扩展功能
文章信息
- 尹唯凰, 刘旸, 马晓周, 刘欣辰, 于子莹
- YIN Weihuang, LIU Yang, MA Xiaozhou, LIU Xinchen, YU Ziying
- 第一鳃弓综合征并发皮样囊肿1例报告及文献复习
- First branchial arch syndrome complicated with dermoid cyst:A case report and literature review
- 吉林大学学报(医学版), 2020, 46(05): 1078-1081
- Journal of Jilin University (Medicine Edition), 2020, 46(05): 1078-1081
- 10.13481/j.1671-587x.20200530
-
文章历史
- 收稿日期: 2019-10-29
2. 吉林大学第二医院关节外科, 吉林 长春 130041;
3. 吉林大学口腔医院牙体牙髓科, 吉林 长春 130021
2. Department of Orthopedics, Second Hospital, Jilin University, Changchun 130041, China;
3. Department of Endodontics, Stomatology Hospital, Jilin University, Changchun 130021, China
第一鳃弓综合征被称为眼-耳-脊柱综合征(oculo-auriculo-vertebral syndrome,OAVS)、面-耳-脊柱综合征和Goldenhar综合征(Goldenhar syndrome,GS)等[1],是以发育受损为特征的一系列疾病的总称,包括眼、耳、面部、口腔、骨骼发育异常以及中枢神经系统缺陷等[2]。外耳道畸形和颌骨发育不足是最常见的临床表现[3],但第一鳃弓综合征并发皮样囊肿少有报道。皮样囊肿位于颌面部时,通常发生于口底,其次是舌,临床症状不明显,若肿物缓慢增大可导致吞咽、发音和呼吸困难等。因此手术切除为第一鳃弓综合征首选治疗方法[4]。国外病例报道称第一鳃弓综合征可伴有眼球皮样囊肿[5],国内相关报道较少,而伴发面部皮样囊肿更为罕见。本文报道1例第一鳃弓综合征并发皮样囊肿病例,结合国内外相关报道,总结该病发生机制、临床表现、诊断和手术方法,为第一鳃弓综合征患者的临床诊断提供新思路。
1 临床资料 1.1 一般资料患者,女性,9岁。2019年6月21日因右面部无明显诱因肿胀,自行抗炎治疗4 d(药名不详)无效,肿胀缓慢加重,就诊于吉林大学口腔医院颌面外科,彩色超声检查结果显示右面颊部皮下囊实性病变,门诊以“右面部肿物”收入院。
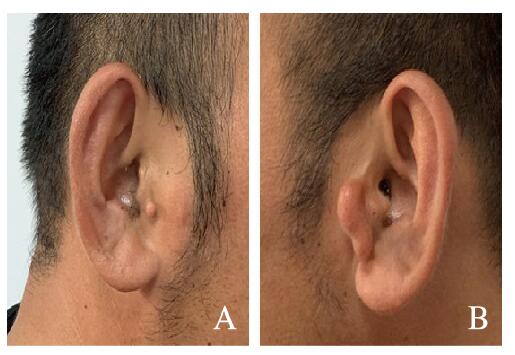
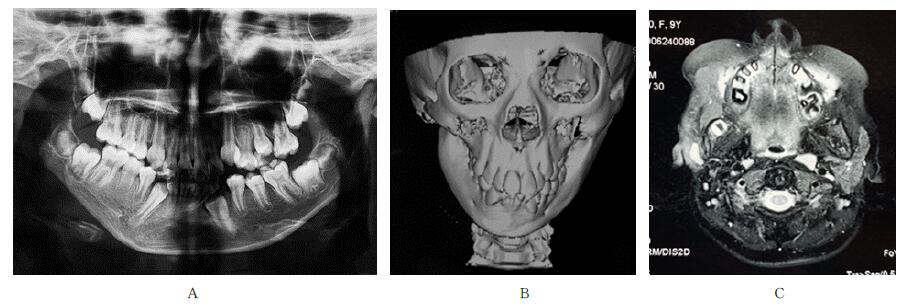
1.2 检查结果专科检查:面部左右不对称,右侧面部肿胀明显,表面可见窦道,挤压可见黄白色液体,触诊质地软,边界尚清,活动度良好,双侧腮腺咬肌区可见附耳(图 1,见插页八);右侧外耳道形态异常,右耳屏前有1个直径为0.5 cm的圆形赘生物,质软(图 1A,见插页八);右侧下颌角发育异常,偏颌。患者妹妹为多指畸形,其父亲左侧外耳道畸形,耳屏形态异常,右侧耳屏前有1个圆形赘生物(图 2,见插页八)。曲面断层及颌骨三维CT检查结果显示:颌骨发育不全,右侧下颌升支后份及髁状突部分骨质缺如(图 3A和B)。颌面部MRI检查结果显示:右侧腮腺体积较对侧缩小(图 3C),其内可见条状呈T1长T2信号影,边界清晰,右侧咀嚼肌前外方可见片状异常信号影,T1WI和T2压脂呈等信号,与正常腮腺组织信号类似,其内可见类圆形异常信号影,T1WI呈低信号,T2WI呈高信号,DWI呈高信号,ADC呈稍高信号。

|
| A: Right side; B: Left side. 图 1 第一鳃弓综合征并发皮样囊肿患者右侧耳屏异常及双侧附耳图像 Fig. 1 Photos of abnormal right tragus and preauricular appendages from both sides of patient with first branchial arch syndrome complicated with dermoid cyst(seen on page 1079 in paragraph) |
|
|
|
| A: Right side; B: Left-side. 图 2 第一鳃弓综合征并发皮样囊肿患者父亲右侧耳前赘生物及左侧耳屏形态异常图像 Fig. 2 Photos of right preauricular excrescence and dabnormal left tragusof father of patient with first branchial arch syndrome complicated with dermoid cyst (seen on page 1079 in paragraph) |
|
|
|
| A: Pantomography image; B: 3D-CT reconstruction image; C:MRI image 图 3 第一鳃弓综合征并发皮样囊肿患者曲面断层、头部CT和MRI影像 Fig. 3 PPantomography, head CT and MRI images of patient with first branchial arch syndrome complicated with dermoid cyst |
|
|
经临床、影像学和病理学检查诊断:①第一鳃弓综合征;②右面部皮样囊肿。
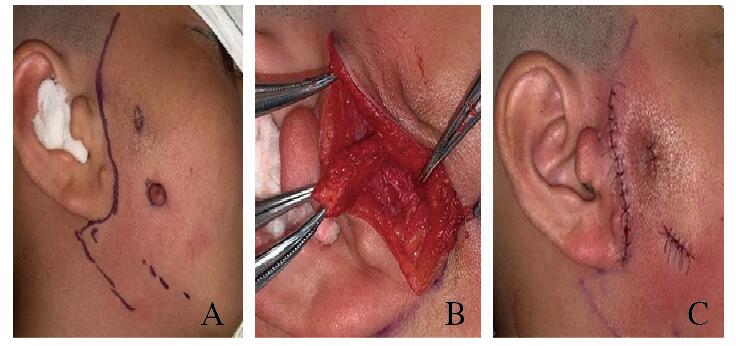
1.4 治疗方法术前全面检查,未见手术禁忌证,于手术室全麻下摘除囊肿并切除面部赘生物。手术于右侧耳前画常规“S”形切口线(图 4A,见插页八),常规切开皮肤和皮下组织,见腮腺腺体萎缩,部分区域肿物似肉芽组织,红褐色,质地脆,边界不清,瘘管下方至外耳道软骨可见一条索,边界尚清(图 4B,见插页八),沿其外侧分离,充分保护面神经,于瘘管表面皮肤行梭形切口,完整切除肿物,于面颊部附耳周围行梭形切口,完整切除附耳(图 4C,见插页八)。
|
| A: Preoperative view; B: Intraoperative view; C: Postoperative view. 图 4 第一鳃弓综合征并发皮样囊肿患者手术图像 Fig. 4 Photos of operation of patient with first branchial arch syndrome complicated with dermoid cyst(seen on page 1080 in paragraph) |
|
|
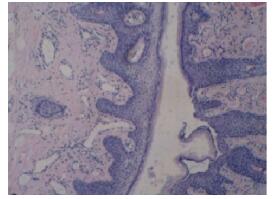
术后病理切片光学显微镜下观察显示:纤维结缔组织囊壁内衬复层过度正角化上皮,囊壁内见毛囊。病理学诊断考虑为右面部皮样囊肿(图 5,见插页八)。
|
| 图 5 第一.鳃弓综合征并发皮样囊肿患者术后皮样囊肿组织病理形态表现(HE, X400) Fig. 5 Pathomorphology of dermoid cyst tissue of patient with first branchial arch syndrome complicated with dermoid cyst after surgery(HE, . X 400)(seen on page 1080 in paragraph) |
|
|
第一鳃弓综合征是以颅颌面发育障碍为主要特征的疾病,发病率约为1/3 500[6]。其发病机制尚不明确,但研究[1]认为遗传因素和环境因素与其发生有关,其临床表现多样:①眼。双眼不对称、眼睑下垂、缺损或眼裂过小、眼球皮样囊肿、泪囊炎和眼球运动障碍等。②耳。耳前附件、耳前瘘管、耳廓畸形、小耳畸形、无耳畸形、耳不对称、外耳道闭锁、伴或不伴有听力损害的耳发育不良、中耳或内耳异常。③面部。上下颌骨发育不全、错畸形、面部不对称、半侧颜面部短小畸形、大口畸形、面裂、唇裂、腭裂、偶有腮腺缺失或涎腺瘘。④口腔。裂舌、牙齿异常(多生牙、牙釉质和牙本质发育异常)和牙齿发育迟缓。⑤骨骼。脊椎裂、小头畸形和畸形足等。⑥内脏。心脏和肾脏异常等。⑦中枢神经系统缺陷[2]。还有部分患者临床表现为颈椎异常[7]、眼球表皮样囊肿[8]、生殖系统异常[9]和肛门闭锁[10]。国外有文献报道第一鳃弓综合征伴有眼球皮样囊肿[8],但尚无发生于颌面部皮样囊肿的相关报道。第一鳃弓综合征包含多学科疾病,因此在治疗时要根据患者的年龄、病变范围、异常程度和严重程度进行早期、长期甚至跨学科治疗[11]。一般情况下,消化道异常在新生儿出生最初几个小时内出现,需要及时进行外科手术。若发生在颅颌面部,可表现为面裂、唇裂、腭裂、腭咽闭合不全和面部短小。需建立持久的、阶段性治疗计划,年龄较大的患儿可能需要应用咽部皮瓣来改善语音质量。出于美学考虑,可以在早期去除耳前附属物。患有面横裂、唇裂和腭裂的患儿通常需要在适当的年龄进行多次手术,一般在3个月时行唇裂修复[12],在9个月至2年内行腭裂修复[13]。下颌骨发育畸形是第一鳃弓综合征的主要临床表现,临床治疗方法包括:①骨移植。包括肋骨、肋软骨和髂骨移植,用于延长下颌骨,重建下颌支和颞下颌关节。但可能存在移植骨不可预测的增长,过度增长会使面部不对称[14],同时也增加感染和移植物排斥的风险[15]。②截骨术。截骨术是一种大型外科手术,存在多种并发症,包括愈合不良、咬合恢复不良和损伤神经出现感觉异常等症状[14]。上述2种方法由于手术风险较高、创伤较大,不适用于本例患者。③全颞下颌关节假体置换术。通过计算机断层扫描获取数据重建全颞下颌关节假体。该术式具有咬合稳定性,改善颞下颌关节功能,改善面部平衡,具有较好的舒适性和可预测性。但仍存在假体使用寿命未知、感染和患者对假体材料过敏等局限性[16]。④牵张成骨术。适用于年轻患者,可以同时延长颌骨和扩张软组织,治疗过程中可调节,复发率低[17]。在设计颌骨畸形的手术治疗方案时,应充分考虑患儿家属的经济和风险承受能力。对于本例患儿,根据家属要求,仅手术摘除右侧面部皮样囊肿和右侧耳前赘生物,医生仍建议患者及其家属尽早行颌骨畸形的治疗,以减少面部畸形对患者发育和身心健康的影响。另外,建议患儿家属到综合医院就诊,排除第一鳃弓综合征伴发其他系统性疾病,做到早发现、早诊断和早治疗。
综上所述,皮样囊肿是一种非牙源性疾病,临床上少见,很少累及颌面部,占全身皮样囊肿的1.6%~7.0%[18]。其发病机制目前有2种学说:①胚胎发育第3~4周,第一鳃弓和第二鳃弓融合时,中线外胚层细胞向深部组织进入导致发育畸形形成囊肿[19]。②创伤性植入。手术摘除是治疗皮样囊肿最有效的方法,位于下颌舌骨肌上方的囊肿一般采用口内切口,若囊肿位于口底,因其术后感染肿胀时可能干扰气道影响呼吸而采用口外切口[20]。较大囊肿可抽吸部分内容物减压后手术摘除。本例患儿囊肿位于右侧腮腺咬肌区,故采用右侧耳前“S”形切口线,显露该区域,完整摘除囊壁组织和瘘管以减少复发风险。
| [1] |
AIZENBUD D, SHOHAM N V, CONSTANTINI S, et al. Goldenhar syndrome and medulloblastoma: a coincidental association? The first case report[J]. J Craniomaxillofac Surg, 2014, 42(5): e91-e96. DOI:10.1016/j.jcms.2013.07.003 |
| [2] |
BOGUSIAK K, PUCH A, ARKUSZEWSKI P. Goldenhar syndrome: current perspectives[J]. World J Pediatr, 2017, 13(5): 405-415. DOI:10.1007/s12519-017-0048-z |
| [3] |
BELEZA-MEIRELES A, HART R, CLAYTON-SMITH J, et al. Oculo-auriculo-vertebral spectrum: clinical and molecular analysis of 51 patients[J]. Eur J Med Genet, 2015, 58(9): 455-465. DOI:10.1016/j.ejmg.2015.07.003 |
| [4] |
VIEIRA E M, BORGES A H, VOLPATO L E, et al. Unusual dermoid cyst in oral cavity[J]. Case Rep Pathol, 2014, 2014: 389752. |
| [5] |
AL-KZAYER L F Y, SARSAM S N, ALHUR N Y, et al. Asymmetrically enlarged parietal foramina in a rare case of Goldenhar syndrome with a possible etiopathogenesis[J]. Oncotarget, 2018, 9(2): 2962-2968. DOI:10.18632/oncotarget.23479 |
| [6] |
BELEZA-MEIRELES A, CLAYTON-SMITH J, SARAIVA J M, et al. Oculo-auriculo-vertebral spectrum: a review of the literature and genetic update[J]. J Med Genet, 2014, 51(10): 635-645. DOI:10.1136/jmedgenet-2014-102476 |
| [7] |
KABAK S L, SAVRASOVA N A, ZATOCHNAYA V V, et al. Hemifacial microsomia: skeletal abnormalities evaluation using CBCT (case report)[J]. J Radiol Case Rep, 2019, 13(11): 1-9. |
| [8] |
JAHANIMOGHADAM F, SHARIFI M. Goldenhar syndrome in a 6-year-old patient: a case report and review of literature[J]. J Dent Shiraz Iran, 2019, 20(4): 298-303. |
| [9] |
BENJAMIN J C. Goldenhar syndrome associated with genital tract abnormality[J]. BMJ Case Rep, 2019, 12(8): e230686. |
| [10] |
SHARAWAT I K, BHATTACHARYA D, SAINI L. Goldenhar syndrome with imperforate anus: new association or coincidence![J]. Indian J Pediatr, 2019, 86(12): 1150. DOI:10.1007/s12098-019-03038-8 |
| [11] |
KUSHWAHA R K, SINGH A, MOHTA A, et al. Goldenhar syndrome: A report of two cases[J]. Indian Dermatol Online J, 2019, 10(6): 719-720. DOI:10.4103/idoj.IDOJ_491_18 |
| [12] |
ZHANG J X, ARNEJA J S. Evidence-based medicine: the bilateral cleft lip repair[J]. Plast Reconstr Surg, 2017, 140(1): 152e-165e. |
| [13] |
SHKOUKANI M A, LAWRENCE L A, LIEBERTZ D J, et al. Cleft palate: a clinical review[J]. Birth Defects Res Part C Embryo Today, 2014, 102(4): 333-342. DOI:10.1002/bdrc.21083 |
| [14] |
WAN D C, TAUB P J, ALLAM K A, et al. Distraction osteogenesis of costocartilaginous rib grafts and treatment algorithm for severely hypoplastic mandibles[J]. Plast Reconstr Surg, 2011, 127(5): 2005-2013. DOI:10.1097/PRS.0b013e31820cf4d6 |
| [15] |
FATTAH A Y, CARO C, KHECHOYAN D Y, et al. Cephalometric outcomes of orthognathic surgery in hemifacial microsomia[J]. J Craniofac Surg, 2014, 25(5): 1734-1739. DOI:10.1097/SCS.0000435808.91512.58 |
| [16] |
WOLFORD L M, BOURLAND T C, RODRIGUES D, et al. Successful reconstruction of nongrowing hemifacial microsomia patients with unilateral temporomandibular joint total joint prosthesis and orthognathic surgery[J]. J Oral Maxillofac Surg, 2012, 70(12): 2835-2853. DOI:10.1016/j.joms.2012.02.010 |
| [17] |
PLUIJMERS B I, CARON C J, DUNAWAY D J, et al. Mandibular reconstruction in the growing patient with unilateral craniofacial microsomia: a systematic review[J]. Int J Oral Maxillofac Surg, 2014, 43(3): 286-295. DOI:10.1016/j.ijom.2013.11.001 |
| [18] |
KUMAR N G, ARORA S S, KUMAR I, et al. Dermoid cysts of the maxillofacial region: case series[J]. J Maxillofac Oral Surg, 2019, 18(2): 238-244. DOI:10.1007/s12663-018-1129-9 |
| [19] |
LIMA S M JR, CHRCANOVIC B R, DE PAULA A M, et al. Dermoid cyst of the floor of the mouth[J]. Sci World J, 2003, 3: 156-162. DOI:10.1100/tsw.2003.04 |
| [20] |
LONGO F, MAREMONTI P, MANGONE G M, et al. Midline (dermoid)cysts of the floor of the mouth: report of 16 cases and review of surgical techniques[J]. Plast Reconstr Surg, 2003, 112(6): 1560-1565. DOI:10.1097/01.PRS.0000086735.56187.22 |
 2020, Vol. 46
2020, Vol. 46

