2. The First Affiliated Hospital, Zhejiang University, Hangzhou 310003, Zhejiang, China;
3. Zhejiang International Travel Healthcare Center, Hangzhou 310009, Zhejiang, China;
4. The Second Affiliated Hospital, Zhejiang University, Hangzhou 310009, Zhejiang, China
Emergencies of epistaxis in students caused by environmental pollution have rarely been reported to date. This study aimed to explore the cause of an emergency of epistaxis in elementary students by using a field epidemiological investigation. Twenty-two epistaxis cases from a single school with differences in gender, age, and classroom, were diagnosed within a period of 7 days. The air concentration of chromic acid mist (Cr6+) in the electroplating factory area, new campus, and residential area exceeded the limit of uncontrolled emissions. The emission of HCL and H2SO4was also observed. Formaldehyde levels in the classrooms exceeded the limits of indoor air quality. Abnormal nasal mucosa was significantly more frequent in the case group (93.3%) and control group 1 (of the same school) (66.7%) than in control group 2 (from a mountainous area with no industrial zone) (34.8%; P < 0.05 and P < 0.01, respectively). On the basis of the pre-existing local nasal mucosal lesions, excessive chromic acid mist in the school's surrounding areas and formaldehyde in the classrooms were considered to have acutely irritated the nasal mucosa, causing epistaxis. Several lessons regarding factory site selection, eradication of chemical emissions, and indoor air quality in newly decorated classrooms, should be learned from this emergency.
Epistaxis is defined as an acute hemorrhage from the nostril, nasal cavity, or nasopharynx. Although the vast majority of patients who present to the emergency department (ED) with epistaxis may be successfully treated, it often causes significant anxiety in patients and their family members[1]. An emergent event of epistaxis among many students may draw wide public attention, which presents a challenge for local government to deal with the public events appropriately.
In addition to trauma, infections, and tumors, which are the most common known factors, chemical irritants in indoor or outdoor air pollution may be a factor in the differential diagnosis of epistaxis[2]. A study by Szyszkowicz et al. suggested that an association exists between air pollution exposure and ED visits for epistaxis[3]. In terms of indoor air pollution, a study by Wantke et al. indicated that exposure to gaseous formaldehyde could induce IgE-mediated sensitization to formaldehyde in school-age children at the age of 8 years[4]. The report also suggested that many clinical symptoms among affected children, such as epistaxis, headache, and rhinitis, were associated with the formaldehyde concentrations in classrooms. In the occupational setting, nasal septum lesions induced by chromium exposure area type of occupational disease. Chromium electroplating workers usually suffer from epistaxis during work due to nasal septum perforation[5-6].
Epistaxis is common among children and young adults. A retrospective review of 101 patients seen with epistaxis in hospitals showed that modal age presentations for epistaxis were recorded among 1-20-years-old (40.6%, with 1-10 years accounting for over 20%)[7]. The predilection site of epistaxis in children usually locates at the anterior part of the nasal septum. The most common cause of epistaxis in adolescents is angiectasis or erosion of the nasal mucosa in Little's region of the nasal septum[8].
Although children are susceptible to epistaxis, an outbreak of many epistaxis cases among school students, which might be associated with environmental pollution, has rarely been reported. In this report, multiple methods, including field epidemiological investigation, air monitoring, and a case-control study, were used to explore the cause of the event, to provide a scientific basis for the local government to deal with the emergency.
On September 3, 2013, an elementary school in a town of Zhejiang Province, East China, moved to a new location. Within the first week of classes, 22 students suffered different degrees of epistaxis. The event drew wide public attention because of the large number of epistaxis cases and the fact that epistaxis was observed immediately after the move to a new campus. The elementary school was located in a rural community with developed township enterprises. There were 27 classes and 1211 students from Grade 1 to Grade 6. The classrooms of the new campus were newly decorated with various materials.
Thirty-one factories were located within a 1-km radius around the school. Among them, 27 factories were involved in potential emission of air pollutants. Their layout is illustrated in Supplemental Figure 1 (see the website:www.besjournal.com). These included two electroplating factories, one chemical factory, three heat-treatment processing enterprises, and two aluminum die-casting enterprises. The production processes in the two electroplating factories included degreasing, pickling, and plating (chromium, copper, and nickel) processes. The main hazardous chemicals from the production processes were sulfuric acid, hydrogen chloride, and hexavalent chromium. The prevailing wind direction of the local area was northeasterly. The new campuses may have been affected by noxious gases throughout the year.
|
Download:
|
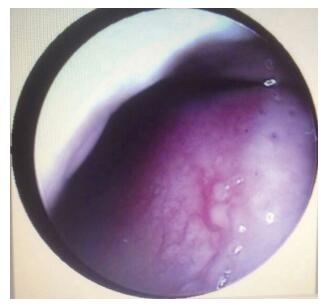
| Figure 1 Image of angiectasis and mucosa erosions in the Little's region obtained by using nasal endoscopy. | |
On September 6, the local environmental department conducted tests for sulfuric acid, chromic acid mist, hydrogen chloride, benzene, toluene, and xylene around one of the electroplating factories (the one located closest to the school), as well as at sites around the school. These environmental pollutants were determined on the basis of their corresponding criteria in China. Of the 16 classrooms in which students experienced epistaxis, 8 classrooms were randomly selected as sampling locations for formaldehyde, benzene, toluene, and xylene. These chemicals were determined on the basis of the standard in China (GB/T 18883-2002 'Indoor Air Quality Standard').
Fifteen students who had experienced epistaxis were selected as the case group, and another 18 students from the same school who did not experience epistaxis were selected as control group 1. Sixty-six students from a school located in a mountainous area with no industrial zone were selected as control group 2. The average ages and gender compositions of the two control groups were not significantly different from those of the case group (P > 0.05). All study participants provided informed consent. All subjects underwent nasoscopy and nasal endoscopy. Abnormal nasal mucosa was defined by the presence of Little's region angiectasis, nasal mucosa erosions, and rhinitis.
One-way analysis of variance with the least significant difference post-hoc test (equal variances) was used to analyze the differences in average age among the three groups. A chi-square test was applied to analyze the differences in the percentages of abnormal nasal mucosa and other confounding factors in the three groups.
Detailed epidemiological characteristics of the 22 students with epistaxis are as follows: (1) population distribution: 15 male and 7 female students aged 7 to 12 years; (2) time distribution: from September 3 to 9 (4 cases on September 3, 3 cases on September 4, 10 cases on September 5, 1 case on September 6, and 4 cases on September 9); (3) class distribution: 16 classes from Grade 1 to Grade 6; (4) clinical manifestations: one student experienced epistaxis ≥ 4 times, 2 experienced it 3 times, 6 experienced it twice, and 13 experienced it once. Nine students had a history of rhinitis, and 13 were aware of an abnormal smell in the classroom. In addition to epistaxis, subjects showed different degrees of accompanying symptoms, such as dizziness, headache, cough, or a sore throat. Epistaxis was not observed after the students left school and returned home to rest.
Table 1 shows that the levels of chromic acid mist around the electroplating factory area, the area of painted steel frame piles on the new campus, and the local community area were beyond the concentration limits of uncontrolled emissions as specified in China's GB16297-1996 'Integrated emission standard of air pollutants.' Hydrogen chloride and sulfuric acid were also detected, but these levels were not very high. Benzene, toluene, and xylene were not detected at the above sampling locations around the electroplating factory, new campus, or residential area. Table 2 shows that formaldehyde levels at all sampling locations in the classrooms of the new campus exceeded the limits specified in China's GB/T 18883-2002 'Indoor Air Quality Standard, ' whereas benzene, toluene, and xylene were not detected in the classrooms of the new campus.
|
|
Table 1 Air monitoring for chemicals around the factory, new campus and residential area |
|
|
Table 2 Formaldehyde levels in the classrooms of the new campus |
Supplemental Table 1 (see the website: www.besjournal.com) shows that abnormal nasal mucosa was significantly more frequent in the case group and control group 1 than in control group 2 (P < 0.05 or P < 0.01). Abnormal nasal mucosa cases were more frequent in the case group than in control group 1, but this difference was not statistically significant. To rule out the effects of blood diseases, chronic chromium poisoning, and nose picking habits on epistaxis, routine blood examinations and urine chromium tests were performed for all subjects, and their nose picking habits were investigated. There were no significant differences in routine blood indexes (white blood cell count, hemoglobin level, platelet count, prothrombin time, and endogenous thrombin) or the proportion of students with a nose picking habit between the case group and two control groups (P > 0.05). Hexavalent chromium was not detected in the subjects' urine samples.
According to epidemiological data obtained from the 22 epistaxis patients, the gender, age, classroom, and grade varied, although all cases occurred within the same school during a period of 7 days. The similarity of clinical manifestations indicated that the patients had a common exposure history or homology. These lines of evidence, such as the aggregation of cases within the same time frame and in the same space and clinical manifestations with no fever, could rule out the possibility of infectious diseases. Hence, the event might be initially considered a poisoning emergency.
Evidence from field epidemiology and clinical and laboratory examinations was used to investigate the cause of this poisoning incident. The two electroplating businesses near the school were found to have uncontrolled emissions of chromic acid mist, sulfuric acid, and hydrochloric acid from their production processes. The excessive level of chromic acid mist was detected in the air of the electroplating factory area, the local community area, and the new campus. The school was located downwind at the time of the event, which increased the severity of chromic acid mist pollution in the school. Since the classrooms in the new campus had been newly renovated, air levels of formaldehyde in the classrooms were also very high, which indicated that the students were also exposed to severe formaldehyde pollution. Taken together, the evidence indicated that the poisoning incident might be associated with air pollution of chromic acid mist and formaldehyde, with respiratory inhalation being the means of exposure.
According to the clinical evidence, abnormal nasal mucosa in Little's region was significantly more common in the case group and control group 1 (including students exposed to indoor and outdoor environmental pollution) than in control group 2 (including students not exposed to environmental pollution). Figure 1 shows an example of angiectasis and mucosa erosions in the Little's region observed by using nasal endoscopy. The nasal lesions in all cases were located in the anterior part of nasal fossa. These results indicated that the majority of students in this school (including those who did not experience epistaxis) were suffering from chronic nasal mucosa lesions, such as angiectasis, nasal mucosa erosions, and rhinitis. Long-term exposure to an unfavorable air environment could result in local lesions in many students. Local irritation by chemicals could cause vascular rupture and bleeding. Aerosols, such as chromic acid mist and formaldehyde, have been found to have an irritating effect on the nasal mucosa[9-10]and to cause acute nasal mucosal bleeding at high concentrations. In the event reported here, high concentrations of formaldehyde in the classroom environment and chromic acid mist in the indoor and outdoor environment of the school may have caused an acute irritation of nasal mucosa in the students, possibly inducing an acute episode of pre-existing chronic lesions of the nasal mucosa in Little's region and causing epistaxis. Students who experienced epistaxis did not have epistaxis again after leaving school for a while and being away from exposure to chromic acid mist and formaldehyde, corroborating evidence that epistaxis is associated with acute irritation by these environmental pollutants.
In addition to nasal cavity disease, systemic diseases, such as bleeding disorders, platelet count or functional disorders, clotting factor disorders, and acute febrile diseases, are also causes of epistaxis[11]. In this report, systemic causes could be ruled out because there were no differences in blood routine indexes between the case group and control group 2. In addition, the effect of some behavioral factors on epistaxis, for example, nose picking[12], in this incident was ruled out because there was no significant difference in the proportion of students with a nose picking habit between the case group and the control groups[2]. Moreover, viral infection could be ruled out on the basis of the results of nasal endoscopies and routine blood examination. Nasal endoscopies showed that the local nasal lesions were limited in the Little's region, which was different from the characteristics of acute viral infection with a wide range of hyperemia. A routine blood examination also failed to reveal some characteristics of acute viral infection, such as abnormal lymphocyte counts.
Taken together, evidence in the form of field, patient, and laboratory tests suggested that the emergency of epistaxis in school students was attributable to acute irritation of the nasal mucosa by the excessive chromic acid mist in the school's surrounding areas and formaldehyde in the classroom environment of the new campus, based on the pre-existing local mucosal lesions. The lessons from this epistaxis event caused by environmental pollutants in elementary school students were as follows: (1) Factories with potential environmental pollution hazards needed to consider a sufficient distance from local susceptible populations; (2) Anti-pollution measures in factories should be taken to eradicate emissions of hazardous substances; and (3) Newly renovated classrooms should only be used when their air quality meets the standard.
| 1. | Kodiya AM, Labaran AS, Musa E, et al. Epistaxis in Kaduna, Nigeria:a review of 101 cases[J]. Afr Health Sci , 2012, 12 :479–82. |
| 2. | Iseh KR, Muhammad Z. Pattern of epistaxis in Sokoto, Nigeria:a review of 72 cases[J]. Ann Afr Med , 2008, 7 :107–11. doi:10.4103/1596-3519.55668 |
| 3. | Szyszkowicz M, Shutt R, Kousha T, et al. Air pollution and emergency department visits for epistaxis[J]. Clin Otolaryngol , 2014, 39 :345–51. doi:10.1111/coa.2014.39.issue-6 |
| 4. | Wantke F, Demmer CM, Tappler P, et al. Exposure to gaseous formaldehyde induces IgE-mediated sensitization to formaldehyde in school-children[J]. Clin Exp Allergy , 1996, 26 :276–80. doi:10.1111/cea.1996.26.issue-3 |
| 5. | Lin SC, Tai CC, Chan CC, et al. Nasal septum lesions caused by chromium exposure among chromium electroplating workers[J]. Am J Ind Med , 1994, 26 :221–8. doi:10.1002/(ISSN)1097-0274 |
| 6. | Yang Y, Liu H, Xiang XH, et al. Outline of occupational chromium poisoning in China[J]. Bull Environ Contam Toxicol , 2013, 90 :742–9. doi:10.1007/s00128-013-0998-3 |
| 7. | Kodiya AM, Labaran AS, Musa E, et al. Epistaxis in Kaduna, Nigeria:a review of 101 cases[J]. Afr Health Sci , 2012, 12 :479–82. |
| 8. | Felek SA, Celik H, Islam A, et al. Bilateral simultaneous nasal septal cauterization in children with recurrent epistaxis[J]. Int J Pediatr Otorhinolaryngol , 2009, 73 :1390–3. doi:10.1016/j.ijporl.2009.06.023 |
| 9. | Zhai L, Zhao J, Xu B, et al. Influence of indoor formaldehyde pollution on respiratory system health in the urban area of Shenyang, China[J]. Afr Health Sci , 2013, 13 :137–43. |
| 10. | Aiyer RG, Kumar G. Nasal manifestations in chromium industry workers[J]. Indian J Otolaryngol Head Neck Surg , 2003, 55 :71–3. |
| 11. | Middleton PM. Epistaxis[J]. Emerg Med Australas , 2004, 16 :428–40. doi:10.1111/emm.2004.16.issue-5-6 |
| 12. | McDonald TJ. Nosebleed in children. Background and techniques to stop the flow[J]. Postgrad Med , 1987, 81 :217–24. |
 2016, Vol. 29
2016, Vol. 29

