型中, 以ataxin-3核质转运为靶点, 双硫仑(disulfiram) 能够加速ataxin-3入核, 进而加重因入核诱发的细胞凋亡。过表达importin α1 (KPNA2) 能够促进ataxin-3入核且增加包涵体的数量, 而且GST-pull down实验表明importin α1和ataxin-3直接相互作用, 然而importin α7却没有发现该作用[119]。以核质转运受体importin α1为药物靶点, 双丙戊酸钠通过影响importin α1的细胞定位能够直接调控ataxin-3核质转运以及包涵体的形成, 并减少ataxin-3入核诱发的细胞凋亡[120]。以上研究表明, 多个importin α共同参与ataxin-3的importin α/β经典入核途径。由此可见, 以ataxin-3蛋白核质转运为靶点, 能够有效改善SCA3的疾病症状, 是一个非常有潜力的治疗药物研发靶点。
5 其他神经退行性疾病AD俗称老年痴呆症, 是一种发病进程缓慢、随着时间不断恶化的神经退化性疾病, 疾病的进程与大脑中的β-淀粉样蛋白质纤维状斑块沉积和tau蛋白有关。已有越来越多的直接证据表明, AD的核质转运异常。在AD患者的大脑中, 带有苯丙氨酸-甘氨酸重复结构域(FG结构域) 的Nups在核膜的错误定位与胞质tau聚集体相关, 这表明NCT功能在AD中受到破坏, 其具体机制可能和tau过度磷酸化(p-tau) 有关, p-tau与Nup98直接发生作用, 促进tau纤维化, 通过堵塞NPC或通过隔离Nups到胞浆抑制NCT功能[121]。此外, 从AD患者脑组织中分离出的细胞核对荧光标记的葡聚糖显示出更高的渗透性, 这表明NPC的通透屏障或核膜发生了变化, 且RanGTP在核质浓度梯度降低, 表明主动转运过程遭到破坏[122]。在AD患者的神经细胞中发现FG-Nup62核内形态和核蛋白受体importin α1定位都发生异常[123, 124], 但其他核孔蛋白如Nup54、POM121、Nup88、Nup153、Nup133和Nup214并没有明显变化, 这表明细胞的核孔复合物并没有遭到完全破坏[121, 124]。
脊髓延髓肌萎缩症(spinal and bulbar muscular atrophy, SBMA), 又称肯尼迪病(Kennedy disease, KD), 也是一类多聚谷氨酰胺疾病, 由于雄激素受体(androgen receptor, AR) 基因第1个外显子三核苷酸重复序列CAG重复扩增导致的X染色体隐性遗传的神经系统变性疾病[125]。AR蛋白的核转运在SBMA致病机制过程中起到了重要的作用[126]。研究表明, 含有谷氨酰胺扩增的AR基因的出核遭受损伤, 这一过程的出现可能早于核内聚集体。此外, 通过额外的出核信号促使AR出核, 能够减少核内聚集体的形成以及诱发的细胞毒性[127]。AR包含一段75个氨基酸区域(残基743~817) 在AR受体结合区域(LBD) 调控AR出核。此外, DNA结合结构域(DBD) 和铰链区中的残基也对出核有影响[127]。核转运异常对SBMA不像对ALS或者HD疾病的影响那么广泛, Ran相关的核质转运以及RanGAP1的定位并没有异常, 但SBMA核转运异常可能和AR特异性S650磷酸化减弱有关, 受到MAPK激酶4/JNK和MAPK激酶6/p38应激激酶信号通路调控[127]。
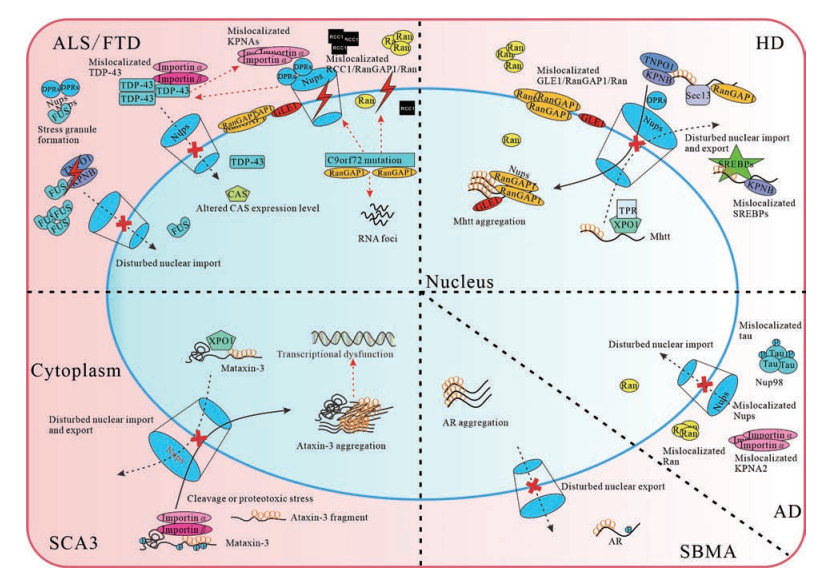
6 结语和展望已有越来越多的证据表明, 核质转运障碍是神经退行性疾病发病机制中的关键起始因素, 核孔蛋白和核转运受体的损伤往往是这些疾病的典型特征[1]。近两年发表在《Cell》等杂志的研究成果表明, 细胞的核质转运通路与疾病的致病蛋白可能存在相互作用, 不仅表现在核质转运通路对致病蛋白核质转运的影响, 还表现在致病蛋白对RanGTP/RanGDP浓度梯度、Ran调控蛋白的细胞定位以及核膜结构的破坏等方面, 同时也会造成核孔的渗透性增强, 减少核输入受体的利用率, 使更多的胞浆蛋白漏到核内, 导致被动转运功能受损, 造成恶性循环。对于ALS和FTD而言, 入核作用可能比出核影响要大, 抑制入核能够中和入核缺陷造成的影响。但是在polyQ疾病中的入核现象研究得很少, 出核影响要大些(图 3)。重要的是, 入核蛋白importins具有核转运受体和分子伴侣的双重功能, 这对于抑制疾病相关的RNA结合蛋白(RNA-binding proteins, RBPs) 的相变和纤维化是至关重要的, 如TDP-43和FUS。尽管核转运受体仍有许多未了解的功能, 但这些引人入胜的多功能蛋白已经成为神经退行性疾病新的治疗靶标。已有证据表明, 出核蛋白抑制剂包括KPT-350、KPT-335和KPT-276具有神经保护作用, 而Biogen研发的药物IIB100 (XPO1抑制剂) 已经进入临床I期用于治疗ALS患者[128]。
|
Figure 3 Representation of the disturbed nucleocytoplasmic transport in several neurodegenerative diseases. ALS/FTD: Impaired RNA export, disturbed Nups, altered distribution of RCC1/RanGAP1/Ran, mislocalizated GLE1, and importins and stress granule formation in C9orf72 mutations; Disturbed the nuclear transport function and TDP-43 localization in DPRs formation; Impaired NPC and altered Nups and CAS expression level involved in the presence of TDP-43 cytoplasmic aggregates; Damaged FUS import in the presence of aggregates containing FUS. HD: Intranuclear aggregates of mutant htt sequestering Nups, GLE1, and RanGAP1; Mislocalizated GLE1/RanGAP1/Ran and mislocalizated SREBPs in the presence of mutant htt; Impaired nuclear export in the presence of mutant htt aggregates. SCA3: Altered ataxin-3 translocation by posttranslational modification and proteotoxic stress; Ataxin-3 nuclear transport regulated by importins. AD: Disturbed nuclear import in the presence of mislocalizated tau; Mislocalizated Nups/Ran/KPNA2 in tau cytoplasmic aggregates. SBMA: Disturbed nuclear export in AR aggregation[19]. ALS/FTD: Amyotrophic lateral sclerosis/frontotemporal dementia; TDP-43: TAR DNA-binding protein 43; DPRs: Dipeptide repeat proteins; NPC: Nuclear pore complex; FUS: Fused in sarcoma; HD: Huntington's disease; AD: Alzheimer's disease; SBMA: Spinal and bulbar muscular atrophy; SGs: Stress granules; KPNA2: Karyopherin α2, importin α1; Mataxin-3: Mutant ataxin-3; mhtt: Mutant htt; XPO1: Exportin 1 |
虽然核质转运与神经退行性疾病的相关研究已经有了很大的进展, 但仍有许多难题尚未彻底攻克, ①核质运输缺陷在神经退行性疾病发病机制中的作用尚未得到充分评估; ②核质转运障碍是异常聚集体形成的原因还是结果仍未知; ③不同的致病蛋白聚集体是否破坏相同的核质转运途径, 是否存在一种干预方法可以应用到所有的神经退行性疾病中仍需要继续探索[4, 129, 130]。有意思的是, 核质转运还可能和衰老有直接关系, 蛋白质和RNA在细胞核和细胞质之间的动态交换对细胞功能至关重要, 但在正常衰老过程中会慢慢受损。如果细胞模型不是来源于神经细胞或者还没有达到衰老的程度, 致病蛋白积累时间不长, 可能对实验结果也有影响。综上所述, 虽然仍有一些悬而未决的问题, 但是核质转运异常已被认为是导致神经退行性疾病的一个重要原因, 这将为神经退行性疾病药物靶点的突破提供一个新的思路。
作者贡献: 王子见负责提出研究选题、实施研究过程、统稿全文和构建示意图, 获取科研经费支持; 李子恒负责整体文献调研、搜集、查阅和翻译文献; 常亦昆负责医学内容核对、文献翻译以及全文修改; 张甜和任媛媛负责稿件格式编辑和修改; 何凤琴负责审阅文章和指导工作。
利益冲突: 本文不存在与任何组织机构、任何研究者的利益冲突。
| [1] |
Fahrenkrog B, Harel A. Perturbations in traffic: aberrant nucleocytoplasmic transport at the heart of neurodegeneration[J]. Cells, 2018, 7: 232. DOI:10.3390/cells7120232 |
| [2] |
Liu ZL, Li XY, Zhang Q, et al. Establishment and application of a screening anti-HIV-1 drug model targeted nuclear trafficking of virus RNA[J]. Acta Pharm Sin (药学学报), 2010, 45: 257-262. |
| [3] |
Benarroch EE. Nucleocytoplasmic transport: mechanisms and involvement in neurodegenerative disease[J]. Neurology, 2019, 92: 757-764. DOI:10.1212/WNL.0000000000007305 |
| [4] |
Kim HJ, Taylor JP. Lost in transportation: nucleocytoplasmic transport defects in ALS and other neurodegenerative diseases[J]. Neuron, 2017, 96: 285-297. DOI:10.1016/j.neuron.2017.07.029 |
| [5] |
Xiong JM, Cui F. Progress in nucleocytoplasmic transport in pathogenesis of amyotrophic lateral sclerosis and frontotemporal dementia[J]. J Neurol Neurorehabil (神经病学与神经康复学杂志), 2018, 3: 167-171. |
| [6] |
Moore S, Rabichow BE, Sattler R. The Hitchhiker's guide to nucleocytoplasmic trafficking in neurodegeneration[J]. Neurochem Res, 2020, 45: 1306-1327. DOI:10.1007/s11064-020-02989-1 |
| [7] |
Guo JL, Xu CX. Research progress of structure and function of importin[J]. Chin J Cell Biol (中国细胞生物学学报), 2015, 37: 1013-1020. |
| [8] |
Li N, Lagier-Tourenne C. Nuclear pores: the gate to neurodegeneration[J]. Nat Neurosci, 2018, 21: 156-158. DOI:10.1038/s41593-017-0066-0 |
| [9] |
Wente SR, Rout MP. The nuclear pore complex and nuclear transport[J]. Cold Spring Harb Perspect Biol, 2010, 2: a000562. |
| [10] |
Peng JS, Gong JM. The mechanisms of protein sorting and translocation regulated by signal peptides[J]. Plant Physiol J (植物生理学报), 2011, 47: 9-17. |
| [11] |
Cheng G, Hu WX. Nuclear transport receptor--importin α and nucleocytoplasmic transport[J]. Chem Life (生命的化学), 2010, 30: 504-508. |
| [12] |
Dolgin E. The brain's traffic problems[J]. Science, 2019, 363: 221-223. DOI:10.1126/science.363.6424.221 |
| [13] |
Vucic S, Rothstein JD, Kiernan MC. Advances in treating amyotrophic lateral sclerosis: insights from pathophysiological studies[J]. Trends Neurosci, 2014, 37: 433-442. DOI:10.1016/j.tins.2014.05.006 |
| [14] |
Taylor JP, Brown RH, Cleveland DW. Decoding ALS: from genes to mechanism[J]. Nature, 2016, 539: 197-206. DOI:10.1038/nature20413 |
| [15] |
Gijselinck I, Van Langenhove T, van der Zee J, et al. A C9orf72 promoter repeat expansion in a Flanders-Belgian cohort with disorders of the frontotemporal lobar degeneration-amyotrophic lateral sclerosis spectrum: a gene identification study[J]. Lancet Neurol, 2012, 11: 54-65. DOI:10.1016/S1474-4422(11)70261-7 |
| [16] |
DeJesus-Hernandez M, Mackenzie IR, Boeve BF, et al. Expanded GGGGCC hexanucleotide repeat in noncoding region of C9orf72 causes chromosome 9p-linked FTD and ALS[J]. Neuron, 2011, 72: 245-256. DOI:10.1016/j.neuron.2011.09.011 |
| [17] |
Swinnen B, Robberecht W. The phenotypic variability of amyotrophic lateral sclerosis[J]. Nat Rev Neurol, 2014, 10: 661-670. DOI:10.1038/nrneurol.2014.184 |
| [18] |
Lomen-Hoerth C, Anderson T, Miller B. The overlap of amyotrophic lateral sclerosis and frontotemporal dementia[J]. Neurology, 2002, 59: 1077-1079. DOI:10.1212/WNL.59.7.1077 |
| [19] |
Bitetto G, Di Fonzo A. Nucleo-cytoplasmic transport defects and protein aggregates in neurodegeneration[J]. Transl Neurodegener, 2020, 9: 25. DOI:10.1186/s40035-020-00205-2 |
| [20] |
Zhang K, Donnelly CJ, Haeusler AR, et al. The C9orf72 repeat expansion disrupts nucleocytoplasmic transport[J]. Nature, 2015, 525: 56-61. DOI:10.1038/nature14973 |
| [21] |
Jovičić A, Mertens J, Boeynaems S, et al. Modifiers of C9orf72 dipeptide repeat toxicity connect nucleocytoplasmic transport defects to FTD/ALS[J]. Nat Neurosci, 2015, 18: 1226-1229. DOI:10.1038/nn.4085 |
| [22] |
Boeynaems S, Bogaert E, Van Damme P, et al. Inside out: the role of nucleocytoplasmic transport in ALS and FTLD[J]. Acta Neuropathol, 2016, 132: 159-173. DOI:10.1007/s00401-016-1586-5 |
| [23] |
Solomon DA, Stepto A, Au WH, et al. A feedback loop between dipeptide-repeat protein, TDP-43 and karyopherin-alpha mediates C9orf72-related neurodegeneration[J]. Brain, 2018, 141: 2908-2924. DOI:10.1093/brain/awy241 |
| [24] |
Freibaum BD, Lu Y, Lopez-Gonzalez R, et al. GGGGCC repeat expansion in C9orf72 compromises nucleocytoplasmic transport[J]. Nature, 2015, 525: 129-133. DOI:10.1038/nature14974 |
| [25] |
Nousiainen HO, Kestilä M, Pakkasjärvi N, et al. Mutations in mRNA export mediator GLE1 result in a fetal motoneuron disease[J]. Nat Genet, 2008, 40: 155-157. DOI:10.1038/ng.2007.65 |
| [26] |
Kaneb HM, Folkmann AW, Belzil VV, et al. Deleterious mutations in the essential mRNA metabolism factor, hGle1, in amyotrophic lateral sclerosis[J]. Hum Mol Genet, 2015, 24: 1363-1373. DOI:10.1093/hmg/ddu545 |
| [27] |
Gasset-Rosa F, Chillon-Marinas C, Goginashvili A, et al. Polyglutamine-expanded huntingtin exacerbates age-related disruption of nuclear integrity and nucleocytoplasmic transport[J]. Neuron, 2017, 94: 48-57. e4. DOI:10.1016/j.neuron.2017.03.027 |
| [28] |
Renton AE, Majounie E, Waite A, et al. A hexanucleotide repeat expansion in C9ORF72 is the cause of chromosome 9p21-linked ALS-FTD[J]. Neuron, 2011, 72: 257-268. DOI:10.1016/j.neuron.2011.09.010 |
| [29] |
Shang J, Yamashita T, Nakano Y, et al. Aberrant distributions of nuclear pore complex proteins in ALS mice and ALS patients[J]. Neuroscience, 2017, 350: 158-168. DOI:10.1016/j.neuroscience.2017.03.024 |
| [30] |
Kinoshita Y, Ito H, Hirano A, et al. Nuclear contour irregularity and abnormal transporter protein distribution in anterior horn cells in amyotrophic lateral sclerosis[J]. J Neuropathol Exp Neurol, 2009, 68: 1184-1192. DOI:10.1097/NEN.0b013e3181bc3bec |
| [31] |
Coyne AN, Zaepfel BL, Hayes L, et al. G4C2 repeat RNA initiates a POM121-mediated reduction in specific nucleoporins in C9orf72 ALS/FTD[J]. Neuron, 2020, 107: 1124-1140. e11. DOI:10.1016/j.neuron.2020.06.027 |
| [32] |
Zhang YJ, Gendron TF, Grima JC, et al. C9ORF72 poly(GA) aggregates sequester and impair HR23 and nucleocytoplasmic transport proteins[J]. Nat Neurosci, 2016, 19: 668-677. DOI:10.1038/nn.4272 |
| [33] |
Shi KY, Mori E, Nizami ZF, et al. Toxic PRn poly-dipeptides encoded by the C9orf72 repeat expansion block nuclear import and export[J]. Proc Natl Acad Sci U S A, 2017, 114: E1111-E1117. DOI:10.1073/pnas.1620293114 |
| [34] |
Lee KH, Zhang P, Kim HJ, et al. C9orf72 dipeptide repeats impair the assembly, dynamics, and function of membraneless organelles[J]. Cell, 2016, 167: 774-788. DOI:10.1016/j.cell.2016.10.002 |
| [35] |
Lin Y, Mori E, Kato M, et al. Toxic PR poly-dipeptides encoded by the C9orf72 repeat expansion target LC domain polymers[J]. Cell, 2016, 167: 789-802. DOI:10.1016/j.cell.2016.10.003 |
| [36] |
Khosravi B, Hartmann H, May S, et al. Cytoplasmic poly-GA aggregates impair nuclear import of TDP-43 in C9orf72 ALS/FTLD[J]. Hum Mol Genet, 2017, 26: 790-800. |
| [37] |
Hayes LR, Duan L, Bowen K, et al. C9orf72 arginine-rich dipeptide repeat proteins disrupt karyopherin-mediated nuclear import[J]. Elife, 2020, 9: e51685. DOI:10.7554/eLife.51685 |
| [38] |
Saberi S, Stauffer JE, Jiang J, et al. Sense-encoded poly-GR dipeptide repeat proteins correlate to neurodegeneration and uniquely co-localize with TDP-43 in dendrites of repeat-expanded C9orf72 amyotrophic lateral sclerosis[J]. Acta Neuropathol, 2018, 135: 459-474. DOI:10.1007/s00401-017-1793-8 |
| [39] |
Zhang K, Daigle JG, Cunningham KM, et al. Stress granule assembly disrupts nucleocytoplasmic transport[J]. Cell, 2018, 173: 958-971. e17. DOI:10.1016/j.cell.2018.03.025 |
| [40] |
Zhang YJ, Gendron TF, Ebbert MTW, et al. Poly(GR) impairs protein translation and stress granule dynamics in C9orf72-associated frontotemporal dementia and amyotrophic lateral sclerosis[J]. Nat Med, 2018, 24: 1136-1142. DOI:10.1038/s41591-018-0071-1 |
| [41] |
Vanneste J, Vercruysse T, Boeynaems S, et al. C9orf72-generated poly-GR and poly-PR do not directly interfere with nucleocytoplasmic transport[J]. Sci Rep, 2019, 9: 15728. DOI:10.1038/s41598-019-52035-6 |
| [42] |
Birsa N, Bentham MP, Fratta P. Cytoplasmic functions of TDP-43 and FUS and their role in ALS[J]. Semin Cell Dev Biol, 2020, 9: 193-201. |
| [43] |
Neumann M, Sampathu DM, Kwong LK, et al. Ubiquitinated TDP-43 in frontotemporal lobar degeneration and amyotrophic lateral sclerosis[J]. Science, 2006, 314: 130. DOI:10.1126/science.1134108 |
| [44] |
Weskamp K, Barmada SJ. TDP43 and RNA instability in amyotrophic lateral sclerosis[J]. Brain Res, 2018, 1693: 67-74. DOI:10.1016/j.brainres.2018.01.015 |
| [45] |
Svahn AJ, Don EK, Badrock AP, et al. Nucleo-cytoplasmic transport of TDP-43 studied in real time: impaired microglia function leads to axonal spreading of TDP-43 in degenerating motor neurons[J]. Acta Neuropathol, 2018, 136: 445-459. DOI:10.1007/s00401-018-1875-2 |
| [46] |
Nakashima-Yasuda H, Uryu K, Robinson J, et al. Co-morbidity of TDP-43 proteinopathy in Lewy body related diseases[J]. Acta Neuropathol, 2007, 114: 221-229. DOI:10.1007/s00401-007-0261-2 |
| [47] |
Uryu K, Nakashima-Yasuda H, Forman MS, et al. Concomitant TAR-DNA-binding protein 43 pathology is present in Alzheimer disease and corticobasal degeneration but not in other tauopathies[J]. J Neuropathol Exp Neurol, 2008, 67: 555-564. DOI:10.1097/NEN.0b013e31817713b5 |
| [48] |
Wilson AC, Dugger BN, Dickson DW, et al. TDP-43 in aging and Alzheimer's disease-a review[J]. Int J Clin Exp Pathol, 2011, 4: 147-155. |
| [49] |
Chou CC, Zhang Y, Umoh ME, et al. TDP-43 pathology disrupts nuclear pore complexes and nucleocytoplasmic transport in ALS/FTD[J]. Nat Neurosci, 2018, 21: 228-239. DOI:10.1038/s41593-017-0047-3 |
| [50] |
Heyburn L, VSSS Sajja, Long JB. The role of TDP-43 in military-relevant TBI and chronic neurodegeneration[J]. Front Neurol, 2019, 10: 680. DOI:10.3389/fneur.2019.00680 |
| [51] |
Smith C, Malek N, Grosset K, et al. Neuropathology of dementia in patients with Parkinson's disease: a systematic review of autopsy studies[J]. J Neurol Neurosurg Psychiatry, 2019, 90: 1234-1243. |
| [52] |
Matej R, Tesar A, Rusina R. Alzheimer's disease and other neurodegenerative dementias in comorbidity: a clinical and neuropathological overview[J]. Clin Biochem, 2019, 73: 26-31. DOI:10.1016/j.clinbiochem.2019.08.005 |
| [53] |
Nishimura AL, Zupunski V, Troakes C, et al. Nuclear import impairment causes cytoplasmic trans-activation response DNA-binding protein accumulation and is associated with frontotemporal lobar degeneration[J]. Brain, 2010, 133: 1763-1771. DOI:10.1093/brain/awq111 |
| [54] |
Winton MJ, Igaz LM, Wong MM, et al. Disturbance of nuclear and cytoplasmic TAR DNA-binding protein (TDP-43) induces disease-like redistribution, sequestration, and aggregate formation[J]. J Biol Chem, 2008, 283: 13302-13309. DOI:10.1074/jbc.M800342200 |
| [55] |
Boeynaems S, Bogaert E, Michiels E, et al. Drosophila screen connects nuclear transport genes to DPR pathology in c9ALS/FTD[J]. Sci Rep, 2016, 6: 20877. DOI:10.1038/srep20877 |
| [56] |
Zhang YJ, Xu YF, Cook C, et al. Aberrant cleavage of TDP-43 enhances aggregation and cellular toxicity[J]. Proc Natl Acad Sci U S A, 2009, 106: 7607-7612. DOI:10.1073/pnas.0900688106 |
| [57] |
Pinarbasi ES, Cağatay T, Fung HYJ, et al. Active nuclear import and passive nuclear export are the primary determinants of TDP-43 localization[J]. Sci Rep, 2018, 8: 7083. DOI:10.1038/s41598-018-25008-4 |
| [58] |
Archbold HC, Jackson KL, Arora A, et al. TDP43 nuclear export and neurodegeneration in models of amyotrophic lateral sclerosis and frontotemporal dementia[J]. Sci Rep, 2018, 8: 4606. DOI:10.1038/s41598-018-22858-w |
| [59] |
Ederle H, Funk C, Abou-Ajram C, et al. Nuclear egress of TDP-43 and FUS occurs independently of exportin-1/CRM1[J]. Sci Rep, 2018, 8: 7084. DOI:10.1038/s41598-018-25007-5 |
| [60] |
Gasset-Rosa F, Lu S, Yu H, et al. Cytoplasmic TDP-43 de-mixing independent of stress granules drives inhibition of nuclear import, loss of nuclear TDP-43, and cell death[J]. Neuron, 2019, 102: 339-357. DOI:10.1016/j.neuron.2019.02.038 |
| [61] |
Prpar Mihevc S, Darovic S, Kovanda A, et al. Nuclear trafficking in amyotrophic lateral sclerosis and frontotemporal lobar degeneration[J]. Brain, 2017, 140: 13-26. DOI:10.1093/brain/aww197 |
| [62] |
Woerner AC, Frottin F, Hornburg D, et al. Cytoplasmic protein aggregates interfere with nucleocytoplasmic transport of protein and RNA[J]. Science, 2016, 351: 173-176. DOI:10.1126/science.aad2033 |
| [63] |
Maurel C, Chami AA, Thépault RA, et al. A role for SUMOylation in the formation and cellular localization of TDP-43 aggregates in amyotrophic lateral sclerosis[J]. Mol Neurobiol, 2020, 57: 1361-1373. DOI:10.1007/s12035-019-01810-7 |
| [64] |
Dormann D, Rodde R, Edbauer D, et al. ALS-associated fused in sarcoma (FUS) mutations disrupt transportin-mediated nuclear import[J]. EMBO J, 2010, 29: 2841-2857. DOI:10.1038/emboj.2010.143 |
| [65] |
Hofweber M, Hutten S, Bourgeois B, et al. Phase separation of FUS is suppressed by its nuclear import receptor and arginine methylation[J]. Cell, 2018, 173: 706-719. DOI:10.1016/j.cell.2018.03.004 |
| [66] |
Neumann M, Valori CF, Ansorge O, et al. Transportin 1 accumulates specifically with FET proteins but no other transportin cargos in FTLD-FUS and is absent in FUS inclusions in ALS with FUS mutations[J]. Acta Neuropathol, 2012, 124: 705-716. DOI:10.1007/s00401-012-1020-6 |
| [67] |
Takeuchi R, Toyoshima Y, Tada M, et al. Transportin 1 accumulates in FUS inclusions in adult-onset ALS without FUS mutation[J]. Neuropathol Appl Neurobiol, 2013, 39: 580-584. DOI:10.1111/nan.12022 |
| [68] |
Yoshizawa T, Ali R, Jiou J, et al. Nuclear import receptor inhibits phase separation of FUS through binding to multiple sites[J]. Cell, 2018, 173: 693-705. e22. DOI:10.1016/j.cell.2018.03.003 |
| [69] |
Devoy A, Kalmar B, Stewart M, et al. Humanized mutant FUS drives progressive motor neuron degeneration without aggregation in 'FUSDelta14' knockin mice[J]. Brain, 2017, 140: 2797-2805. DOI:10.1093/brain/awx248 |
| [70] |
Scekic-Zahirovic J, Oussini HE, Mersmann S, et al. Motor neuron intrinsic and extrinsic mechanisms contribute to the pathogenesis of FUS-associated amyotrophic lateral sclerosis[J]. Acta Neuropathol, 2017, 133: 887-906. DOI:10.1007/s00401-017-1687-9 |
| [71] |
Dormann D, Madl T, Valori CF, et al. Arginine methylation next to the PY-NLS modulates transportin binding and nuclear import of FUS[J]. EMBO J, 2012, 31: 4258-4275. DOI:10.1038/emboj.2012.261 |
| [72] |
Suárez-Calvet M, Neumann M, Arzberger T, et al. Monomethylated and unmethylated FUS exhibit increased binding to transportin and distinguish FTLD-FUS from ALS-FUS[J]. Acta Neuropathol, 2016, 131: 587-604. DOI:10.1007/s00401-016-1544-2 |
| [73] |
Darovic S, Prpar Mihevc S, Župunski V, et al. Phosphorylation of C-terminal tyrosine residue 526 in FUS impairs its nuclear import[J]. J Cell Sci, 2015, 128: 4151-4159. |
| [74] |
Steyaert J, Scheveneels W, Vanneste J, et al. FUS-induced neurotoxicity in Drosophila is prevented by downregulating nucleocytoplasmic transport proteins[J]. Hum Mol Genet, 2018, 27: 4103-4116. |
| [75] |
Bessert DA, Gutridge KL, Dunbar JC, et al. The identification of a functional nuclear localization signal in the Huntington disease protein[J]. Brain Res Mol Brain Res, 1995, 33: 165-173. DOI:10.1016/0169-328X(95)00124-B |
| [76] |
Desmond CR, Atwal RS, Xia J, et al. Identification of a karyopherin β1/β2 proline-tyrosine nuclear localization signal in huntingtin protein[J]. J Biol Chem, 2012, 287: 39626-39633. DOI:10.1074/jbc.M112.412379 |
| [77] |
Xia J, Lee DH, Taylor J, et al. Huntingtin contains a highly conserved nuclear export signal[J]. Hum Mol Genet, 2003, 12: 1393-1403. DOI:10.1093/hmg/ddg156 |
| [78] |
Maiuri T, Woloshansky T, Xia J, et al. The huntingtin N17 domain is a multifunctional CRM1 and Ran-dependent nuclear and cilial export signal[J]. Hum Mol Genet, 2013, 22: 1383-1394. DOI:10.1093/hmg/dds554 |
| [79] |
Zheng Z, Li A, Holmes BB, et al. An N-terminal nuclear export signal regulates trafficking and aggregation of Huntingtin (Htt) protein exon 1[J]. J Biol Chem, 2013, 288: 6063-6071. DOI:10.1074/jbc.M112.413575 |
| [80] |
Yan Y, Peng D, Tian J, et al. Essential sequence of the N-terminal cytoplasmic localization-related domain of huntingtin and its effect on huntingtin aggregates[J]. Sci China Life Sci, 2011, 54: 342-350. DOI:10.1007/s11427-011-4151-4 |
| [81] |
Son S, Bowie LE, Maiuri T, et al. High-mobility group box 1 links sensing of reactive oxygen species by huntingtin to its nuclear entry[J]. J Biol Chem, 2019, 294: 1915-1923. DOI:10.1074/jbc.RA117.001440 |
| [82] |
Gu X, Greiner ER, Mishra R, et al. Serines 13 and 16 are critical determinants of full-length human mutant huntingtin induced disease pathogenesis in HD mice[J]. Neuron, 2009, 64: 828-840. DOI:10.1016/j.neuron.2009.11.020 |
| [83] |
Thompson LM, Aiken CT, Kaltenbach LS, et al. IKK phosphorylates huntingtin and targets it for degradation by the proteasome and lysosome[J]. J Cell Biol, 2009, 187: 1083-1099. DOI:10.1083/jcb.200909067 |
| [84] |
Atwal RS, Desmond CR, Caron N, et al. Kinase inhibitors modulate huntingtin cell localization and toxicity[J]. Nat Chem Biol, 2011, 7: 453-460. DOI:10.1038/nchembio.582 |
| [85] |
Havel LS, Wang CE, Wade B, et al. Preferential accumulation of N-terminal mutant huntingtin in the nuclei of striatal neurons is regulated by phosphorylation[J]. Hum Mol Genet, 2011, 20: 1424-1437. DOI:10.1093/hmg/ddr023 |
| [86] |
DeGuire SM, Ruggeri FS, Fares MB, et al. N-terminal Huntingtin (Htt) phosphorylation is a molecular switch regulating Htt aggregation, helical conformation, internalization, and nuclear targeting[J]. J Biol Chem, 2018, 293: 18540-18558. DOI:10.1074/jbc.RA118.004621 |
| [87] |
Grima JC, Daigle JG, Arbez N, et al. Mutant Huntingtin disrupts the nuclear pore complex[J]. Neuron, 2017, 94: 93-107. e6. DOI:10.1016/j.neuron.2017.03.023 |
| [88] |
Veldman MB, Yang XW. Huntington's disease: nuclear gatekeepers under attack[J]. Neuron, 2017, 94: 1-4. DOI:10.1016/j.neuron.2017.03.032 |
| [89] |
Hosp F, Vossfeldt H, Heinig M, et al. Quantitative interaction proteomics of neurodegenerative disease proteins[J]. Cell Rep, 2015, 11: 1134-1146. DOI:10.1016/j.celrep.2015.04.030 |
| [90] |
Bui KH, von Appen A, DiGuilio AL, et al. Integrated structural analysis of the human nuclear pore complex scaffold[J]. Cell, 2013, 155: 1233-1243. DOI:10.1016/j.cell.2013.10.055 |
| [91] |
Lussi YC, Hügi I, Laurell E, et al. The nucleoporin Nup88 is interacting with nuclear lamin A[J]. Mol Biol Cell, 2011, 22: 1080-1090. DOI:10.1091/mbc.e10-05-0463 |
| [92] |
Truant R, Atwal RS, Burtnik A. Nucleocytoplasmic trafficking and transcription effects of huntingtin in Huntington's disease[J]. Prog Neurobiol, 2007, 83: 211-227. DOI:10.1016/j.pneurobio.2006.11.004 |
| [93] |
Cornett J, Cao F, Wang CE, et al. Polyglutamine expansion of huntingtin impairs its nuclear export[J]. Nat Genet, 2005, 37: 198-204. DOI:10.1038/ng1503 |
| [94] |
Bañez-Coronel M, Ayhan F, Tarabochia AD, et al. RAN translation in Huntington disease[J]. Neuron, 2015, 88: 667-677. DOI:10.1016/j.neuron.2015.10.038 |
| [95] |
Di Pardo A, Monyror J, Morales LC, et al. Mutant huntingtin interacts with the sterol regulatory element-binding proteins and impairs their nuclear import[J]. Hum Mol Genet, 2020, 29: 418-431. DOI:10.1093/hmg/ddz298 |
| [96] |
Zheng J, Yang J, Choe YJ, et al. Role of the ribosomal quality control machinery in nucleocytoplasmic translocation of polyQ-expanded huntingtin exon-1[J]. Biochem Biophys Res Commun, 2017, 493: 708-717. DOI:10.1016/j.bbrc.2017.08.126 |
| [97] |
Li T, Hou X, Chen Z, et al. RNA expression profile and potential biomarkers in patients with spinocerebellar ataxia type 3 from mainland China[J]. Front Genet, 2019, 10: 566. DOI:10.3389/fgene.2019.00566 |
| [98] |
Chen Z, Wang P, Wang C, et al. Updated frequency analysis of spinocerebellar ataxia in China[J]. Brain, 2018, 141: e22. DOI:10.1093/brain/awy016 |
| [99] |
Saute JA, Jardim LB. Machado Joseph disease: clinical and genetic aspects, and current treatment[J]. Expert Opin Orphan Drugs, 2015, 3: 1-19. DOI:10.1517/21678707.2015.1084714 |
| [100] |
Matos CA, de Almeida LP, Nóbrega C. Machado-Joseph disease/spinocerebellar ataxia type 3:lessons from disease pathogenesis and clues into therapy[J]. J Neurochem, 2019, 148: 8-28. DOI:10.1111/jnc.14541 |
| [101] |
Wang ZJ. Experimental and clinical strategies for treating spinocerebellar ataxia type 3[J]. Neuroscience, 2018, 371: 138-154. DOI:10.1016/j.neuroscience.2017.11.051 |
| [102] |
McLoughlin HS, Moore LR, Paulson HL. Pathogenesis of SCA3 and implications for other polyglutamine diseases[J]. Neurobiol Dis, 2020, 134: 104635. DOI:10.1016/j.nbd.2019.104635 |
| [103] |
Schmidt T, Landwehrmeyer GB, Schmitt I, et al. An isoform of ataxin-3 accumulates in the nucleus of neuronal cells in affected brain regions of SCA3 patients[J]. Brain Pathol, 1998, 8: 669-679. DOI:10.1111/j.1750-3639.1998.tb00193.x |
| [104] |
Warrick JM, Paulson HL, Gray-Board GL, et al. Expanded polyglutamine protein forms nuclear inclusions and causes neural degeneration in Drosophila[J]. Cell, 1998, 93: 939-949. DOI:10.1016/S0092-8674(00)81200-3 |
| [105] |
Da Silva JD, Teixeira-Castro A, Maciel P. From pathogenesis to novel therapeutics for spinocerebellar ataxia type 3:evading potholes on the way to translation[J]. Neurotherapeutics, 2019, 16: 1009-1031. DOI:10.1007/s13311-019-00798-1 |
| [106] |
Antony PM, Mäntele S, Mollenkopf P, et al. Identification and functional dissection of localization signals within ataxin-3[J]. Neurobiol Dis, 2009, 36: 280-292. DOI:10.1016/j.nbd.2009.07.020 |
| [107] |
Macedo-Ribeiro S, Cortes L, Maciel P, et al. Nucleocytoplasmic shuttling activity of ataxin-3[J]. PLoS One, 2009, 4: e5834. DOI:10.1371/journal.pone.0005834 |
| [108] |
Sowa AS, Martin E, Martins IM, et al. Karyopherin α-3 is a key protein in the pathogenesis of spinocerebellar ataxia type 3 controlling the nuclear localization of ataxin-3[J]. Proc Natl Acad Sci U S A, 2018, 115: E2624-E2633. DOI:10.1073/pnas.1716071115 |
| [109] |
Bichelmeier U, Schmidt T, Hübener J, et al. Nuclear localization of ataxin-3 is required for the manifestation of symptoms in SCA3:in vivo evidence[J]. J Neurosci, 2007, 27: 7418-7428. DOI:10.1523/JNEUROSCI.4540-06.2007 |
| [110] |
Todi SV, Scaglione KM, Blount JR, et al. Activity and cellular functions of the deubiquitinating enzyme and polyglutamine disease protein ataxin-3 are regulated by ubiquitination at lysine 117[J]. J Biol Chem, 2010, 285: 39303-39313. DOI:10.1074/jbc.M110.181610 |
| [111] |
Matos CA, Nóbrega C, Louros SR, et al. Ataxin-3 phosphorylation decreases neuronal defects in spinocerebellar ataxia type 3 models[J]. J Cell Biol, 2016, 212: 465-480. DOI:10.1083/jcb.201506025 |
| [112] |
Hübener J, Weber JJ, Richter C, et al. Calpain-mediated ataxin-3 cleavage in the molecular pathogenesis of spinocerebellar ataxia type 3(SCA3)[J]. Hum Mol Genet, 2013, 22: 508-518. DOI:10.1093/hmg/dds449 |
| [113] |
Simões AT, Gonçalves N, Nobre RJ, et al. Calpain inhibition reduces ataxin-3 cleavage alleviating neuropathology and motor impairments in mouse models of Machado-Joseph disease[J]. Hum Mol Genet, 2014, 23: 4932-4944. DOI:10.1093/hmg/ddu209 |
| [114] |
Weber JJ, Golla M, Guaitoli G, et al. A combinatorial approach to identify calpain cleavage sites in the Machado-Joseph disease protein ataxin-3[J]. Brain, 2017, 140: 1280-1299. DOI:10.1093/brain/awx039 |
| [115] |
Weber JJ, Haas E, Maringer Y, et al. Calpain-1 ablation partially rescues disease-associated hallmarks in models of Machado-Joseph disease[J]. Hum Mol Genet, 2020, 29: 892-906. DOI:10.1093/hmg/ddaa010 |
| [116] |
Reina CP, Zhong X, Pittman RN. Proteotoxic stress increases nuclear localization of ataxin-3[J]. Hum Mol Genet, 2010, 19: 235-249. DOI:10.1093/hmg/ddp482 |
| [117] |
Robijns J, Houthaeve G, Braeckmans K, et al. Loss of nuclear envelope integrity in aging and disease[J]. Int Rev Cell Mol Biol, 2018, 336: 205-222. |
| [118] |
Wang Z. Disulfiram facilitates ataxin-3 nuclear translocation and potentiates the cytotoxicity in a cell model of SCA3[J]. J Toxicol Sci, 2019, 44: 535-542. DOI:10.2131/jts.44.535 |
| [119] |
Wang Z, He F, Abeditashi M, et al. Divalproex sodium regulates ataxin-3 translocation likely by an importin α1-dependent pathway[J]. Neuroreport, 2019, 30: 760-764. DOI:10.1097/WNR.0000000000001246 |
| [120] |
Wang ZJ, Hanet A, Weishäupl D, et al. Divalproex sodium modulates nuclear localization of ataxin-3 and prevents cellular toxicity caused by expanded ataxin-3[J]. CNS Neurosci Ther, 2018, 24: 404-411. DOI:10.1111/cns.12795 |
| [121] |
Eftekharzadeh B, Daigle JG, Kapinos LE, et al. Tau protein disrupts nucleocytoplasmic transport in Alzheimer's disease[J]. Neuron, 2018, 99: 925-940. e7. DOI:10.1016/j.neuron.2018.07.039 |
| [122] |
Mastroeni D, Chouliaras L, Grover A, et al. Reduced RAN expression and disrupted transport between cytoplasm and nucleus; a key event in Alzheimer's disease pathophysiology[J]. PLoS One, 2013, 8: e53349. DOI:10.1371/journal.pone.0053349 |
| [123] |
Lee BJ, Cansizoglu AE, Süel KE, et al. Rules for nuclear localization sequence recognition by karyopherin beta 2[J]. Cell, 2006, 126: 543-558. DOI:10.1016/j.cell.2006.05.049 |
| [124] |
Sheffield LG, Miskiewicz HB, Tannenbaum LB, et al. Nuclear pore complex proteins in Alzheimer disease[J]. J Neuropathol Exp Neurol, 2006, 65: 45-54. DOI:10.1097/01.jnen.0000195939.40410.08 |
| [125] |
Katsuno M, Tanaka F, Adachi H, et al. Pathogenesis and therapy of spinal and bulbar muscular atrophy (SBMA)[J]. Prog Neurobiol, 2012, 99: 246-256. DOI:10.1016/j.pneurobio.2012.05.007 |
| [126] |
Montie HL, Cho MS, Holder L, et al. Cytoplasmic retention of polyglutamine-expanded androgen receptor ameliorates disease via autophagy in a mouse model of spinal and bulbar muscular atrophy[J]. Hum Mol Genet, 2009, 18: 1937-1950. DOI:10.1093/hmg/ddp115 |
| [127] |
Arnold FJ, Pluciennik A, Merry DE. Impaired nuclear export of polyglutamine-expanded androgen receptor in spinal and bulbar muscular atrophy[J]. Sci Rep, 2019, 9: 119. DOI:10.1038/s41598-018-36784-4 |
| [128] |
Biogen.A Study to Evaluate the Safety, Tolerability, Pharmacokinetics, and Pharmacodynamics of BⅡB100 Administered Orally to Adults with Amyotrophic Lateral Sclerosis[R]. Cambridge: Biogen, 2019. https://clinicaltrials.gov/ct2/show/NCT03945279.
|
| [129] |
Lester E, Parker R. The tau of nuclear-cytoplasmic transport[J]. Neuron, 2018, 99: 869-871. DOI:10.1016/j.neuron.2018.08.026 |
| [130] |
Hutten S, Dormann D. Nucleocytoplasmic transport defects in neurodegeneration-cause or consequence?[J]. Semin Cell Dev Biol, 2020, 9: 151-162. |
 2021, Vol. 56
2021, Vol. 56


