2. National Center for Chronic and Noncommunicable Disease Control and Prevention, Chinese Center for Disease Control and Prevention, Beijing 102206, China;
3. Department of Neurology, Beijing Tiantan Hospital, Capital Medical University, Beijing 100050, China;
4. National Institute for Nutrition and Health, Chinese Center for Disease Control and Prevention, Beijing 102206, China
Objective To update the estimated prevalence rates of smoking and examine major metabolic diseases associated with smoking status in Chinese adults.
Methods Using a complex, multistage, probability sampling design, we recruited a nationally representative sample of 98,658 Chinese adults aged ≥18 years in 2010. Information on current, former, never, and passive smoking status was obtained using a standard questionnaire. All estimates were weighted to represent the overall Chinese adult population.
Results The estimated proportion of current smokers was 28.3% for Chinese adults aged ≥18 years. The corresponding values of former and passive smokers were 5.1% and 21.4%, respectively. Additionally, former smokers were found to have a less favorable metabolic risk profile among all categories of smoking status in both men and women. The prevalence of metabolic diseases such as diabetes and hypertension also increased with a greater number of smoking pack-years in men.
Conclusion The prevalences of current smoking and passive smoking remain high in Chinese adults.
Cigarette smoking is the leading cause of preventable death worldwide. Many diseases, including chronic obstructive pulmonary disease, cardiovascular disease, and many types of cancer are causally associated with tobacco use[1-2]. In addition, nearly 6 million deaths and more than half a trillion dollars of healthcare expenditure are attributable to smoking each year worldwide[3].
China is the largest tobacco producer and consumer in the world[4]. Domestic tobacco production has steadily increased from 651 billion cigarettes in 1979 to 2290 billion cigarettes in 2009. Moreover, more than 99% of domestically produced cigarettes are consumed in the country[5]. The overall prevalence of smoking in China was reported to be 33.9% in 1984[6], and this increased to 35.8% in 2002[7]. A recent World Health Organization (WHO) report indicated that China has the largest number of tobacco-related deaths in the world with 1.37 million in 2014[8]. Using a complex, multistage, probability sampling design, we conducted the 2010 China Noncommunicable Disease Surveillance study to examine the current status of several major chronic diseases, such as diabetes, hypertension, and dyslipidemia, and related behavioral risk factors, including smoking. For the current analysis, we aimed to estimate the prevalence of smoking in the overall Chinese population, as well as in subgroups, and to examine cross-sectional associations between smoking status and metabolic disorders using this large, nationally representative survey of 98, 658 Chinese adults.
RESEARCH DESIGN AND METHODS Study PopulationThe 2010 China Noncommunicable Disease Surveillance study recruited participants from 162 study sites, covering major geographic areas of all 31 provinces, autonomous regions, and municipalities in mainland China. Participants who represent civilian, noninstitutionalized adults were selected at each site using a complex, multistage, probability sampling design. Only persons living in their current residence for ≥6 months were eligible to participate. Detailed study design and sampling methods have been previously published[9-10]. Briefly, in the first stage of sampling, 4 subdistricts in urban areas, or townships in rural areas, were selected from each site with probability proportional to size (PPS). In the second stage of sampling, 3 neighborhood communities or administrative villages were selected with PPS. In the third stage of sampling, households within each neighborhood community or administrative village were listed, and from these, 50 households were randomly selected. In the final stage of sampling, 1 person aged ≥18 years was selected randomly from each household using a Kish selection table. Replacement with a similar household in the same or nearby neighborhood community or administrative village was implemented if the selected individual did not wish to participate. Finally, 109, 023 adults were selected and a total of 98, 658 people participated in the survey. The overall response rate was 90.5% and the replacement rate was 9.25%. Those who did not respond were either unavailable or refused to participate.
The Ethical Review Committee of the Chinese Center for Disease Control and Prevention (CDC) approved this study and all participants provided written informed consent.
Data CollectionAccording to a standard protocol, data were collected in examination centers at local health stations or community clinics in the participants' residential area by trained staff. A questionnaire including information on smoking status, demographic characteristics, medical history, and lifestyle factors was used by trained interviewers. Body mass index (BMI) was calculated as weight (kg)/height (m2). Waist circumference was determined at the midpoint between the lowest costal ridge and the upper border of the iliac crest when participants were standing. Blood pressure was measured in triplicate using the non-dominant arm after at least 5 min of rest with an automated device (OMRON Model HEM-7071, Omron Co, Kyoto, Japan). Participants were asked to sit comfortably for 5 min before the first measurement was taken, and the set interval between measurements was 1 min.
A venous blood sample was drawn from each participant following a 10 h fast to assess fasting blood sugar and lipid profiles. Participants without a self-reported history of diabetes underwent a two-point (0 and 2 h) 75 g oral glucose tolerance test. Plasma glucose was measured within 24 h of collection using glucose oxidase or hexokinase methods. A Hemoglobin Capillary Collection System (Bio-Rad Laboratories, Hercules, CA, USA) was used to collect capillary blood samples for the measurement of hemoglobin A1c (HbA1c) and capillary values were converted into venous values using a validated formula[9]. Serum samples were aliquoted and frozen at -80 ℃, and were delivered to the central laboratory by air in dry ice, where serum total cholesterol, low-density lipoprotein (LDL) cholesterol, high-density lipoprotein (HDL) cholesterol, and triglycerides (TG) levels were tested using an autoanalyser (ARCHITECT ci16200, Abbott Laboratories, Chicago, IL, USA).
DefinitionsCurrent smokers were those who were currently smoking at the time of the survey. Former smokers were those who had smoked in their lifetime but had stopped smoking by the time of the survey. Passive smokers were those who did not smoke themselves but were exposed to another person's tobacco smoke for at least 15 min daily on more than 1 day per week. Never smokers were those who had not smoked in their lifetime and were not passive smokers. Pack-years of smoking were calculated by multiplying the number of years smoked by the number of cigarette packs smoked per day[11].
Those with a BMI of 25.0 to 29.9 kg/m2 were classified as overweight while those with a BMI ≥30.0 kg/m2 were classified as obese[12]. Central obesity was defined as a waist circumference of ≥90 cm in men and ≥80 cm in women[13]. Diabetes was defined according to the 2010 American Diabetes Association (ADA) criteria, which include 1) a self-reported previous diagnosis by health professionals, and/or 2) fasting plasma glucose (FPG) ≥126 mg/dL, and/or 3) 2-h plasma glucose (PPG) ≥200 mg/dL, and/or 4) HbA1c ≥6.5%[14]. Hypertension was defined as systolic blood pressure (SBP) ≥140 mmHg, and/or diastolic blood pressure (DBP) ≥90 mmHg, and/or self-reported current use of anti-hypertensive medications[15]. Dyslipidemia was defined according to the criteria of the US National Cholesterol Education Program Adult Treatment Panel Ⅲ, which include 1) total cholesterol ≥240 mg/dL, and/or 2) HDL cholesterol <40 mg/dL, and/or 3) LDL cholesterol ≥160 mg/dL, and/or 4) triglycerides ≥200 mg/dL, and/or 5) current use of lipid-lowering drugs[16].
Statistical AnalysisPrevalence rates of current smoking, former smoking, passive smoking, and never smoking were estimated in the overall Chinese adult population and in subgroups according to geographical location, age, economic development, BMI, and waist circumference. Absolute numbers of Chinese adults with different smoking status were also estimated in the overall population and in subgroups. Means and 95% confidence intervals (CIs) of metabolic-related key variables, and percentages and 95% CIs of major metabolic diseases were calculated according to cigarette smoking status as well as the numbers of pack-years of current smokers.
Data were analyzed using SAS version 9.3 (SAS Institute Inc., Cary, NC, USA) and SUDAAN version 10.0 (Research Triangle Institute, Research Triangle Park, NC, USA). Weight coefficients, derived from 2010 China population census data and the sampling scheme of the current survey, were used to calculate national estimates for Chinese adults aged ≥18 years. The Taylor-linearization method appropriate for the complex survey design was used to calculate standard errors.
RESULTSOverall, the estimated prevalence rates of current smoking, former smoking, passive smoking, and never smoking in Chinese adults aged ≥18 years were 28.3%, 5.1%, 21.4%, and 45.1%, respectively (Table 1). Individuals living in urban areas or more developed regions were less likely to smoke than those living in rural areas or less developed regions. Current smoking was most prevalent among individuals aged 40 to 59 years. Generally, the prevalence of former smoking increased with age, while the prevalence of passive smoking decreased with age. Current smoking was more prevalent in Chinese adults with a lower BMI or waist circumference. In addition, former smoking was more prevalent in Chinese adults with a higher BMI but lower waist circumference.
|
|
Table 1 Prevalence of Cigarette Smoking among Chinese Adults |
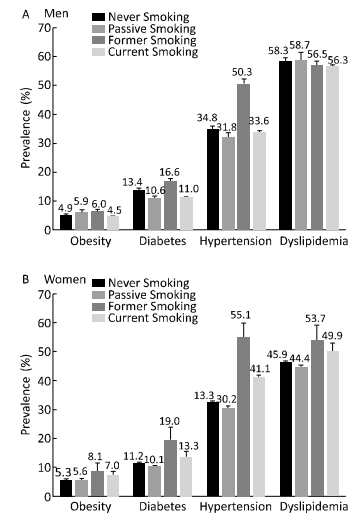
Estimations of the mean levels of key metabolic variables and prevalences of major metabolic diseases among Chinese adults categorized by smoking status are presented in Table 2 and Figure 1, respectively. Generally, former smokers had the least favorable metabolic profile in both men and women, including an older age, and higher BMI, waist circumference, blood pressure, total cholesterol, LDL cholesterol, fasting and 2-h post-load glucose, and HbA1c levels. They also had increased prevalences of obesity, diabetes, hypertension, and dyslipidemia. Male passive smokers and female current smokers had the second least favorable metabolic profile among all smoking categories.
|
|
Table 2 Mean Levels of Key Metabolic Variables among Chinese Adults with Different Cigarette Smoking Status |
|
Download:
|
| Figure 1 Prevalence of major metabolic diseases among Chinese adults with different cigarette smoking status. | |
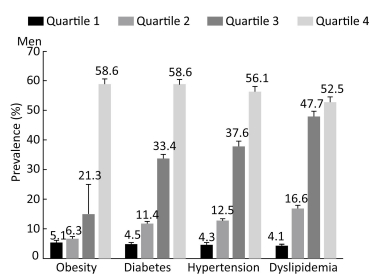
Estimations of mean levels of key metabolic variables and prevalences of major metabolic diseases categorized by the number of pack-years among male current smokers are presented in Table 3 and Figure 2, respectively. Because only a very limited proportion of women were current smokers, data are not presented for women. In male current smokers, estimated levels of most metabolic variables such as waist circumference, blood pressure, total cholesterol, LDL cholesterol, HDL cholesterol, fasting and 2-h post-load glucose, and HbA1c levels, as well as estimated prevalence rates of diabetes and hypertension increased dose-dependently with an elevated number of smoking pack-years. However, BMI and triglyceride levels decreased from quartile 2 through quartile 4 of smoking pack-years, and the prevalence of obesity and dyslipidemia also decreased with increasing quartiles of smoking pack-years.
|
|
Table 3 Mean Levels of Key Metabolic Variables among Male Current Smokers According to the Number of Pack-years |
|
Download:
|
| Figure 2 Prevalence of major metabolic diseases among male current smokers according to the number of pack-years. | |
The current study provided updated prevalence estimates of current smoking, former smoking, and passive smoking status in Chinese men and women aged ≥18 years using a large, nationally represen- tative sample. The estimated proportion of current smokers was 28.3%. The corresponding values of former smokers and passive smokers were 5.1% and 21.4%, respectively. In addition, mean levels of key metabolic variables and the prevalence of major metabolic diseases were also estimated according to smoking categories, as well as numbers of smoking pack-years in men and women separately. Former smokers were found to have a less favorable metabolic risk profile, and metabolic risks also elevated with increasing number of smoking pack-years.
China is regarded as the epicenter of the worldwide tobacco problem and has one of the highest male adult smoking rates, according to a 2014 WHO report[8]. Compared with previous national surveys, the prevalence of current smoking in Chinese men has remained high for the past two decades: 61.0% in 1984[6], 63.0% in 1996[4], and 57.4% in 2002[17]. On the contrary, Chinese women have much lower smoking rates than men: 7.0% in 1984[6], 3.8% in 1996[4], 2.6% in 2002[17]. Meanwhile, the global prevalence of tobacco smoking in people older than 15 years has decreased from 41.2% in 1980 to 31.1% in 2012 for men and from 10.6% to 6.2% for women[18]. In developed countries such as the United States (US), year-to-year decreases in the prevalence of smoking have also been observed in recent decades[19]. Therefore, in a world where combatingsmoking is advocated effortlessly and successes have been achieved in many countries, the ongoing high prevalence of current smoking in Chinese men is especially worrisome. Smoking cessation rates in China are low, as indicated by a relatively small number of former smokers compared with current smokers. Furthermore, the majority of current smokers (66.8%) have never considered ceasing smoking, or taking action to do so, according to the interviews conducted during our study.
To understand and interpret the continuously high prevalence of current smoking, important social and cultural factors should be taken into serious consideration. First, many investigators believe that a major conflict of interest exists for China's State Tobacco Monopoly Administration, which not only leads tobacco control efforts, but is also responsible for maintaining the country's tobacco industry, thus representing a powerful barrier to tobacco intervention in China[20]. Second, the present health warnings on Chinese cigarette packages are ineffective. China seems to apply double standards since it adheres to packaging regulations when selling products to foreign countries but uses weakly worded text-only health warnings in mainland China[21]. Third, evidence shows that there are still large gaps in the population's awareness of the risks of smoking[4]. For example, cigarettes are popular gifts in China. Estimates derived from national survey data suggest that the average smoker receives cigarettes as gifts approximately five times a year[22]. The giving and receiving of luxury cigarettes shows social approbation and social status, and is often used as a way of facilitating business deals[23].
The tobacco epidemic in China indicates a high disease burden from which China is suffering now and from which it will suffer in the future. In other countries such as the US, although tobacco control has more than halved smoking rates, and tobacco control efforts have averted nearly 8 million deaths since 1964, smoking-attributable mortality and morbidity rates are still alarming[24-25]. Therefore, the greatest health risks of smoking may be yet to occur in China[26], as it is still in the early stages which are characterized by high production and consumption. We explored metabolic risks in Chinese adults with different smoking statuses and found that former smokers had the least favorable metabolic profile among all categories (i.e. current smokers, former smokers, never smokers, and passive smokers). However, this finding should be interpreted with caution. It is possible that smoking cessation may have a temporary negative effect on glycemic control or other metabolic risks; a prolonged duration after cessation might contribute to a decreased risk of developing metabolic diseases, such as diabetes, to an extent similar to that in never smokers[27]. Former smokers might therefore require additional attention, and close monitoring and interventions to prevent metabolic diseases should be implemented. Another population cohort study supported a net cardiovascular benefit of smoking cessation, despite subsequent weight gain[28]. In addition, reverse causation might also play a role because the development of metabolic diseases could promote smoking cessation. Moreover, potential confounding by the older age of former smokers, as well as smoking duration, duration after cessation, and unhealthy behaviors such as binge drinking, poor diet, and physical inactivity that may co-exist with smoking indicates that a causality cannot be defined.
Chinese women smoked much less than men, however, this does not protect them from second-hand smoke, although the prevalence of passive smoking decreased from 54.6% in 2002 to 32.1% in 2010[17]. Passive smoking can increase the risk of chronic obstructive pulmonary disease[29], lung cancer[30], breast cancer[31], and cardiovascular disease[32], and is especially detrimental to the health of women. For example, in the Shanghai Women's Health Study, the prevalence of stroke among female nonsmokers increased with the greater intensity and duration of their husbands' smoking[33]. Furthermore, a moderately increased risk of all-cause mortality, and mortality due to lung cancer and cardiovascular disease was also found in Chinese female nonsmokers[34]. Therefore, abstinence from smoking or smoking cessation in men has important clinical and public health implications for the patients themselves, as well as for women who would otherwise be exposed to passive smoking.
In addition, lung cancer was the highest population-attributable risk associated with cigarette smoking in China[26], and there is a dose-response relationship between smoking and lung cancer risk[1]. In our survey, we found that estimated levels of most metabolic variables, such as lipid and glucose, increased with an elevated number of smoking pack-years in men, and therefore glucose and other metabolic factors may play a role in carcinogenesis[35]. However, we did not collect information on lung cancer prevalence and therefore it is impossible for us to connect these metabolic changes with the early detection of lung cancer.
The current study has several strengths. It has provided the latest national estimates on the prevalence of current smoking, former smoking, and passive smoking in Chinese adults, as well as in important subgroups, using a large, nationally representative sample. Projections on sample weighting, which estimated the numbers of Chinese adults with different smoking status, presented the absolute burden of smoking in China. In addition, metabolic risks were also comprehensively evaluated according to smoking status. Finally, a strict quality assurance and quality control program was implemented to ensure data validity and reliability.
There are also several limitations to the present study. First, smoking status was defined by self-reported data collected from questionnaires through face-to-face interviews. There is the potential for misclassification when using this type of data. Second, data on duration since smoking cessation in former smokers were not available and therefore metabolic risks could not be evaluated according to years of cessation. Third, the cross-sectional nature of the current study prevents analysis of any causal inference between smoking status and risks of metabolic diseases.
In conclusion, in a country where the number of smokers accounts for one third of the world's total, programs to promote smoking cessation should be enhanced at all levels by central and local governments, as well as non-governmental organizations. Tobacco control programs such as raising taxes on cigarettes and banning tobacco-related advertising in mass media and public places are already in place. Meanwhile, Beijing's new legislation to ban smoking in all indoor public places, which took effect on June 1st 2015, is one of the most stringent anti-smoking measures in China, and aims to provide a model for further national tobacco-control regulations[36]. However, greater efforts are needed to reduce the high rates of tobacco use in men, to maintain the low rates in women, to protect non-smokers from second-hand smoke, and to reduce risks of diseases attributed to smoking in China.
ACKNOWLEDGEMENTSDr. Xu was supported by the Pujiang Talent Program from Science and Technology Commission of Shanghai Municipality. Dr. Ding was supported by the grant BXJ201613 from the Doctorial Innovation Foundation of Shanghai Jiao-Tong University School of Medicine. The funding agencies had no role in the design and conduct of the study, in the collection, management, analysis, and interpretation of the data, or in the preparation, review, or approval of the manuscript. Dr. BI Yu Fang has full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. We thank all the research staff from local Centers for Disease Control and Prevention for their collection of data and blood samples. We also thank all the study participants for their participation and contribution.
CONFLICTS OF INTERESTWe declare that we have no conflicts of interest.
Investigators for the 2010 China Noncommunicable Disease Surveillance Group
Advisory Group KONG Ling Zhi, YANG Gong Huan, CHEN Yu De, LI Guang Wei, LI Ke Ji, ZHAO Dong, CHEN Jia Lun, PAN Chang Yu, ZENG Zheng Pei, NING Guang, MU Yi Ming, TENG Wei Ping, LIAO Er Yuan, ZHAO Jia Jun, WANG Wei Qing, GUO Xiao Hui, HONG Tian Pei, QIU Ming Cai, LI Cai Ping, SHAN Zhong Yan, LIU Zhi Min, GAO Xin, LIU Chao, CHEN Lu Lu, YAN Li, TONG Nan Wei, SHI Bing Yin, GE Jia Pu, XING Xiao Ping, LIU Jie, DENG Hua Cong, CHEN Biao, CHEN Chun Ming, CHEN Jun Shi, LI Hui, LIU Li Sheng, PENG Dan Tao, SHI Xiao Ming, WANG Wen Zhi, WANG Yong Jun, WU Zheng Lai.
Working Group ZHAO Wen Hua, NING Guang, BI Yu Fang, LAI Jian Qiang, JIANG Yong, WANG Li Min, DAI Meng, HU Nan, HUANG Zheng Jing, LI Jian Hong, LI Xiao Yan, LI Yi Chong, WANG Zhi Hui, ZHANG Mei, YIN Peng, XU Yu, ZHOU Wen Zhong, BAI Ya Min, CAI Xiao Ning, CAO Guo Ping, CHEN Xiao Rong, DONG Wen Lan, DUAN Lei Lei, FENG Ya Jing, HE Yuan, HUANG Yun, LI Mian, LI Bo Ren, MI Sheng Quan, SHI Xiao Qian, WANG Bao Hua, WANG Chun Xiao, WANG Tian Ge, WANG Yi Long, WANG Zhuo Qun, WU Hong Xi, XING Dan, YANG Jing, ZHAO Xing Quan, ZHENG Tao, YANG Jing Ren, ZHANG Di, WU Yu Bei.
| 1. | Smoking and Health:Report of the Advisor Committee to the Surgeon General of the Pub Health Service. Surgeon General's Advisory Committee on Smoking and Health[1964]. http://profiles.nlm.nih.gov/NN/B/B/M/Q/.[2016-6-11] |
| 2. | The Health Consequences of Smoking-50 Years of Progress:A Report of the Surgeon General, 2014. http://www.surgeongeneral.gov/library/reports/50-years-of-progress/index.html.[2016-6-11] |
| 3. | WHO report on the global tobacco epidemic, 2013:enforcing bans on tobacco advertising, promotion and sponsorship. Geneva:World Health Organization, 2013; 12. |
| 4. | Yang G, Fan L, Tan J, et al. Smoking in China:findings of the 1996 National Prevalence Survey[J]. JAMA , 1999, 282 :1247–53. doi:10.1001/jama.282.13.1247 |
| 5. | Report of tobacco control in China on World No-Tobacco Day 2012-Chinese Association on Tobacco Control. 2012. |
| 6. | Weng XZ, Hong ZG, Chen DY. Smoking prevalence in Chinese aged 15 and above[J]. Chin Med J (Engl) , 1987, 100 :886–92. |
| 7. | Xiao L, Yang J, Wan X, et al. What is the prevalence of smoking in China?[J]. Chiese Journal of Epidemiology , 2009, 30 :30–3. |
| 8. | 2014 GLOBAL PROGRESS REPORT on implementation of the WHO Framework Convention on Tobacco Control. http://www.who.int/fctc/reporting/summary_analysis/en/. [2016-06-11]. p.68. |
| 9. | Xu Y, Wang L, He J, et al. Prevalence and control of diabetes in Chinese adults[J]. JAMA , 2013, 310 :948–59. doi:10.1001/jama.2013.168118 |
| 10. | Bi Y, Jiang Y, He J, et al. Status of cardiovascular health in Chinese adults[J]. J Am CollCardiol , 2015, 65 :1013–25. doi:10.1016/j.jacc.2014.12.044 |
| 11. | Prignot J. Quantification and chemical markers of tobacco-exposure[J]. Eur J Respir Dis , 1987, 70 :1–7. |
| 12. | World Health Organization. Obesity:preventing and managing the global epidemic; 1997. http://www.who.int/nutrition/publications/obesity_executive_summary.pdf. [2016-06-02] |
| 13. | The World Health Organization Western Pacific Region. The Asia-Pacific perspective:redefining obesity and its treatment. http://www.wpro.who.int/nutrition/documents/docs/Redefiningobesity.pdf. [2016-6-11] |
| 14. | Diagnosis and classification of diabetes mellitus. Diabetes Care, 2010; 33, S62-9. |
| 15. | James PA, Oparil S, Carter BL, et al. 2014 evidence-based guideline for the management of high blood pressure in adults:report from the panel members appointed to the Eighth Joint National Committee (JNC 8)[J]. JAMA , 2014, 311 :507–20. doi:10.1001/jama.2013.284427 |
| 16. | Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel Ⅲ). JAMA, 2001; 285, 2486-97. |
| 17. | Yang GH, Ma JM, Liu N, et al. Smoking and passive smoking in Chinese, 2002[J]. Zhonghua Liu Xing Bing Xue Za Zhi , 2005, 26 :77–83. |
| 18. | Ng M, Freeman MK, Fleming TD, et al. Smoking prevalence and cigarette consumption in 187 countries:1980-2012[J]. JAMA , 2014, 311 :183–92. doi:10.1001/jama.2013.284692 |
| 19. | Jamal A, Agaku IT, O'Connor E, et al. Current cigarette smoking among adults-United States:2005-2013[J]. MMWR Morb Mortal Wkly Rep , 2014, 63 :1108–12. |
| 20. | Dan X, Yuankai S, Chen W. Tobacco in China[J]. Lancet , 2014, 383 :2045–6. |
| 21. | 2014 Tobacco Health Warnings in China:Evidence of Effectiveness and Implications for Action. http://www.itcproject.org/resources/view/1636. [2016-6-11] |
| 22. | Huang LL, Thrasher JF, Jiang Y, et al. Incidence and correlates of receiving cigarettes as gifts and selecting preferred brand because it was gifted:findings from the ITC China Survey[J]. BMC Public Health , 2012, 12 :996. doi:10.1186/1471-2458-12-996 |
| 23. | Chu A, Jiang N, Glantz SA. Transnational tobacco industry promotion of the cigarette gifting custom in China[J]. Tob Control , 2011, 20 :e3. |
| 24. | Holford TR, Meza R, Warner KE, et al. Tobacco control and the reduction in smoking-related premature deaths in the United States:1964-2012[J]. JAMA , 2014, 311 :164–71. doi:10.1001/jama.2013.285112 |
| 25. | Rostron BL, Chang CM, Pechacek TF. Estimation of cigarette smoking-attributable morbidity in the United States[J]. JAMA Intern Med , 2014, 174 :1922–8. doi:10.1001/jamainternmed.2014.5219 |
| 26. | Gu D, Kelly TN, Wu X, et al. Mortality attributable to smoking in China[J]. N Engl J Med , 2009, 360 :150–9. doi:10.1056/NEJMsa0802902 |
| 27. | Lycett D, Nichols L, Ryan R, et al. The association between smoking cessation and glycaemic control in patients with type 2 diabetes:a THIN database cohort study[J]. Lancet Diabetes Endocrinol , 2015, 3 :423–30. doi:10.1016/S2213-8587(15)00082-0 |
| 28. | Clair C, Rigotti NA, Porneala B, et al. Association of smoking cessation and weight change with cardiovascular disease among adults with and without diabetes[J]. JAMA , 2013, 309 :1014–21. doi:10.1001/jama.2013.1644 |
| 29. | Yin P, Jiang CQ, Cheng KK, et al. Passive smoking exposure and risk of COPD among adults in China:the Guangzhou Biobank Cohort Study[J]. Lancet , 2007, 370 :751–7. doi:10.1016/S0140-6736(07)61378-6 |
| 30. | Taylor R, Najafi F, Dobson A. Meta-analysis of studies of passive smoking and lung cancer:effects of study type and continent[J]. Int J Epidemiol , 2007, 36 :1048–59. doi:10.1093/ije/dym158 |
| 31. | Pirie K, Beral V, Peto R, et al. Passive smoking and breast cancer in never smokers:prospective study and meta-analysis[J]. Int J Epidemiol , 2008, 37 :1069–79. doi:10.1093/ije/dyn110 |
| 32. | Whincup PH, Gilg JA, Emberson JR, et al. Passive smoking and risk of coronary heart disease and stroke:prospective study with cotinine measurement[J]. BMJ , 2004, 329 :200–5. doi:10.1136/bmj.38146.427188.55 |
| 33. | Zhang X, Shu XO, Yang G, et al. Association of passive smoking by husbands with prevalence of stroke among Chinese women nonsmokers[J]. Am J Epidemiol , 2005, 161 :213–8. doi:10.1093/aje/kwi028 |
| 34. | Wen W, Shu XO, Gao YT, et al. Environmental tobacco smoke and mortality in Chinese women who have never smoked:prospective cohort study[J]. BMJ , 2006, 333 :376. doi:10.1136/bmj.38834.522894.2F |
| 35. | Melkonian SC, Daniel CR, Ye Y, et al. Glycemic Index, Glycemic Load, and Lung Cancer Risk in Non-Hispanic Whites[J]. Cancer Epidemiol Biomarkers Prev , 2016, 25 :532–9. doi:10.1158/1055-9965.EPI-15-0765 |
| 36. | Beijing Tobacco Control Law. http://www.wpro.who.int/china/mediacentre/releases/2014/2014112802/en/. [2016-6-11] |
 2016, Vol. 29
2016, Vol. 29


