2. Putuo District Center for Disease Control and Prevention, Shanghai 200333, China;
3. Songjiang District Center for Disease Control and Prevention, Shanghai 201620, China;
4. Xuhui District Center for Disease Control and Prevention, Shanghai 200237, China;
5. Shanghai Center for Disease Control and Prevention, Shanghai 200336, China;
6. Department of Public Health Sciences, Karolinska Institutet, Stockholm 17177, Sweden
Student contacts of tuberculosis (TB) cases are susceptible to latent tuberculosis infection (LTBI), and chemo-prophylaxis can reduce the risk of active TB among them. This study aimed to assess the acceptance of chemo-prophylaxis for LTBI among students, and their concerns regarding TB and its preventive treatment. A total of 560 students contacts were included in the investigation. The extent of contact was categorized from high to low (4 levels) with 12.9% of the students being close contacts. About 87.0% of the students were willing to receive chemo-prophylaxis if diagnosed with, LTBI, whereas 73 students declined. Students with a higher level of knowledge about TB (aOR = 1.11) or close contact with TB patients (aOR = 4.30) were more likely to accept treatment. To conclude, education regarding TB transmission is necessary. Moreover, LTBI detection should be integrated into the current school-based TB contact investigation.
Latent tuberculosis infection (LTBI) is defined as a state of persistent immune response to stimulation by Mycobacterium tuberculosis (M.TB) antigens without clinical manifestations of active tuberculosis (TB)[1]; LTBI can be diagnosed by Mantoux tuberculin skin test (TST) and interferon-gamma release assay testing. The World Health Organization (WHO) reported that about one third of the world's population was infected with M.TB[2]. Though people with LTBI cannot transmit the infection, they have a 5%-15% risk of developing active TB within the first five years of being infected.
Students' clustering activities render them susceptible when there are cases of infectious TB in the school. Once diagnosed with LTBI, students are in the pool of potential TB cases. Children and adolescents with LTBI are also vulnerable to the risk of reactivation and may transmit the infection to the correspondent population. Chemo-prophylaxis for prevention of LTBI is the major strategy to eliminate TB in the US and other developed countries[3-5]. There is abundant evidence to show that early and short-term LTBI prophylaxis can decrease the risk of active TB effectively[6]. However, LTBI chemo-prophylaxis can be complicated by the side effects of the drug, poor adherence, and incomplete treatment[7].
In 2015, WHO proposed that LTBI management should be incorporated as part of the current TB control programs in countries with a lower incidence of TB (< 100/100, 000 populations)[8]. In China, LTBI chemo-prophylaxis has been suggested for children and adolescents with TST reaction induration size equal to or larger than 15 mm, and the chemo-prophylaxis regimen has been piloted in several high schools and colleges. However, the routine LTBI screening and preventive treatment in TB contact investigation in China has not been regulated so far. Faced with the growing incidence of TB outbreaks in schools, the Chinese Health Authorities are attempting to develop national strategies for chemo-prophylaxis among student contacts with LTBI.
Understanding the acceptance of LTBI chemo-prophylaxis, and identifying the factors influencing it would be helpful in developing strategies for school-based LTBI management in China. In this study, a cross-sectional investigation was conducted among students who had been in contact with infectious TB patients in schools, in Shanghai, China. This study aimed to assess the level of knowledge of student contacts about TB, their willingness to participate in the LTBI chemo-prophylaxis if diagnosed with LTBI after the contact, and their concerns associated with the acceptance of LTBI treatment.
Our research was a cross-sectional study carried out among student contacts of infectious TB cases in three districts of Shanghai. From May 2016 to February 2017, 14 students from six high schools (including both general high schools and vocational-technical schools) and three colleges were diagnosed with active TB. As regulated by the Shanghai school-based TB management guidelines, students contacts of the index cases underwent screening in the form of symptom inquiries and/or chest radiographic examination provided by the district center for disease control and prevention (CDC). During the investigation, the student contacts were also requested to complete a questionnaire on their level of knowledge regarding TB and contact information. Following this, the students received education and individual counseling about LTBI, including the risk of progression from LTBI to active TB, merits of LTBI chemo-prophylaxis, treatment duration and possible side effects. Willingness of the students to accept chemo-prophylaxis for LTBI was then assessed.
Information on the demographics, type of school, and contact history was collected through routine investigation. Core TB knowledge was assessed based on the responses to eight questions on China's national TB control program. Acceptance of LTBI chemo-prophylaxis was further investigated through another self-completed questionnaire afterward. Participation in the study was voluntary and anonymous, with student data confidentiality assured. Ethical clearance was obtained from the School of Public Health, Fudan University, Shanghai, China.
Based on the contact history with the index student TB patients, contact scales were defined as follows: close contact (roommates and/or friends with close communication), routine contact (classmates sharing the same classroom or computer-room), casual contact (students from the neighboring classrooms or dormitories), and rare contact (not satisfying any of the above categories but having a dormitory on the same floor).
For the eight questions assessing the level of knowledge regard TB, each correct answer was awarded one point. Analysis of variance (ANOVA) was used for continuous variables, while the Chi-square test was applied to categorical variables. Adjusted odds ratio (aOR) and 95% confidence interval (CI) were obtained by logistic regression analysis after adjusting for gender, resident status, and the type of school. The significant level (α) was set at 0.05. Data analysis was performed using SPSS v.19.0 (IBM, USA) and SAS v.9.3 packages (SAS Institute, Cary, North Carolina).
In total, 560 high school/college students were categorized as contacts of the 14 TB index cases. Amongst these student contacts, 460 (82.1%) and 170 (30.4%) underwent TB symptom inquiry and chest radiographic examination, respecting. No case of active TB was detected. The average age of the student contacts was 17.9 years (range, 15-26 years), and 57.7% of the student contacts were local residents (Supplementary Table 1, available in www.besjournal.com). Boys accounted for 66.8% of the contacts. About 78.6% of the contacts were high school students. Approximately 12.9% of these students were close contacts of the index cases; 40.6% were routine contacts, and the rest were casual contacts (25.4%) and rare contacts (21.1%).
|
|
Supplementary Table 1 Demographic Factors of the Student TB Contacts |
The students' responses to questions related to knowledge and attitude toward TB are presented in Table 1. Among the close contacts, only 43 (59.7%) students were aware of the main symptoms of TB; this number was significantly lower than in other groups. Less than half the students were aware that contact with TB patients increases the risk of contracting TB. Only 25.0% (n = 140) had heard of the free treatment policy for TB under the national TB control program. The average score for the level of knowledge about TB was 5.03 points with a standard deviation (SD) of 2.15. Only 8.2% (n = 46) of the student contacts scored 8 points. Students in the casual contact group presented a lower knowledge score 4.69 ± 2.21 compared to the others. About 54.1% of the students thought that they should avoid contact with TB patients. There were 160 students (28.6%) with the view that they could maintain contact with TB patients as usual, and this proportion was significantly higher among students in the close and routine contact groups (P = 0.011).
|
|
Table 1 Responses to Questions Related to Knowledge and Attitude toward TB among Student Contacts Categorized by the Extent of Contact |
Of the 560 student contacts, 487 (87.0%) agreed to receive chemo-prophylaxis if diagnosed with LTBI. The three most frequently reported reasons for willingness to receive LTBI prophylaxis were: preventing active TB (67.1%); concerns about spreading it to other students in case of reactivation (49.5%); and consistent contact with TB patients (40.7%). However, there were still 73 students who declined chemo-prophylaxis believing the risk of active TB to be low, and claiming unobservable effects of LTBI prophylaxis and lack of time for treatment (Table 2).
|
|
Table 2 Main Reasons for Acceptance/Refusal of Chemo-prophylaxis for LTBI |
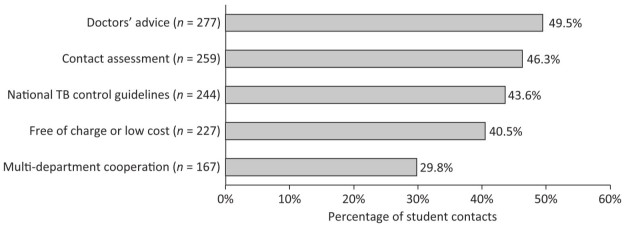
Multivariate analysis revealed that the acceptance of LTBI chemo-prophylaxis was significantly associated with higher level of TB knowledge (Table 3). Students with better knowledge of TB transmission and treatment were more likely to accept chemo-prophylaxis (aOR = 1.89, aOR = 2.82). Likewise, students with a higher score were also more likely to receive LTBI treatment (aOR = 1.11). A positive association was also observed between the extent of contact and acceptance of prophylaxis. Close contacts were more likely to accept chemo-prophylaxis for LTBI compared to those in the rare contact group (aOR = 4.30). Additionally, about 80% of the student contacts approved of the idea of providing chemo-prophylaxis for LTBI in schools. Elements influencing the students' view included doctors' advice (49.5%), contact assessment (46.3%), regulations in the national TB control guidelines (43.6%), free or low cost (40.5%), as well as cooperation between the education and health departments (29.8%). (Supplementary Figure 1, available in www.besjournal.com)
|
|
Table 3 Multivariate Analysis of Factors Influencing Acceptance of LTBI Chemo-prophylaxis |
|
Download:
|
| Supplementary Figure 1 Key components for providing LTBI chemo-prophylaxis in schools. | |
In this study, we found that students who had close contact with TB patients were more likely to accept LTBI prophylaxis, indicating that LTBI health education, screening, and prophylaxis should be prioritized in these contacts, if diagnosed. Consistent with the results of other studies in China[9], knowledge of TB among student contacts in the present study was not well disseminated. Less than half of students were aware that contact with pulmonary TB patients increased the risk of TB infection. It was also observed that students with a lower TB knowledge score were less likely to accept LTBI chemo-prophylaxis. These results suggest that health education on TB transmission and self-protection should be provided especially to close-contact students, which could improve student awareness of both the risk of TB infection and preventive and treatment solutions.
Many students who declined LTBI prophylaxis were concerned about its unobservable long-term effects, possible side effects, and prolonged treatment duration, which emphasizes the importance of integrating the latest evidence of the effectiveness of the therapeutic regimen into LTBI health education. A cohort study reported that the incidence of gastrointestinal and hepatic side effects in isoniazid (INH) prophylaxis were 21% and 5%, with a lower risk in younger patients[10]. Nikos suggested that an alternative therapy with 3-4 months of isoniazid and rifampicin (INH-RFP) had fewer severe adverse events and better adherence in children with LTBI than 9 months of INH monotherapy[11]. Given that many students believe themselves to be at low risk for active TB, risk evaluation and subsequent LTBI detection should be provided by health-care providers to identify those at high risk for LTBI. In addition, the accessibility of LTBI chemo-prophylaxis also had an influence on students' acceptance, which means that cooperation between the education and health departments should be intensified to provide feasible, accessible, and affordable LTBI treatment.
In China, the current school-based TB control strategy prioritizes detection of active TB cases through symptom inquiry and chest radiographic examination; however, the detection and management of LTBI is neglected to some extent. Lack of screening and prophylaxis for LTBI might increase the incidence of TB infection in schools. According to China's national TB surveillance in 2012, the incidence of active TB among students was 16.63/100, 000[12]. To stem the increasing TB epidemics in schools, management of LTBI should be integrated into the current TB contact investigation strategy, especially among student contacts. In the process of strengthening school-based LTBI management, technical guidelines should be established to create a conducive policy. Health-care providers from the CDC should provide tailored TB health education and risk evaluation during the contact investigation in schools. Once LTBI prophylaxis is initiated, health-care providers and teachers should regularly monitor the potential side effects and ensure adherence to treatment.
The authors declare no conflict of interest.
| 1. | Mack U, Migliori GB, Sester M, et al. LTBI: latent tuberculosis infection or lasting immune responses to M. tuberculosis?A TBNET consensus statement. Eur Respir J, 2009, 33: 956. doi:10.1183/09031936.00120908 |
| 2. | Dye C, Scheele S, Dolin P, et al. Global Burden of Tuberculosis: Estimated Incidence, Prevalence, and Mortality by Country. JAMA, 1999, 282: 1189–210. |
| 3. | Hirsch-Moverman Y, Daftary A, Franks J, et al. Adherence to treatment for latent tuberculosis infection: systematic review of studies in the US and Canada. Int J Tuberclung D, 2009, 12: 1235. |
| 4. | Chee CB, Teleman MD, Boudville IC, et al. Treatment of latent TB infection for close contacts as a complementary TB control strategy in Singapore. Int J Tuberclung D, 2004, 8: 226–31. |
| 5. | Denholm JT, Mcbryde ES. Management of Latent Tuberculosis Infections in Australia and New Zealand: A Review of Current Practice. Tuberc Res Treat, 2010, 2010. |
| 6. | Stagg HR, Zenner D, Harris RJ, et al. Treatment of latent tuberculosis infection: a network meta-analysis. AM J Resp Crit Care, 2014, 162: 394–5. |
| 7. | Cass AD, Talawera GA, Gresham LS, et al. Structured behavioral intervention to increase children's adherence to treatment for latent tuberculosis infection. Int J Tuberclung D, 2005, 9: 415. |
| 8. | World Health Organization. Guidelines on the management of latent tuberculosis infection. http://www.who.int/tb/publications/latent-tuberculosis-infection/en/ [2017/2/20] |
| 9. | Zhao Y, Ehiri J, Li D, et al. A survey of TB knowledge among medical students in Southwest China: is the information reaching the target?. BMJ Open, 2013, 3. |
| 10. | Denholm JT, Mcbryde ES, Eisen DP, et al. Adverse effects of isoniazid preventative therapy for latent tuberculosis infection: a prospective cohort study. Drug Healthc Patient Saf, 2014, 6: 145. |
| 11. | Spyridis NP, Spyridis PG, Gelesme A, et al. The Effectiveness of a 9-Month Regimen of Isoniazid Alone versus 3- and 4-Month Regimens of Isoniazid plus Rifampin for Treatment of Latent Tuberculosis Infection in Children: Results of an 11-Year Randomized Study. Clin Infect Dis, 2007, 45: 715–22. doi:10.1086/520983 |
| 12. | Spyridis NP, Spyridis PG, Gelesme A, et al. The Effectiveness of a 9-Month Regimen of Isoniazid Alone versus 3- and 4-Month Regimens of Isoniazid plus Rifampin for Treatment of Latent Tuberculosis Infection in Children: Results of an 11-Year Randomized Study. Clin Infect Dis, 2007, 45: 715–22. doi:10.1086/520983 |
 2018, Vol. 31
2018, Vol. 31


