2. Department of Obstetrics and Gynaecology, Chinese PLA General Hospital, Beijing 100853, China
Objective This study was designed to determine the prevalence of oncogenic human papillomavirus (HPV) in cervical infections in Beijing, China, and to investigate the odds ratio (OR) of HPV single and multiple infections in abnormal cytology.
Methods A total of 19,018 specimens from outpatients in the department of obstetric and gynecology were collected. They were detected using high-risk HPV genotyping real-time polymerase chain reaction (PCR) kit and analyzed by ThinPrep cytology test for cervical pathological diagnosis. HPV prevalence, age-specific prevalence, and OR of each type of HPV in abnormal cytology were analyzed.
Results Overall, 19.1% (3,623/19,018) of the individuals were positive for HPV infection, 14.9% (2,833/19,018) were positive for a single HPV type, and 4.2% (790/19,018) were positive for multiple types. Among the 3,623 HPV-positive individuals, the most predominant HPV types were HPV52 (4.4%, 834/19,018), HPV16 (3.7%, 710/19,018), and HPV58 (3.4%, 644/19,018). The OR of multiple infections and single infection differed significantly among disease severities. The OR of dual infection was higher than that of each of the two single infection types, respectively.
Conclusion HPV prevalence in the outpatients was 19.1%, and the most predominant HPV types in the study were HPV52, HPV16, and HPV58. Women with multiple infectionswere more likely to have abnormal cytology.
Cervical cancer (CC) is the second most common malignant disease and a leading cause of cancer mortality among women worldwide[1]. The causal link between human papillomavirus (HPV) infection and CC is now established beyond doubt. HPVs are small DNA viruses having a circular double-stranded DNA genome of approximately 8 kb,and they are classified on the basis of their genome DNA sequence. An HPV type has <90% similarity with other types at the nucleotide level[2-3].
Based on their association with CC and precursor lesions,HPVs can be grouped into high-risk,possible high-risk,and low-risk HPV types[4]. The high-risk HPV (HR-HPV) infection accounts for 43%-53% of patients with cervical intraepithelial neoplasia (CIN) in the western population[5-6]. HPV screening is strongly advised because of the important role of HPV in the development of CC and other associated diseases and its greater sensitivity and cost-effectiveness in detecting CC. Screening for HR-HPV may reduce the risk for CC. HPV16 and HPV18 are two predominant prevalent types associated with CC in western countries[7]. HPV prevalence data of some regions of China suggest that the distribution of HPV types is different in China[8-11].
Cervical coinfection with more than one HPV genotype is common. Nonetheless,it is unclear whether any two HPV types are more or less likely to be involved in a coinfection. The role played by coinfections with multiple HPV types in cervical neoplasia remains a difficult area of investigation. Some studies have shown that the risk for cervical precancerous lesions or invasive cancer in women infected with multiple HPV types is no greater than that in those with single-type infections,while some studies have shown that infection with multiple HPV types appears to act synergistically in cervical carcinogenesis[12-15]. With the increasing administration of HPV prophylactic vaccines,the mechanism behind multiple-type infections warrants further investigation,in light of the concern for HPV type replacement.
The purpose of this study was to investigate the prevalence of HR-HPVs and the frequency of single and multiple infections and to investigate the different risk of cervical lesion severity between HPV single and multiple infections. The interaction between different phylogenetic species in dual infection was also analyzed to assess the presence of any biological interactions between species that contribute to multiple-type infections.
MATERIALS AND METHODS SubjectsA total of 19,018 patients were studied from January 2013 to July 2014 in the department of obstetric and gynecology at the Chinese PLA General Hospital in Beijing. All the 19,018 patients underwent high-risk HPV DNA quantitative measurement and biopsy. Among them,17,790 individuals were diagnosed as normal,959 patients were diagnosed with atypical squamous cells of undetermined significance (ASCUS),93 patients were diagnosed with low-grade squamous intraepithelial lesion (LSIL),and 176 patients were diagnosed with high-grade squamous intraepithelial lesion (HSIL).
Pathological ExaminationCervical cytology was carried out by ThinPrep cytology test (TCT). Cytological diagnosis was made according to the Bethesda system classification. Histological diagnosis of the cervix was made according to the criteria proposed by the 7th edition of ‘Obstetrics and Gynecology’. The biopsy of pathological sections was reviewed by senior physicians.
HPV Detection and GenotypingDNA extraction and HPV genotyping were carried out using high-risk HPV genotyping real-time PCR kit (Shanghai ZJ Bio-Tech Co.,Ltd) to detect the following HPV types: HPV 16,18,31,33,35,39,45,51,52,56,58,59,and [68] The lowest detection limit of the kit was 1×104 copies/mL. Amplification techniques performed on SLAN®-96P (Shanghai Hongshi Medical Technology Co.,Ltd) were used for the quantitative estimation of HPV DNA copies.
Statistical AnalysisAll statistical analyses were performed using SPSS statistical software version 19.0. The data were stratified by age (≤20 years,21-25 years,26-30 years,31-35 years,36-40 years,41-45 years,46-50 years,51-55 years,56-60 years,and ≥61 years). Chi-squared analyses were used for bivariate comparisons between age groups. P<0.05 was considered as statistically significant. Logistic regression was used to estimate the odds ratio (OR) with 95% confidence intervals to examine the association between HPV infection and CIN risk.
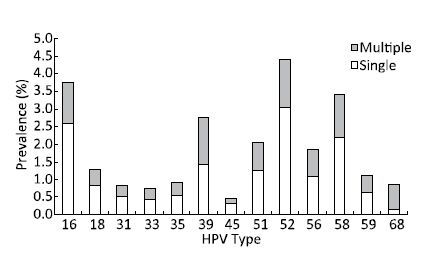
RESULTS Prevalence of the Oncogenic Genotypes in the Cervical SamplesReal-time PCR quantification assays were used to investigate the frequency of type-specific HPV infection. Among the 19,018 patients,positive HPV test were obtained in 3,623 (19.1%,3,623/19,018) patients,of whom 2,833 (14.9%,2,833/19,018) were positive for a single HPV type and 790 (4.2%,790/19,018) were positive for multiple types (Figure 1).
|
Download:
|
| Figure 1 Prevalence of the 13 oncogenic HR-HPVs. | |
Overall,HPV52 had the highest prevalence (4.4%,834/19,018),followed by HPV16 (3.7%,710/19,018),HPV58 (3.4%,644/19,018),HPV39 (2.7%,518/19,018),and HPV51 (2.0%,387/19,018). HPV18 had a prevalence of 1.3% (241/19,018) and was ranked seventh. In the 2,833 patients infected with single infection,the three most prevalence types were HPV52 (3.0%,576/19,018),HPV16 (2.6%,491/19,018),and HPV58 (2.2%,416/19,018). In the 790 patients infected with multiple infections,the three most prevalence types were HPV52 (1.4%,258/19,018),HPV39 (1.3%,253/19,018),and HPV58 (1.2%,228/19,018) (Figure 1). Among the multiple infections,632 (80.0%,632/790) had dual infections,125 (15.8%,125/790) had triple infections,29 (3.7%,29/790) had fourfold infections,and 4 (0.5%,4/790) had fivefold infections.
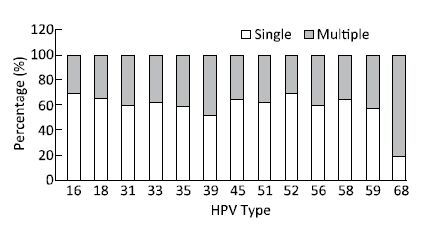
The percentages of the single and multiple infections of each of the 13 typesare shown in Figure 2. Among the 13 oncogenic HPV types,HPV16 (69.2%,491/710),HPV52 (69.1%,576/834),and HPV18 (65.1%,157/241) constituted the highest proportion of single infections and HPV68 (82.1%,133/162),HPV39 (48.8%,253/518),and HPV59 (42.9%,90/210) constituted the highest proportion of multiple infections. HPV68,HPV39,and HPV59 belonged to Alpha genus seventh species (A7).
|
Download:
|
| Figure 2 Single and multiple infection constituent ratios of each of the 13 oncogenic HPV types. | |
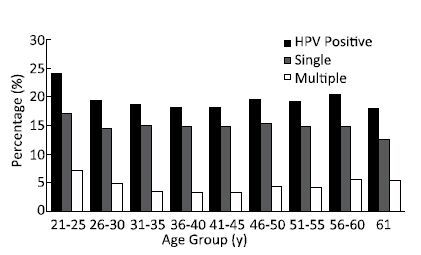
The prevalence of HPV infection was significantly different among the different age groups (χ2=20.542,P=0.00847),ranging from 17.8% (171/961) in women aged ≥61 years to 24.1% (210/872) in women aged 21-25 years. Two peaks were observed for the prevalence of HPV infection,one for the group of women aged 21-25 years and the other for the group of women aged 56-60 years (20.3%,196/967) (Figure 3). (The number of samples in the 20-year-old age group was too small for the analysis) .
|
Download:
|
| Figure 3 Age-specific prevalence of HPV infection. | |
The prevalence of single HPV infection was not significantly different among the different age groups (χ2=8.3016,P=0.4046),ranging from 12.5% (120/961) in women aged ≥61 years to 17.1% (149/872) in women aged 21-25 years (Figure 3).
The prevalence of multiple HPV infections was significantly different among the different age groups (χ2=42.726,P=9.894×10-7),ranging from 3.3% in women aged 36-40 years (102/2,529) and 41-45 years (109/2,746) to 7.0% (61/872) in women aged 21-25 years. Two peaks were observed for the prevalence of HPV infection,one for the group of women aged 21-25 years and the other for the group of women aged 56-60 years (5.5%,53/967) (Figure 3).
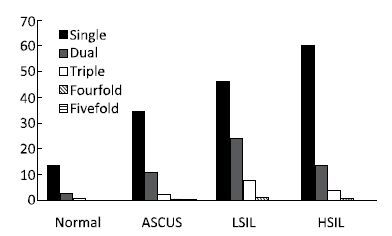
Prevalence of HPV Infection in Different Cytological DiagnosesThe prevalence of HPV infections was significantly different among the different disease categories. The prevalence rates were 16.6% (2,946/17,790) in normal individuals,48.6% (466/959) in patients with ASCUS,78.5% (73/93) in patients with LSIL,and 78.4% (138/176) in patients with HSIL.
The prevalence rates of single HPV infection were 13.2% (2,351/17,790) in normal individuals,34.7% (333/959) in patients with ASCUS,46.2% (43/93) in patients with LSIL,and 60.2% (106/176) in patients with HSIL. Thecytological diagnosis showed an increasing trend in the single HPV infection.
The prevalence rates of multiple HPV infectionswere 3.3% (595/17,790) in normal individuals,13.9% (133/959) in patients with ASCUS,32.3% (30/93) in patients with LSIL,and 18.2% (32/176) in patients with HSIL. The prevalence of dual infections ranged from 2.7% (480/17,790) in normal individuals to 23.7% (22/93) in patients with LSIL. The prevalence of triple infections ranged from 0.5% (89/17,790) in normal individuals to 7.5% (7/93) in patients with LSIL.
The prevalence rates of HPV infection in normal individuals and in patients with LSIL and HSIL were shown in Figure 4.
|
Download:
|
| Figure 4 Prevalence of HPV infection in different cytology categories. | |
The risk of HPV infection and cervical lesions was investigated. Overall,the OR ranged from 4.76 (4.22-5.38) in ASCUS to 18.39 (12.85-26.33) in LSIL; HSIL showed an OR of 18.3 (14.07-23.81). OR showed an increasing trend in the single HPV infection,ranging from 4.26 (3.73-4.88) in ASCUS to 13.57 (9.02-20.43) in LSIL and to 17.61 (13.39-23.16) in HSIL. The OR of multiple infections ranged from 6.73 (5.61-8.08) in ASCUS to 37.42 (26.31-53.24) in LSIL; HSIL showed an OR of 21.01 (15.01-29.41).
In comparison to single infection,ORs in the multiple infections were 1.58 (1.27-1.96) in ASCUS,2.76 (1.75-4.35) in LSIL,and 1.19 (0.80-1.79) in HSIL. In comparison to single infection,ORs in both dual infections and triple infections were all greater than 1. In general,multiple infections had a higher OR than that of single infection in all the categories,triple infections had a higher OR than that of dual infections in all the categories,and dual infection had a higher OR than that of single infection.
Incomparison to single infection,ORs of multiple infections of each of the oncogenic types were almost greater than that of single infection,except HPV16.When HPV16 alone was analyzed,women with single infection were more likely to have abnormal cytology with the highest OR associated with HSIL [70.60 (56.29-88.54)] in single infection than in multiple infections [56.17 (41.32-76.36)] (Table 1).
|
|
Table 1 Dual infections in different cervical disease categories |
Among the 632 dual-infection individuals,the most predominant types were HPV39 (30.2%,191/632),HPV52 (27.8%,176/632),and HPV58 (25.5%,161/632). At the type level,A5 (HPV51) accounted for 16.8% (106/632),A6 (HPV56) accounted for 16.0% (101/632),A7 (HPV18,39,45,59,68) accounted for 68.7% (434/632),and A9 (HPV16,31,33,35,52,58) accounted for 98.6% (623/632).
There were 68 combination types of 2 of the 13 HPV-type coinfections. The most predominant types were HPV39&68 (14.6%,92/632),HPV16&52 (4.9%,31/632),and HPV16&58 (4.7%,30/632). There were a total of 10 types of dual coinfections with the number of individuals beyond 16,with the individual number of 457 (48.9%,309/632) (Table 2).
|
|
Table 2 Dual Infections in Different Cervical Disease Categories |
According to the type of HPV species classification,the dual infections could be divided into eight types (A5+A6,A5+A7,A5+A9,A6+A7,A6+A9,A7+A7,A7+A9,and A9+A9). The most predominant types were A9+A9 (26.6%),followed by A7+A9 (25.8%),A7+A7 (16.6%),A6+A9 (11.1%),A5+A9 (10.4%),A5+A7 (4.6%),A6+A7 (3.2%),and A5+A6 (1.76%). The constituent ratio of the dual infections at species level showed that the dual infections including A5 accounted for 16.8% (106/632),A6 accounted for 16.0% (101/632),A7 accounted for 50.2% (317/632),and A9 accounted for 73.9% (467/632) of the dual infections.
The risk of HPV infection and cervical lesions was investigated in the eight types of dual coinfections. The OR for LSIL of A5+A6 was greater than that of A5 single and A6 single types. The OR of A5+A7 was greater than that of A5 single and A7 single types. A6+A7,A7+A7,and A9+A9 had greater OR than that of the single species,respectively (Table 3).
|
|
Table 3 HPV Infections and Cytology Result-all Odds Ratios of Dual Infections in Comparison to the Normal Group |
All the ORs of the dual infections were greater than that of the single infection of the two types,respectively (Table 4).
|
|
Table 4 HPV infections and cytology result-all odds ratios of dual infections (n>16) in comparison to the normal group |
In the current study,HPV52 had the highest prevalence (4.4%),followed by HPV16 (3.7%) and HPV58 (3.4%),while HPV18 (1.3%) was ranked seventh. Previous studies have suggested that HPV52 and HPV58 are two important HPV types associated with CC in China. The oncogenic HPV prevalence result in the current study was consistent with those of previous studies[7-14].
The constituent ratio of each of the 13 oncogenic HPV types showed that HPV68 (82.1%),HPV39 (48.8%),and HPV59 (42.9%) constituted the highest proportion of multiple infections. HPV68,HPV39,and HPV59 belonged to Alpha genus seventh species (A7). Therefore,the dual infections including A7 may not occur randomly,whereas multiple-type infections occur more frequently than would be expected by chance alone.
As to each of the 13 HPV types,the ORs of multiple infections were all greater than that of the single infection,except HPV16 (Table 1). This was not consistent with previous studies.
Our results demonstrate that women with multiple infections were at a significantly increased risk for ASCUS,LSIL,and HSIL compared to those with single infections. Dual infections had a significantly increased risk for ASCUS,LSIL,and HSIL when compared with each of the two single types. Our results indicate that women with multiple infections are at a significantly increased risk for cervical disease compared to those with single infection.
This study is a relatively large-scale epidemiological survey of HR-HPV prevalence in China,and the prevalence data of the 13 HPV types have reference value for the surveillance of HPV infection and CC control and prevention. There are still some limitations of this study that should be noted. The HPV genotyping kit used in this study can detect only 13 HPV types of all the known HPV types; hence,the prevalence of multiple infections may be underestimated to some extent. In addition,the analysis of interaction between the different types may be limited.
In summary,this study investigated the prevalence of the most predominant oncogenic HPV types (HPV52,HPV16,and HPV58) in women with normal and abnormal cytology. This study suggests that women with multiple-type HPV infections were more likely to have abnormal cytology than those with single HPV-type infections.
| 1. | Chen W, Zheng R, Baade PD, et al. Cancer statistics in China, 2015[J]. CA Cancer J Clin , 2016, 66 :115–32. doi:10.3322/caac.21338 |
| 2. | de Villiers EM. Cross-roads in the classification of papillomaviruses[J]. Virology , 2013, 445 :2–10. doi:10.1016/j.virol.2013.04.023 |
| 3. | de Villiers EM, Fauquet C, Broker TR, et al. Classification of papillomaviruses[J]. Virology , 2004, 324 :17–27. doi:10.1016/j.virol.2004.03.033 |
| 4. | Muñoz N BF, de Sanjosé S, Herrero R, et al. International Agency for Research on Cancer Multicenter Cervical Cancer Study Group. Epidemiologic classification of human papillomavirus types associated with cervical cancer[J]. N Engl J Med , 2003, 348 :518–27. doi:10.1056/NEJMoa021641 |
| 5. | Hernández-Hernández DM, Ornelas-Bernal L, Guido-Jiménez M, et al. Association between high-risk human papillomavirus DNA load and precursor lesions of cervical cancer in Mexican women[J]. Gynecologic Oncology , 2003, 90 :310–7. doi:10.1016/S0090-8258(03)00320-2 |
| 6. | Solomon D, Schiffman M, Tarone R. Comparison of three management strategies for patients with atypical squamous cells of undetermined significance:baseline results from a randomized trial[J]. J Natl Cancer Inst , 2001, 93 :293–9. doi:10.1093/jnci/93.4.293 |
| 7. | Clifford GM GS, Herrero R, Muñoz N, et al. IARC HPV Prevalence Surveys Study Group. Worldwide distribution of human papillomavirus types in cytologically normal women in the International Agency for Research on Cancer HPV prevalence surveys:a pooled analysis[J]. Lancet , 2005, 366 :991–8. doi:10.1016/S0140-6736(05)67069-9 |
| 8. | Dai M, Bao YP, Li N, et al. Human papillomavirus infection in Shanxi Province, People's Republic of China:a population-based study[J]. Br J Cancer , 2006, 95 :96–101. doi:10.1038/sj.bjc.6603208 |
| 9. | Huang S AI, Miller BA, Beckmann AM. Human papillomavirus types 52 and 58 are prevalent in cervical cancers from Chinese women[J]. Int J Cancer , 1997, 70 :408–11. doi:10.1002/(ISSN)1097-0215 |
| 10. | Li LK, Dai M, Clifford GM, et al. Human papillomavirus infection in Shenyang City, People's Republic of China:A population-based study[J]. Br J Cancer , 2006, 95 :1593–7. doi:10.1038/sj.bjc.6603450 |
| 11. | Li Z, Liu F, Cheng S, et al. Prevalence of HPV infection among 28,457 Chinese women in Yunnan Province, southwest China[J]. Sci Rep , 2016, 6 :21039. doi:10.1038/srep21039 |
| 12. | Chaturvedi AK, Katki HA, Hildesheim A, et al. Human papillomavirus infection with multiple types:pattern of coinfection and risk of cervical disease[J]. J Infect Dis , 2011, 203 :910–20. doi:10.1093/infdis/jiq139 |
| 13. | Dickson EL, Vogel RI, Bliss RL, et al. Multiple-type human papillomavirus (HPV) infections:a cross-sectional analysis of the prevalence of specific types in 309,000 women referred for HPV testing at the time of cervical cytology[J]. Int J Gynecol Cancer , 2013, 23 :1295–302. doi:10.1097/IGC.0b013e31829e9fb4 |
| 14. | Dickson EL, Vogel RI, Geller MA, et al. Cervical cytology and multiple type HPV infection:a study of 8182 women ages 31-65[J]. Gynecol Oncol , 2014, 133 :405–8. doi:10.1016/j.ygyno.2014.03.552 |
| 15. | Trottier H, Mahmud S, Costa MC, et al. Human papillomavirus infections with multiple types and risk of cervical neoplasia[J]. Cancer Epidemiol Biomarkers Prev , 2006, 15 :1274–80. doi:10.1158/1055-9965.EPI-06-0129 |
| 16. | Chen CA, Liu CY, Chou HH, et al. The distribution and differential risks of human papillomavirus genotypes in cervical preinvasive lesions:A Taiwan Cooperative Oncologic Group Study[J]. Int J Gynecol Cancer , 2006, 16 :1801–8. doi:10.1111/ijg.2006.16.issue-5 |
| 17. | Gary M, Clifford RKR, Silvia Franceschi, et al. Human Papillomavirus Genotype Distribution in Low-Grade Cervical Lesions:Comparison by Geographic Region and with Cervical Cancer[J]. Cancer Epidemiol Biomarkers Prev , 2005, 14 :1157–61. doi:10.1158/1055-9965.EPI-04-0812 |
| 18. | Rassu M, Bertoloni G, Mengoli C, et al. HPV genotype prevalence in cervical specimens with abnormal cytology:a report from north-east Italy[J]. Scand J Infect Dis , 2005, 37 :476–81. doi:10.1080/00365540510036633 |
| 19. | Smith JS, Lindsay L, Hoots B, et al. Human papillomavirus type distribution in invasive cervical cancer and high-grade cervical lesions:a meta-analysis update[J]. Int J Cancer , 2007, 121 :621–32. doi:10.1002/(ISSN)1097-0215 |
 2016, Vol. 29
2016, Vol. 29


