2. 中国医学科学院、北京协和医学院医药生物技术研究所, 北京 100050
2. Institute of Medicinal Biotechnology, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing 100050, China
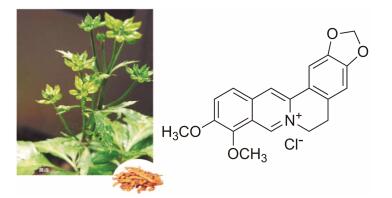
小檗碱(berberine, BBR, C20H19NO5, MW 336.37), 又称黄连素, 是从黄连(Coptis chinensis)等中草药中分离提取得到的一种异喹啉类生物碱(图 1)[1]。临床常用的是盐酸小檗碱(berberine hydrochloride, MW 371.81)。据报道, 小檗碱具有抗菌、降血糖、降血脂、降血压、抗肿瘤、抗氧化、抗痢疾和抗传染性原虫等药理活性[2-5]。其中小檗碱的抗菌作用是最早为人所知且用于临床的。本文将对小檗碱抗菌作用的研究进展进行综述, 以期为小檗碱的深度研发提供科学依据。
|
Figure 1 The herb and structure of berberine HCl[1] |
小檗碱是黄连的主要成分之一, 临床已经运用多年, 主要用于治疗肠道细菌性感染。最初发现小檗碱具有体外抗菌活性是在1969年由Amin等[6]首次报道的。报道指出小檗碱在体外对革兰阳性菌(G+)、革兰阴性菌(G-)和真菌都有显著的抑制活性。之后研究者对小檗碱的抗菌作用展开了深入的研究。Freile等[7]研究发现, 小檗碱在体外能够抑制金黄色葡萄球菌的生长。随后有大量实验指出, 小檗碱还能够在体外抑制耐甲氧西林金黄色葡萄球菌(MRSA)的生长[8, 9]。同时, 小檗碱对致病的肺炎链球菌[10]、无乳链球菌[11]抑菌作用也很明显。对于G-大肠杆菌, 小檗碱也有一定的抑制作用[12, 13], 但是抑制作用远远低于对G+菌的作用。小檗碱对G-痢疾杆菌的抑制作用非常显著[14, 15], 高于对G+菌的作用, 这也被认为是小檗碱发挥胃肠道感染治疗作用的特点之一。此外, 小檗碱对幽门螺旋杆菌[16]、结核分枝杆菌[17]和霍乱弧菌[18]等均表现出不同程度的抑菌活性。除了对细菌的抗菌作用外, 小檗碱还能够与抗真菌药物氟康唑等唑类药物联合使用, 明显增强抗真菌药物对多种临床分离真菌菌株的活性[19, 20]。小檗碱体外主要的抗菌活性及与临床主要抗菌药物相比较的结果如表 1[21, 22]所示。
| Table 1 In vitro antibacterial activity of berberine[21, 22]. *Since the minimum inhibitory concentration (MIC) of the same strain reported in different literatures are various, we select the average value here |
尽管小檗碱的抗菌作用弱, 在不同微生物之间的抗菌活性差异较大, 但与一般的抗生素相比, 小檗碱不容易产生耐药性[23]。此外, 有报道指出, 小檗碱属的植物除了能产生小檗碱外, 还能产生一种多药耐药外排泵NorA的抑制剂5'-MHC, 当小檗碱与5'-MHC联合使用时, 可以增加细菌内小檗碱的浓度, 减少产生对小檗碱的耐药性, 增加小檗碱的抗菌作用[24]。
2 小檗碱的抗菌作用机制小檗碱抗菌机制远未阐明, 可能与其抗菌效果偏弱有关; 此外, 传统上认为小檗碱是一个多靶点化合物, 可以作用于细菌代谢的多个途径及细菌产生致病性的多个过程, 增加了研究的复杂性。以下专门介绍几个研究结果, 说明小檗碱与细菌的相互作用, 为深入探索小檗碱抗菌作用机制提供研究思路。
2.1 小檗碱抑制菌体核酸的功能有研究表明, 小檗碱及其衍生物能够与菌体单链/双链DNA结合形成复合体[25], 并且能够抑制拓扑异构酶(TOP Ⅰ/Ⅱ)的活性[26-28], 有可能是通过抑制DNA的功能而发挥其抗菌作用的。Das等[29]通过热动力学技术和圆二色谱法分析得出, 小檗碱除了能与DNA结合外, 还与细菌双链RNA相互作用, 尤其是结合在AU碱基配对处, 影响RNA的正常功能。
2.2 小檗碱抑制菌体功能蛋白酶的活性小檗碱能够降低伤寒沙门氏菌中乙酰转移酶的活性, 并且呈剂量依赖性地减少转录及蛋白水平乙酰转移酶的量[30], 使细菌中芳基胺类物质的代谢受到阻碍, 导致细菌因非正常代谢而死亡。还有研究通过基因芯片分析, 小檗碱能够抑制金黄色葡萄球菌中的谷氨酰胺合成酶, 使得菌体中重要的氨基酸谷氨酰胺的合成受到影响[31], 推测这可能也是小檗碱的一种抗菌机制。
2.3 小檗碱抑制菌体分裂细菌FtsZ蛋白是菌体的分裂蛋白。FtsZ自我聚合成分裂隔板处的Z-ring, 在细菌菌体分裂过程中发挥着重要的作用。小檗碱能够抑制大肠杆菌FtsZ的GTP酶活性, 从而抑制Z-ring的形成[32]。核磁共振及分子对接实验表明, 小檗碱结合在大肠杆菌FtsZ的疏水GTP酶活性位点, 使得FtsZ不能发挥其GTP酶功能[33]。除此之外, 小檗碱还有可能与细菌菌体分裂蛋白FtsA、ZipA等相互作用影响菌体分裂[34]。
2.4 小檗碱抑制细菌致病性的作用Oh等[35]发现小檗碱能够抑制金黄色葡萄球菌转肽酶SrtA、SrtB的活性。SrtA和SrtB的主要功能是将金黄色葡萄球菌毒力因子蛋白铆钉在细胞壁外层, 小檗碱通过抑制两种不同亚型酶的活性影响金黄色葡萄球菌的致病性, 从而发挥其抑菌作用。小檗碱还能抑制大肠杆菌、链球菌等鞭毛的亚基装配, 影响其黏附作用[36], 达到抑菌效果。
2.5 小檗碱对胃肠道黏膜的保护作用及抗菌机制在对大肠杆菌和霍乱弧菌肠毒素引起的家兔、小鼠肠功能紊乱实验中, 小檗碱能够拮抗肠毒素的毒性作用[37], 减少细菌肠毒素导致的肠黏膜损伤及引起的电解质失调。还有研究表明, 小檗碱能够作为细菌脂多糖(LPS)的拮抗剂, 抑制机体LPS/TLR4信号通路, 并且抑制炎症因子NF-κB、IL-6、TNFα和IFNβ的分泌, 保护LPS引起的胃肠道黏膜损伤, 发挥其抗菌作用[38]。
2.6 小檗碱与肠道菌相互作用及抗菌机制小檗碱在肠道主要对痢疾杆菌效果较好(表 1), 而对其他菌抑制作用很弱(表 2)[39]。Wang等[40]报道小檗碱可以减少肠道菌产生ATP和NADH, 也可能是抑制细菌的机制之一。小檗碱已经在大量的人群中试用, 到目前为止, 即使在长期服用小檗碱的患者中, 也尚未见到口服小檗碱引起肠道菌群紊乱的报道[41]。实际上小檗碱可以减少肠道的致病菌, 而增加有益的细菌。Zhang等[42]报道小檗碱能够增加具有短链脂肪酸(SCFA)产生功能的Blautia和Allobaculum等菌属, 而SCFA能够调节肠道pH值、抗炎、调节人体代谢与免疫等功能; 同时, 小檗碱还能够抑制产生内毒素的Barnesiella和Butyricimonas等菌属, 而内毒素会损害肠道屏障、引起人体代谢和免疫失调等。
| Table 2 The antibacterial activity of berberine on 14 intestinal bacteria |
此外, Lv等[43]报道将小檗碱与万古霉素联用, 治疗梭状芽胞杆菌感染效果好于单独使用万古霉素, 其作用机制是由于小檗碱对万古霉素治疗造成的肠道杆菌数量及种类的破坏起到重塑作用, 通过小檗碱与肠道菌的相互作用增加万古霉素的抗感染治疗效果。由此可见, 小檗碱非但没有引起肠道正常菌群的菌群失调, 相反还能够调节肠道菌群结构, 促进肠道正常菌群的稳态环境。这也与目前已有研究结果相吻合, 小檗碱只对致病性肠道菌(如痢疾杆菌和幽门螺旋杆菌)有较强的抑菌活性, 一般剂量的小檗碱对其他正常肠道菌抑制作用很弱。临床使用小檗碱后的菌群失调尚未见报告。在中医里有“黄连厚肠胃”的说法, 说明其对肠道的有益之处。
由于小檗碱的结构属于季铵碱, 水溶性较差, 口服后难吸收, 血浆中生物利用度低。有不少研究者针对小檗碱在体内的吸收、代谢、分布进行了大量的研究。口服小檗碱吸收量少, 大量小檗碱聚集肠道与肠道菌相互作用。此外, 小檗碱被肠道菌中的硝基还原酶转化成易于吸收的二氢小檗碱等代谢产物, 这些代谢产物的抗菌作用更弱, 可能代表了细菌自我保护的机制之一[39]。
2.7 小檗碱抗菌的其他机制在小鼠感染大肠杆菌动物实验中, 小檗碱能够上调吞噬大肠杆菌的巨噬细胞表达caspase-1p 10和IL-1β, 从而激活AMPK通路[44], 同时, 还可以激活AMPK介导的巨噬细胞自噬作用[45], 产生抑菌效果。除了激活AMPK通路, 小檗碱通过抑制机体MEK/ERK MAPK通路[46], 抑制病原体的RNA和蛋白表达, 从而抑制病原体感染人体。小檗碱还能够与巨噬细胞中溶菌酶的色氨酸相结合[47], 形成复合体, 并且氧化色氨酸, 激活巨噬细胞氧化应激反应(ROS), 发挥其抑菌功效。
3 小檗碱抗菌作用的临床应用小檗碱最早运用于临床, 就是将其作为肠道感染的治疗药物。在成人感染大肠杆菌肠毒素引起的腹泻患者中, 给予小檗碱24 h后, 患者腹泻症状明显减轻[18]。对小儿细菌性肠炎, 小檗碱也表现出明显的治疗效果。小儿口服小檗碱治疗腹泻与成人效果相同。除此之外, 在常规抗感染及补液治疗的基础上, 使用盐酸小檗碱灌肠治疗小儿细菌性肠炎, 治疗效果优于只进行常规治疗的对照组患者[48]。而盐酸小檗碱在临床上也一直作为非处方药物用于治疗腹泻, 效果明确且无不良反应。然而, 英国1985年有报告指出, 小檗碱在临床对霍乱引起的水样腹泻并无效果[49]。因此, 小檗碱对不同细菌引起的腹泻疗效可能有差别, 值得认真研究。
近年来, 小檗碱的抗菌作用也被越来越广泛地运用到其他临床治疗中。将小檗碱涂抹于脓包疮患者患处表面局部给药, 脓包疮感染明显好转, 获得较好治疗效果[50]。小檗碱与抗真菌西药联合应用, 显示出良好的协同作用, 用于临床真菌感染性疾病的治疗[51]。小檗碱与奥美拉唑、阿莫西林联用, 治疗幽门螺旋杆菌感染引起的胃炎中, 对幽门螺旋杆菌的根除效果好于只用奥美拉唑、阿莫西林对照组患者[52], 说明了小檗碱的抗菌增效作用。目前, 小檗碱的临床给药形式以口服和体表局部用药为主, 尚未见静脉全身给药的报道。目前认为小檗碱的直接抗菌活性是其治疗细菌性感染的主要基础。
4 小结小檗碱对多种微生物均有不同程度的抑制效果, 尤其是对革兰阴性菌中的痢疾杆菌效果明显。与一般抗生素相比, 虽然小檗碱的抗菌作用相对较弱, 但是由于小檗碱使用安全, 相对不易产生耐药, 更重要的是能聚集于肠道, 所以目前主要用于胃肠道细菌感染。对小檗碱抗菌机制的深入研究, 以及对肠道菌群的作用了解, 将有助于小檗碱(及衍生物)的深度研发和运用。
| [1] | Li GR. Illustrated Handbook for 800 Kinds of Chinese Medicinal Herbs (800种中草药彩色图鉴)[M]. Fujian: Fujian Science and Technology Press, 2017. |
| [2] | Imenshahidi M, Hosseinzadeh H. Berberis vulgaris and berberine:an update review[J]. Phytother Res, 2016, 30: 1745–1764. DOI:10.1002/ptr.v30.11 |
| [3] | Ortiz LM, Lombardi P, Tillhon M, et al. Berberine, an epiphany against cancer[J]. Molecules, 2014, 19: 12349–12367. DOI:10.3390/molecules190812349 |
| [4] | Huang ZJ, Zeng Y, Lan P, et al. Advances in structural modifications and biological activities of berberine:an active compound in traditional Chinese medicine[J]. Mini Rev Med Chem, 2011, 11: 1122–1129. DOI:10.2174/138955711797655362 |
| [5] | Li B, Zhu WL, Chen KX. Advances in the study of berberine and its derivatives[J]. Acta Pharm Sin (药学学报), 2008, 43: 773–787. |
| [6] | Amin AH, Subbaiah TV, Abbasi KM. Berberine sulfate:antimicrobial activity, bioassay, and mode of action[J]. Can J Microbiol, 1969, 15: 1067–1076. DOI:10.1139/m69-190 |
| [7] | Freile ML, Giannini F, Pucci G, et al. Antimicrobial activity of aqueous extracts and of berberine isolated from Berberis heterophylla[J]. Fitoterapia, 2003, 74: 702–705. DOI:10.1016/S0367-326X(03)00156-4 |
| [8] | Yu HH, Kim KJ, Cha JD, et al. Antimicrobial activity of berberine alone and in combination with ampicillin or oxacillin against methicillin-resistant Staphylococcus aureus[J]. J Med Food, 2005, 8: 454–461. DOI:10.1089/jmf.2005.8.454 |
| [9] | Chu M, Zhang MB, Liu YC, et al. Role of berberine in the treatment of methicillin-resistant Staphylococcus aureus infections[J]. Sci Rep, 2016, 6: 24748. DOI:10.1038/srep24748 |
| [10] | Kang S, Li Z, Yin Z, et al. The antibacterial mechanism of berberine against Actinobacillus pleuropneumoniae[J]. Nat Prod Res, 2015, 29: 2203–2206. DOI:10.1080/14786419.2014.1001388 |
| [11] | Peng L, Kang S, Yin Z, et al. Antibacterial activity and mechanism of berberine against Streptococcus agalactiae[J]. Int J Clin Exp Pathol, 2015, 8: 5217–5223. |
| [12] | Liang RM, Yong XL, Duan YQ, et al. Potent in vitro synergism of fusidic acid (FA) and berberine chloride (BBR) against clinical isolates of methicillin-resistant Staphylococcus aureus (MRSA)[J]. World J Microbiol Biotechnol, 2014, 30: 2861–2869. DOI:10.1007/s11274-014-1712-2 |
| [13] | Yang Y, Ye XL, Li XG, et al. Synthesis and antimicrobial activity of 8-alkylberberine derivatives with a long aliphatic chain[J]. Planta Med, 2007, 73: 602–604. DOI:10.1055/s-2007-967180 |
| [14] | Joshi PV, Shirkhedkar AA, Prakash K, et al. Antidiarrheal activity, chemical and toxicity profile of Berberis aristata[J]. Pharm Biol, 2011, 49: 94–100. DOI:10.3109/13880209.2010.500295 |
| [15] | Fu H, Liu LG, Peng JP, et al. Transcriptional profile of the Shigella flexneri response to an alkaloid:berberine[J]. FEMS Microbiol Lett, 2010, 303: 169–175. DOI:10.1111/fml.2010.303.issue-2 |
| [16] | Li C, Xie J, Chen X, et al. Comparison of Helicobacter pylori urease inhibition by rhizoma coptidis, cortex phellodendri and berberine:mechanisms of interaction with the sulfhydryl group[J]. Planta Med, 2016, 82: 305–311. |
| [17] | Liu YX, Xiao CL, Wang YX, et al. Synthesis, structureactivity relationship and in vitro anti-mycobacterial evaluation of 13-n-octylberberine derivatives[J]. Eur J Med Chem, 2012, 52: 151–158. DOI:10.1016/j.ejmech.2012.03.012 |
| [18] | Rabbani GH, Butler T, Knight J, et al. Randomized controlled trial of berberine sulfate therapy for diarrhea due to enterotoxigenic Escherichia coli and Vibrio cholerae[J]. J Infect Dis, 1987, 155: 979–984. DOI:10.1093/infdis/155.5.979 |
| [19] | Iwazaki RS, Endo EH, Ueda-Nakamura T, et al. In vitro antifungal activity of the berberine and its synergism with fluconazole[J]. Antonie Van Leeuwenhoek, 2010, 97: 201–205. DOI:10.1007/s10482-009-9394-8 |
| [20] | Cong L, Liao Y, Yang S, et al. In vitro activity of berberine alone and in combination with antifungal drugs against planktonic forms and biofilms of Trichosporon Asahii[J]. Mycopathologia, 2017. DOI:10.1007/s11046-017-0119-7 |
| [21] | Guan KZ, Zhang WJ, Peng XQ. Effect of antibacterial activities of berberine by introduction of lipophilic aryl in its 9-position[J]. Pharmacy Today (今日药学), 2011, 21: 411–413. |
| [22] | Imanshahidi M, Hosseinzadeh H. Pharmacological and therapeutic effects of Berberis vulgaris and its active constituent, berberine[J]. Phytother Res, 2008, 22: 999–1012. DOI:10.1002/ptr.2399 |
| [23] | Yang Y, Lei ZY, Wu FP, et al. The advance on antimicrobial effect of berberine[J]. Prog Modern Biomed (现代生物医学进展), 2010, 10: 1783–1785. |
| [24] | Stermitz FR, Lorenz P, Tawara JN, et al. Synergy in a medicinal plant:antimicrobial action of berberine potentiated by 5'-methoxyhydnocarpin, a multidrug pump inhibitor[J]. Proc Natl Acad Sci U S A, 2000, 97: 1433–1437. DOI:10.1073/pnas.030540597 |
| [25] | Bae J, Lee D, Kim YK, et al. Berberine protects 6-hydroxydopamine-induced human dopaminergic neuronal cell death through the induction of heme oxygenase-1[J]. Mol Cells, 2013, 35: 151–157. DOI:10.1007/s10059-013-2298-5 |
| [26] | Krishnan P, Bastow KF. The 9-position in berberine analogs is an important determinant of DNA topoisomerase Ⅱ inhibition[J]. Anticancer Drug Des, 2000, 15: 255–264. |
| [27] | Li TK, Bathory E, LaVoie EJ, et al. Human topoisomerase Ⅰ poisoning by protoberberines:potential roles for both drugDNA and drug-enzyme interactions[J]. Biochemistry, 2000, 39: 7107–7116. DOI:10.1021/bi000171g |
| [28] | Kettmann V, Kost'alova D, Holtje HD. Human topoisomerase Ⅰ poisoning:docking protoberberines into a structure-based binding site model[J]. J Comput Aided Mol Des, 2004, 18: 785–796. DOI:10.1007/s10822-004-7878-1 |
| [29] | Das S, Kumar GS, Ray A, et al. Spectroscopic and thermodynamic studies on the binding of sanguinarine and berberine to triple and double helical DNA and RNA structures[J]. J Biomol Struct Dyn, 2003, 20: 703–714. DOI:10.1080/07391102.2003.10506887 |
| [30] | Wu LT, Tsou MF, Ho CC, et al. Berberine inhibits arylamine N-acetyltransferase activity and gene expression in Salmonella typhi[J]. Curr Microbiol, 2005, 51: 255–261. DOI:10.1007/s00284-005-4569-7 |
| [31] | Wang D, Yu L, Xiang H, et al. Global transcriptional profiles of Staphylococcus aureus treated with berberine chloride[J]. FEMS Microbiol Lett, 2008, 279: 217–225. DOI:10.1111/fml.2008.279.issue-2 |
| [32] | Domadia PN, Bhunia A, Sivaraman J, et al. Berberine targets assembly of Escherichia coli cell division protein FtsZ[J]. Biochemistry, 2008, 47: 3225–3234. DOI:10.1021/bi7018546 |
| [33] | Sun N, Chan FY, Lu YJ, et al. Rational design of berberinebased FtsZ inhibitors with broad-spectrum antibacterial activity[J]. PLoS One, 2014, 9: e97514. DOI:10.1371/journal.pone.0097514 |
| [34] | Boberek JM, Stach J, Good L. Genetic evidence for inhibition of bacterial division protein FtsZ by berberine[J]. PLoS One, 2010, 5: e13745. DOI:10.1371/journal.pone.0013745 |
| [35] | Oh KB, Oh MN, Kim JG, et al. Inhibition of sortasemediated Staphylococcus aureus adhesion to fibronectin via fibronectin-binding protein by sortase inhibitors[J]. Appl Microbiol Biotechnol, 2006, 70: 102–106. DOI:10.1007/s00253-005-0040-8 |
| [36] | Sun D, Abraham SN, Beachey EH. Influence of berberine sulfate on synthesis and expression of Pap fimbrial adhesin in uropathogenic Escherichia coli[J]. Antimicrob Agents Chemother, 1988, 32: 1274–1277. DOI:10.1128/AAC.32.8.1274 |
| [37] | Sack RB, Froehlich JL. Berberine inhibits intestinal secretory response of Vibrio cholerae and Escherichia coli enterotoxins[J]. Infect Immun, 1982, 35: 471–475. |
| [38] | Chu M, Ding R, Chu ZY, et al. Role of berberine in antibacterial as a high-affinity LPS antagonist binding to TLR4/MD-2 receptor[J]. BMC Complement Altern Med, 2014, 14: 89. DOI:10.1186/1472-6882-14-89 |
| [39] | Feng R, Shou JW, Zhao ZX, et al. Transforming berberine into its intestine-absorbable form by the gut microbiota[J]. Sci Rep, 2015, 5: 12155. DOI:10.1038/srep12155 |
| [40] | Wang Y, Shou JW, Li XY, et al. Berberine-induced bioactive metabolites of the gut microbiota improve energy metabolism[J]. Metabolism, 2017, 70: 72–84. DOI:10.1016/j.metabol.2017.02.003 |
| [41] | Wu LG, Chen M. Clinical theraputic effect on hyperlipidemia and weight reduction by berberine and oryzanol[J]. J Clin Cardiol (China) (临床心血管病杂志), 2007, 23: 576–578. |
| [42] | Zhang X, Zhao Y, Zhang M, et al. Structural changes of gut microbiota during berberine-mediated prevention of obesity and insulin resistance in high-fat diet-fed rats[J]. PLoS One, 2012, 7: e42529.. DOI:10.1371/journal.pone.0042529 |
| [43] | Lv Z, Peng G, Liu W, et al. Berberine blocks the relapse of Clostridium difficile infection in C57BL/6 mice after standard vancomycin treatment[J]. Antimicrob Agents Chemother, 2015, 59: 3726–3735. DOI:10.1128/AAC.04794-14 |
| [44] | Li CG, Yan L, Jing YY, et al. Berberine augments ATPinduced inflammasome activation in macrophages by enhancing AMPK signaling[J]. Oncotarget, 2017, 8: 95–109. |
| [45] | Zhou H, Feng L, Xu F, et al. Berberine inhibits palmitateinduced NLRP3 inflammasome activation by triggering autophagy in macrophages:a new mechanism linking berberine to insulin resistance improvement[J]. Biomed Pharmacother, 2017, 89: 864–874. DOI:10.1016/j.biopha.2017.03.003 |
| [46] | Wang H, Li K, Ma L, et al. Berberine inhibits enterovirus 71 replication by downregulating the MEK/ERK signaling pathway and autophagy[J]. Virol J, 2017, 14: 2. DOI:10.1186/s12985-016-0674-4 |
| [47] | Cheng LL, Wang M, Wu MH, et al. Interaction mechanism between berberine and the enzyme lysozyme[J]. Spectrochim Acta A Mol Biomol Spectrosc, 2012, 97: 209–214. DOI:10.1016/j.saa.2012.05.035 |
| [48] | Liu RH, Xiao Y, Chen HY, et al. Berberine hydrochloride enema application of bacterial enteritis in children[J]. Med J West China (西部医学), 2014, 36: 1635–1636. |
| [49] | Khin Maung U, Myo K, Nyunt Nyunt W, et al. Clinical trial of berberine in acute watery diarrhoea[J]. Br Med J (Clin Res Ed), 1985, 291: 1601–1605. DOI:10.1136/bmj.291.6509.1601 |
| [50] | Chen G, Xu Y, Jing J, et al. The anti-sepsis activity of the components of Huanglian Jiedu Decoction with high lipid A-binding affinity[J]. Int Immunopharmacol, 2017, 46: 87–96. DOI:10.1016/j.intimp.2017.02.025 |
| [51] | Tao MC, Xia XJ, Cao Y. In vitro anti-fungal effect of coptidis decoction for detoxification or combined with western medicine[J]. Chin Arch Tradit Chin Med (中华中医药学刊), 2009, 27: 585–587. |
| [52] | Lin YH, Lin JH, Chou SC, et al. Berberine-loaded targeted nanoparticles as specific Helicobacter pylori eradication therapy:in vitro and in vivo study[J]. Nanomedicine (Lond), 2015, 10: 57–71. DOI:10.2217/nnm.14.76 |
 2018, Vol. 53
2018, Vol. 53


