扩展功能
文章信息
- 焦鹏, 陈飞, 金权, 陈楠楠, 张莉, 马宁
- JIAO Peng, CHEN Fei, JIN Quan, CHEN Nannan, ZHANG Li, MA Ning
- 重度牙周炎致牙齿松动脱落患者前牙美学区综合治疗1例报告及文献复习
- Comprehensive treatment of anterior esthetic zone in patient with loosening and falling of teeth induced by severe periodontitis: A case reeport and literature review
- 吉林大学学报(医学版), 2018, 44(02): 421-424
- Journal of Jilin University (Medicine Edition), 2018, 44(02): 421-424
- 10.13481/j.1671-587x.20180241
-
文章历史
- 收稿日期: 2017-09-12
2. 吉林大学口腔医院急诊科, 吉林 长春 130021
2. Department of Emergency, Stomatology Hospital, Jilin University, Changchun 130021, China
目前,重度牙周炎导致的牙齿松动脱落已引起人们的高度重视,而缺牙区的种植修复则成为其重要的治疗手段。但重度牙周炎造成的牙槽骨吸收,导致了种植修复中骨量不足,使国内许多种植医师对于牙周病患者的即刻种植有所顾虑,特别是前牙区重度牙量不足和软组织缺损严重影响种植修复后的美学效果和形态功能,使患者的满意度降低。因此,术前的综合评估和多学科综合考虑,制订合理的治疗方案成为重度牙周炎致牙齿松动脱落患者前牙美学区种植修复的目标。目前国内外对于前牙区的种植美学修复研究[1-2]多为单颗种植体,有关多颗相邻种植体的美学评价少有报道。本文作者报道1例重度牙周炎患者,在牙周基础治疗的基础上,行即刻种植和骨引导再生手术,并通过前牙连续多颗牙修复实现其美学要求,为临床多学科综合治疗提供理论依据及临床指导。
1 临床资料 1.1 一般资料患者,男性,57岁,因上下前牙松动不适半年余于2015年11月就诊于吉林大学口腔医院牙周病科。患者半年前自觉上下前牙松动不适,有“伸长感”,近期松动加重,影响咀嚼,来诊。无牙周治疗史,患者每天刷牙1次,无吸烟史。既往史:否认全身系统性疾病及家族遗传病史,无过敏史及长期用药史。
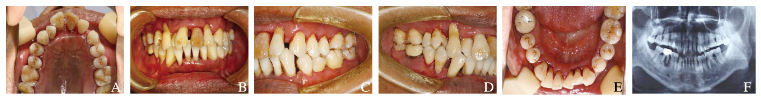
1.2 专科检查全口口腔卫生较差,软垢指数(debris index,DI)为2,牙石指数(alculus index, CI)为2~3,可探及龈下牙石,牙龈色暗红,牙龈乳头水肿,质地松软,探针出血(bleeding on probing, BOP)(+)。11、21、22、41探针深度(probing depth,PD)为6~8 mm,附着丧失(attachment loss, AL)为8~11 mm,牙龈萎缩2~3 mm,松动Ⅲ°。42松动Ⅱ°。PD为8~10 mm,AL为2~3 mm,牙龈退缩2~3 mm,松动Ⅲ°,根分叉病变Ⅲ°。浅覆牙合,浅覆盖,低位笑线,无明显露龈笑。
1.3 曲面断层片11、21、22牙槽骨吸收达根尖1/3,41根2/3处可见根折影,41、42牙槽骨吸收达根中1/3,46根管欠充,近中牙根呈弧形吸收,根分叉处可见低密度影像。
1.4 临床诊断慢性牙周炎(重度)。
1.5 治疗计划(主诉牙)对患者进行术前评估,告知患者可能存在的美学风险,应患者美学要求,经牙周、种植、牙体和修复科会诊,制订以下治疗方案。牙周基础治疗:对患者进行口腔卫生指导,行洁治、刮治和根面平整。种植治疗:行11、21、22、41、42拔除术、即刻种植术;由于患者唇侧软硬组织有明显缺损,建议采用引导骨再生(guided bone regeneration, GBR)进行骨增量,拟行自体骨移植(autogenous bone graft, ABG);采用膜龈手术增宽附着龈,拟行游离龈移植,但患者拒绝接受ABG及游离龈移植术,最终决定采用人工骨粉修复骨缺损,对于牙龈退缩的情况,拟采用龈瓷材料修复。对于非主诉牙46,行46拔除术后,采用GBR进行骨增量,行延期种植。牙体、修复治疗:在二期术后,应患者美学要求,考虑到前牙区牙龈退缩、牙齿变色、扭转、间隙过大等一系列问题,经牙体、修复科会诊后,取消术前修复治疗方案,拟行12、13、23、31、32、33、43根管治疗术,13-23、33-43固定修复。
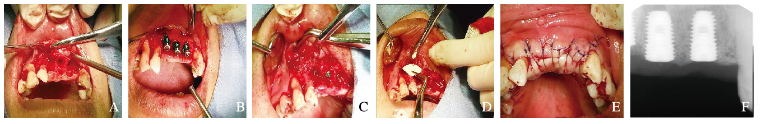
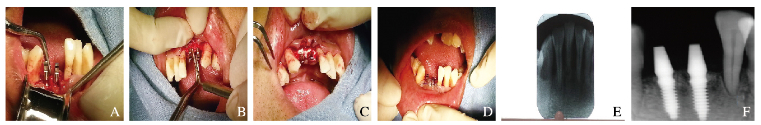
1.6 治疗程序(主诉牙)2015年9—10月行牙周基础治疗,对患者进行口腔卫生指导后,行洁治、刮治和根面平整,辅以药物治疗。牙周治疗后2个月行手术治疗,术前采集患者静脉血,离心备用,常规消毒、铺巾,局麻下微创拔除11、21、22、41和42,搔刮牙槽窝,切开翻瓣,彻底清除拔牙窝内肉芽组织,常规逐级备洞,植入ITI种植体5枚,11、21和22采用骨水平种植体,接入愈合螺丝,41和42采用一段式种植体。于骨缺损处放置Bio-oss骨粉,覆盖在暴露的种植体表面及缺损的牙槽骨间,制备富血小板纤维蛋白(platelet rich fibrin, PRF)膜,将PRF膜覆盖于创口处,表面覆盖Bio-Gide生物膜,严密缝合,术后口服抗生素5d,氯已定含漱液含漱,术后2周拆线。
术后5个月行二期手术,11、21和22取出愈合螺丝,更换愈合基台;12、13、23、31、32、33和43行根管治疗、牙体预备;二期手术2周后11、21、22戴金属基台,13-23、33-43常规取模,送义齿加工厂制作义齿,13-23、33-43全瓷固定修复;颈部采用牙龈瓷,完成永久修复。长期随访修复效果。
2 结果牙周基础治疗后情况:牙周状况稳定,牙周组织炎症得到了有效控制(图 1,见插页八);一期术后曲面断层显示种植体位置良好,种植体周围骨量充足,牙槽嵴高度恢复正常水平(图 2和3,见插页八);术后2周拆线见:牙龈软组织愈合良好,未见红肿渗出及生物膜外露,牙槽嵴丰满度较好;二期术后:袖口形态良好,牙龈颜色及形态未见明显异常;种植修复完成后:边缘龈水平与笑线基本一致、牙龈颜色及形态良好,前牙颜色与邻牙基本协调,牙体形态协调对称、排列整齐(图 4,见插页八)。曲面断层显示种植体颈部和顶端有新生骨生成。修复后较好地恢复了患牙的咀嚼发音功能,无明显的异物感,患者对美学修复效果满意;疗效追踪观察:修复后2个月复查,所有修复体形态及功能完好,种植体与周围骨结合牢固,无松动不适症状,种植体周围软组织无明显炎症,效果较稳定。
|
| 图 1 重度牙周炎致牙齿松动脱落患者术前的口内照片(A-E)及X线片(F) Figure 1 Intraoral photographs(A-E) and radiographs(F) of patient with loosening teeth induced by severe periodontitis before operation |
|
|
|
| 图 2 重度牙周炎致牙齿松动脱落患者术中口内照片(A-E)及X线片(F)(上颌) Figure 2 Intraoral photographs(A-E) and radiographs(F) of patient with loosening teeth induced by severe periodontitis during operation (Maxillary) |
|
|
|
| 图 3 重度牙周炎致牙齿松动脱落患者术中口内照片(A-D)及X线片(E、F)(下颌) Figure 3 Intraoral photographs(A-D) and radiographs(E, F) of patient with loosening teeth induced by severe periodontitis during operation (Mandible) |
|
|

|
| 图 4 重度牙周炎致牙齿松动脱落患者二期术中(A-D)及修复后(E、F)的口内照片 Figure 4 Intraoral photographs of patient with loosening teeth induced by severe periodontitis during second stage operation (A-D) and after repair(E, F) |
|
|
重度牙周炎由于牙槽骨的严重破坏,往往伴有根分叉病变、牙髓病变、牙松动甚至脱落,重度牙周炎的治疗对牙周科医师是一种挑战[3]。目前,上颌或下颌前部美学区牙齿缺失的治疗方法包括可摘局部义齿、固定局部义齿和种植修复[4]。在排除局部或全身禁忌证的情况下,种植治疗通常被认为是部分或全部牙齿缺失的首选方法[5]。根据不同种植时机可以将种植手术分为延期种植和即刻种植[6]。传统的种植治疗,常采用延期种植[7]。研究[8]认为:拔牙后3个月到半年,牙槽骨吸收速度最快。但延期种植时间较长,这就造成延期种植时的骨量不足。1978年德国Tuebingen大学Schulte等[9]提出了即刻种植种植技术,即刻种植是指在拔牙的同时在牙槽窝内植入种植体[10],可以避免拔牙后出现的牙槽骨进行性骨吸收。研究[11]表明:即刻种植和延期种植存留率分别为98%和100%,在主观评估中,2组间比较差异无统计意义。在前牙种植治疗中,美学要求不仅要求有良好的植入物,还要有足够的软硬组织以达到自然的效果,而采用onlay植骨、膜技术、骨牵引和骨劈开可以实现骨增量[12]。研究[13]显示:骨增量技术可以形成足量的骨并恰当地植入骨缺损部位,并且,移植骨和骨缺损区之间可以有良好的接触和结合。Galav等[14]分别采用ABG和PRF治疗牙周病造成的骨缺损,9个月后所有参数明显提高。
本病例为重度牙周炎患者,在进行治疗方案设计时,对于牙周炎的治疗固然重要,但如何恢复其咀嚼发音功能及达到美学要求更是对临床医师的挑战,因此本文作者进行了多学科考虑。本病例通过牙周基础治疗控制牙周炎症,提高了手术的成功率。在手术时采用了即刻种植修复缺失的前牙。为了解决种植修复中骨量不足的问题,在即刻种植的基础上采用骨增量技术,在制订治疗方案时建议采用ABG,但患者拒绝接受,所以最终决定采用人工骨粉修复骨缺损。人工骨粉可以减少牙槽骨的吸收,尽可能地保存牙槽骨的骨量和形态[15]。由于前牙区存在广泛的牙龈退缩,为了恢复前牙美学,在治疗时拟采用膜龈手术增宽附着龈,但患者拒绝了游离龈移植手术。在治疗期间,由于患者的美学要求及修复科建议,将前牙美学区连续多颗牙进行了修复。在修复体材料选择时,本文作者考虑到非贵金属烤瓷冠尤其是镍铬合金烤瓷冠,在其义齿修复的冠边缘处牙龈常逐渐变成灰色或灰黑色,严重影响义齿美观,而贵金属烤瓷冠价格较高,难以普及[16]。氧化锆全瓷冠有较低的断裂率、良好的生物相容性和极佳的审美特性,是理想的美学修复材料[17]。因此采用了氧化锆全瓷修复体,并采用牙龈瓷修复缺损的牙龈组织。患者对最终的美学修复效果满意。复查维护治疗是种植修复的必要手段,长期的疗效观察有利于保持种植体周围软硬组织的稳定性,控制炎症的进展是种植修复成功的关键之一。本文作者通过牙周、牙体、种植和修复多学科联合治疗,成功实现了前牙区多颗牙缺失的美学修复,为多学科联合治疗伴有牙周软组织形态不良的复杂前牙美学问题提供了新思路,开辟了新途径。
| [1] | 祝岩, 万澎波, 赵伟. 上颌前牙美学区连续多颗牙缺失即刻种植的临床研究[J]. 口腔医学, 2016, 36(8): 700–705. |
| [2] | Rokn A, Bassir SH, Rasouli Ghahroudi AA, et al. Long-term stability of soft tissue esthetic outcomes following conventional single implant treatment in the anterior maxilla:10-12 year results[J]. Open Dent J, 2016, 16(10): 602–609. |
| [3] | Zhang J. Orthodintic the treatment of severe periodontitis[J]. Zhonghua Kouqiang Yixue Zazhi, 2017, 52(2): 65–66. |
| [4] | Raj R, Mehrotra K, Narayan I, et al. Natural tooth pontic:an instant esthetic option for periodontally compromised teeth-a case series[J]. Case Rep Dent, 2016, 2016: 8502927. |
| [5] | Alfaleh W. A radiographic study on the prevalence of knife-edge residual alveolar ridge at proposed dental implant sites[J]. Saudi Dent J, 2009, 21(1): 23–27. |
| [6] | Benavides E, Rios HF, Ganz SD, et al. Use of cone beam computed tomography in implant dentistry:the international congress of oral implantologists consensus report[J]. Implant Dent, 2012, 21(2): 78–86. DOI:10.1097/ID.0b013e31824885b5 |
| [7] | Urban IA, Jovanovic SA, Lozada JL, et al. Vertical ridge augmentation using guided bone regeneration (GBR) in three clinical scenarios prior to implant placement:a retrospective study of 35 patients 12 to 72 months after loading[J]. Int J Oral Maxillofac Implants, 2009, 24(3): 502–510. |
| [8] | Tan WL, Wong TL, Wong MC, et al. A systematic review of post-extractional alveolar hard and soft tissue dimensional changes in humans[J]. Clin Oral Implants Res, 2012, 23(Suppl 5): 1–21. |
| [9] | Schulte W, Kleineikenscheidt H, Lindner K, et al. The Tübingen immediate implant in clinical studies[J]. Dtsch Zahnarztl Z, 1978, 33(5): 348–359. |
| [10] | Strub JR, Jurdzik BA, Tuna T. Prognosis of immediately loaded implants and their restorations:a systematic literature review[J]. J Oral Rehabil, 2012, 39(9): 704–717. DOI:10.1111/joor.2012.39.issue-9 |
| [11] | Giannakopoulos NN, Ariaans K, Eberhard L, et al. Immediate and delayed loading of two-piece reduced-diameter implants with locator-analog attachments in edentulous mandibles:One-year results from a randomized clinical trial examining clinical outcome and patient expectation[J]. Clin Implant Dent Relat Res, 2017, 19(4): 643–653. DOI:10.1111/cid.2017.19.issue-4 |
| [12] | Rajput NS, Bhaskar J, Valiathan M, et al. Placement of dental implant in a knife edge ridge in anterior aesthetic zone[J]. J Clin Diagn Res, 2013, 7(10): 2376–2377. |
| [13] | D'Amato S, Tartaro G, Itro A, et al. Mandibular bone regeneration after bone slat technique[J]. Ann Stomatol (Roma), 2017, 8(1): 39–44. DOI:10.11138/ads/2017.8.1.039 |
| [14] | Galav S, Chandrashekar KT, Mishra R, et al. Comparative evaluation of platelet-rich fibrin and autogenous bone graft for the treatment of infrabony defects in chronic periodontitis:clinical, radiological, and surgical reentry[J]. Indian J Dent Res, 2016, 27(5): 502–507. DOI:10.4103/0970-9290.195634 |
| [15] | Yang HL, Zhu XS, Chen L, et al. Bone healing response to a synthetic calcium sulfate/β-tricalcium phosphate graft material in a sheep vertebral body defect model[J]. J Biomed Mater ResPart B Appl Biomater, 2012, 100(7): 1911–1921. |
| [16] | 任运佳, 孙淑芬, 张娟, 等. 镀金合金、镍铬合金和高金合金烤瓷冠的龈缘美学研究[J]. 吉林大学学报:医学版, 2010, 36(4): 753–757. |
| [17] | Qi B, He Y. Clinical evaluation of the zirconia all ceramic crowns in 40 consecutive patients[J]. Shanghai J Stomatol, 2016, 25(3): 364–367. |
 2018, Vol. 44
2018, Vol. 44


