扩展功能
文章信息
- 刘科琳, 邹莹, 王君, 裴颖
- LIU Kelin, ZOU Ying, WANG Jun, PEI Ying
- 太田痣并发青光眼睫状体炎综合征1例报告及文献复习
- Nevus of ota complicated with Posner-Schlossman syndrome:A case report and literature review
- 吉林大学学报(医学版), 2020, 46(05): 1074-1077
- Journal of Jilin University (Medicine Edition), 2020, 46(05): 1074-1077
- 10.13481/j.1671-587x.20200529
-
文章历史
- 收稿日期: 2020-01-12
太田痣(nevus of ota)病因和发病机制目前尚不清楚,临床诊断较为简单,根据临床表现多能明确诊断。三分之二的太田痣患者出生时存在眼部损害,部分患者可在10余年后出现皮肤损害,极少数患者会发生脉络膜及脑部恶性黑素瘤[1]。眼部表现常并发眼压增高,引起继发性青光眼。太田痣在日本发病率高达0.3%~1.0%[2],在我国人群中,太田痣的发病率也达到0.1%~0.2%[3]。青光眼睫状体炎综合征(Posner-Schlossman syndrome,PSS)是一种好发于青壮年的眼科疾病,太田痣患者在临床表现上虽然可以出现眼部受损症状发生继发性青光眼,但太田痣并发PSS较为少见,国内外文献尚未见此类报道。本院眼科门诊青光眼诊室收治1例太田痣并发PSS患者,现对其临床特点进行分析,并对太田痣和PSS相关文献进行复习,旨在提高临床医生对该疾病的认识,为太田痣并发PSS的诊治提供参考。
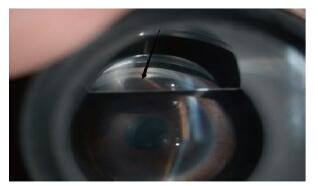
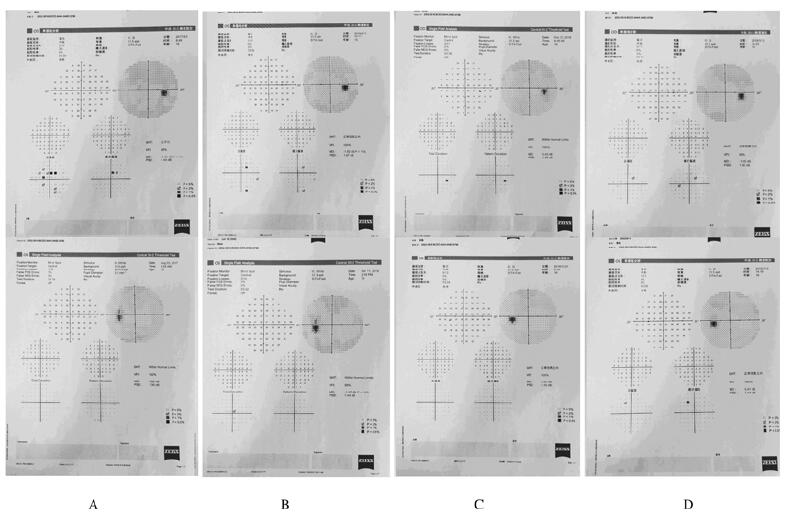
1 临床资料患者,男性,15岁,因“右眼视物模糊、眼红”于2017年8月13日就诊于吉林大学第二医院眼科门诊。患者自述曾于外院行3次颜面部激光治疗。查体:右眼视力0.1,右眼眼压46 mmHg,右侧额部、眼睑全周和颊面部可见蓝黑色色素斑块(图 1,见插页七);裂隙灯显微镜下检查示右眼球结膜充血,巩膜全周可见黑色素沉积(图 2,见插页七)(因巩膜全周色素沉积,图片中球结膜充血不易观察);角膜水肿,角膜后可见3个孤立羊脂状角膜后沉积着物(keratic precipitates,KPs)(图 3,见插页七);房角镜检查示房角开放,小梁网及睫状体带大量色素沉积(图 4,见插页八)。前房深浅大致正常,瞳孔正圆,直径约3.0 mm,虹膜纹理清,可见颜色加深,晶体透明,玻璃体透明;眼底检查示黄斑中心凹反光清,视盘界清色淡红,杯盘比约0.3;双眼视野未见异常(图 5A)。门诊诊断:太田痣并发PSS。给予抗炎及降眼压药物治疗,2周后复查,右眼视力1.0,右眼眼压14 mmHg。随后的2次复查,视力、眼压和视野均无异常(图 5B和C)。19个月后上述症状复发,查体:右眼视力0.4,右眼眼压35 mmHg,眼部检查同上,视野未见异常(图 5D)。超声生物显微镜(ultrasound biomicroscope,UBM)检查示:右眼前房可见点状回声,双眼前房深浅大致正常,右眼前房深度为2.74 mm,左眼前房深度为2.75 mm,双眼房角开放,虹膜平坦,右眼虹膜回声较左眼回声增强,双眼睫状体未见明显异常(图 6,见插页八)。再次给予降眼压及抗炎药物治疗,上述症状好转。
|
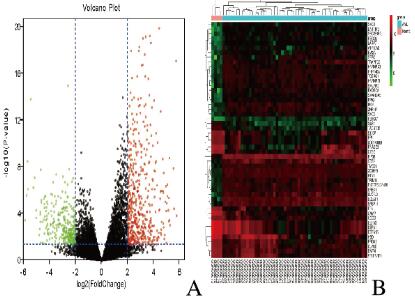
| A: Red represented the up-regulated genes, green represented the down-regulated gene, and black was the gene with no significant difference; B: Genes up-regulated were in red, genes, down-regulated were in green, and genes without any significant difference were in black. The diffe erences were set as corrected P value < 0. 05 and log |FC| ≥2. 图 1 小儿AML患者与正常对照样本.DEGs的火山图(A)和前50个DEGs的热点图(B) Fig. 1 Volcano plots(A)and | hea tmap (B) of top 50 DEGs of AML patients and normal controls(seen on page 1038 in paragraph) |
|
|
|
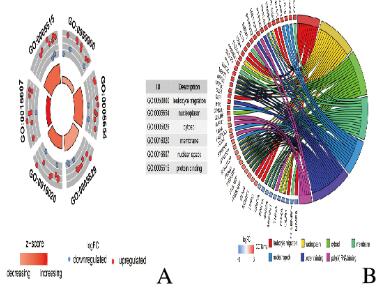
| A:The outer circle represented the expression of DEGs in each enriched GO term, red dots. on each GO term indicated up-regulated genes and blue dots indicated down-regulated genes. The inner circle indicated the significance of GO terms; B: The circle indicated the top 7 functional clusters in their gene ontology terms. 图 2 DEGs的GO富集分析 Fig. 2 GO enrichment analysis of DEGs(seen on page 1038 in paragraph) |
|
|
|
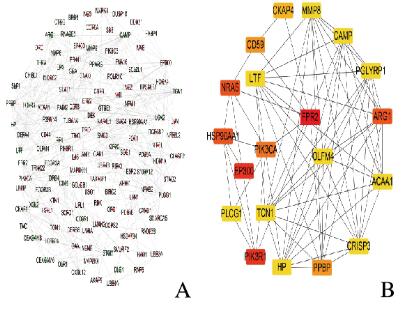
| A: Green nodes represented down-regulated genes, and red nodes represented up-regulated genes; B: Hub genes analyzed by cytoHubba in Cytoscape softw ware. 图 3 DEGs的PPI网络构建和Hub基因筛选 Fig. 3 PPI network construction and nd Hub gene screening of DEGs(seen on page 1038 in paragraph) |
|
|
|
| 图 4 太田痣综合征并发PSS患者房角镜观察结果. Fig. 4 Observation1 result of gonioscope of patient with nevus of ota complicated with PSS (seen on page 1075 in paragraph) |
|
|
|
| A:Initial visual field examination; B, C: Visual field reexamination; D: Visual field examination after recurrence. 图 5 太田痣并发PSS患者视野照片图 Fig. 5 Perimetry images of patient with nevus of ota complicated with PSS |
|
|

|
| 图 6 太田痣综合征并发PSS患者UBM观察结果 Fig. 6 Observation result of UMB of patient with nevus . of ota complicated with PSS .(seen on page 1075 in paragraph) |
|
|
太田痣又被称眼上腭褐青色痣,或眼皮肤黑素细胞增生病(oculoder-mamelanocytosis)[1]。OTA和TONINO两位学者于1939年首次提出并记录[4]。该病好发于女性,多在出生时发病,常为单侧发病,偶见双侧受累,其发病机制尚不明确,目前比较认可的发病机制是由于胚胎时期黑色素细胞凋亡异常、从真皮向表皮迁移受阻以及真皮内黑色素产生异常,还有研究[5]认为与基因突变、内分泌激素水平以及精神因素有关。太田痣临床表现主要波及同侧面部三叉神经第一、二支支配的部位,表现为蓝灰色或蓝黑色色素斑片,鼓膜、眼和鼻等部位可累及[6]。
PSS是前部葡萄膜炎伴青光眼的一种特殊形式,是一种常于20~50岁青壮年发病的继发性青光眼[7]。PPS发病机制尚不清楚,目前关于其发病机制主要包括感染[8]、基因易感性[9]、房水细胞因子[10]和血管内皮功能异常[11]等多种学说。病毒感染是近年来PSS发病机制探讨的热点[8, 12-13],研究[8]显示:幽门螺旋杆菌(Helicobacter pylori,HP)、单纯疱疹病毒(herpes simplex virus,HSV)和巨细胞病毒(cytomegalovirus,CMV)感染在PSS的发病机制和发展过程中起到一定的作用。PSS患者一般自觉症状较少或仅出现轻度症状,可有眼前节轻度炎症,具有单眼反复发作的轻度非肉芽肿性睫状体炎伴眼压升高的特点,眼压可达40~60 mmHg,可引起角膜水肿,但通常对视力影响较小[7]。PSS临床表现一般在发作3 d内出现KPs,常呈羊脂状,典型KPs多为细小、无色素和边界清楚的羊脂状,通常数目不多,约1~10颗不等,多沉积在角膜下1/3部位[14]。普遍认为青光眼睫状体炎综合征具有良性病程及预后,但部分患者可能出现继发性视神经损害和视野缺损的情况[13]。葡萄膜炎继发青光眼在临床表现上与PSS患者相似,其特点是病情反复发作,疾病早期药物治疗效果好,多次反复发作后,可能出现药物治疗效果不佳,患者最终产生青光眼相关视神经及视野改变,常被误诊为PSS,因此在诊断PSS时需要与葡萄膜炎继发青光眼进行鉴别诊断[15]。临床上接诊青壮年不明原因的单眼发作性视物模糊伴眼压升高而前房又不浅时,应提高警惕,考虑PSS的可能,典型的KPs在诊断过程中是不可或缺的证据[7]。本例太田痣并发PSS患者,巩膜周围及房角沉积大量色素,诊断时应与太田痣并发色素性青光眼进行鉴别诊断。色素性青光眼同样是一种继发性青光眼,多由色素播散综合征引起,Krukenberg色素梭、小梁网色素沉积及虹膜透照缺损是色素播散综合征最具特征性的临床体征,也称为“色素播散三联征”[16]。PSS多无眼前节炎症反应,可通过询问病史及相关眼部检查与本例太田痣并发PSS患者进行鉴别诊断。
综上所述,太田痣相关文献报道多见,并发青光眼的病例国内外也有部分报道[17-18],PSS为眼科常见病,国内外文献报道较多,太田痣并发PSS的病例目前国内尚未见类似报道。本病例采用局部激素及降眼压药物等临床对症治疗,效果较好。因患者年龄较小,且曾复发过1次,以后是否存在复发可能以及药物治疗是否有效仍需要密切随诊、跟踪。分析本病例的确诊及治疗旨在为眼科临床工作者提供更多的资料及一定的参考。
| [1] |
张建中, 高兴华. 皮肤性病学[M]. 3版. 北京: 人民卫生出版社, 2015: 320.
|
| [2] |
孙鑫. 调Q开关Nd:YAG激光治疗太田痣80例疗效观察[J]. 中国美容医学, 2010, 19(3): 370. DOI:10.3969/j.issn.1008-6455.2010.03.028 |
| [3] |
管青.太田痣和获得性双侧太田痣样斑发病特征及激光治疗效果的评估[D].重庆: 第三军医大学, 2012.
|
| [4] |
曾颖, 董继英, 王棽, 等. 太田痣激光治疗的进展[J]. 中国激光医学杂志, 2018, 27(3): 178-182. |
| [5] |
郎小乔, 刘华绪, 周桂芝, 等. 不典型太田痣一例[J]. 中国麻风皮肤病杂志, 2019, 35(7): 432-433. |
| [6] |
张凯, 姬瑜. 太田痣的激光治疗进展[J]. 中国麻风皮肤病杂志, 2015, 31(9): 543-545. |
| [7] |
葛坚, 王宁利. 眼科学[M]. 3版. 北京: 人民卫生出版社, 2015: 284.
|
| [8] |
陈文杰, 赵军, 祝天辉, 等. 青光眼睫状体炎综合征患者5种常见病原微生物相关血清抗体的测定及分析[J]. 中华实验眼科杂志, 2017, 35(12): 1115-1119. |
| [9] |
ZHAO J, ZHU T H, CHEN W J, et al. Human leukocyte antigens-B and -C loci associated with posner-schlossman syndrome in a southern Chinese population[J]. PLoS One, 2015, 10(7): e0132179. |
| [10] |
OHIRA S, INOUE T, IWAO K, et al. Factors influencing aqueous proinflammatory cytokines and growth factors in uveitic glaucoma[J]. PLoS One, 2016, 11(1): e0147080. |
| [11] |
SHEN S C, HO W J, WU S C, et al. Peripheral vascular endothelial dysfunction in glaucomatocyclitic crisis:a preliminary study[J]. Investig Ophthalmol Vis Sci, 2010, 51(1): 272-276. DOI:10.1167/iovs.09-3849 |
| [12] |
许欢, 翟如仪, 孔祥梅, 等. 青光眼睫状体炎综合征患者房水病毒情况分析[J]. 中国眼耳鼻喉科杂志, 2018, 18(1): 18-21. |
| [13] |
孙嫣然, 党亚龙. 青光眼睫状体炎综合征病因学研究新进展[J]. 中华实验眼科杂志, 2016, 34(10): 957-960. |
| [14] |
叶天才, 王宁利. 临床青光眼图谱[M]. 北京: 人民卫生出版社, 2007: 338.
|
| [15] |
李树宁. 青光眼睫状体炎综合征的临床思考[J]. 中华眼科医学杂志(电子版), 2013, 3(4): 201-203. |
| [16] |
卿国平, 王宁利. 色素播散综合征和色素性青光眼[J]. 眼科, 2013, 22(1): 10-13. |
| [17] |
LIU J C, BALL S F. Nevus of Ota with glaucoma:report of three cases[J]. Ann Ophthalmol, 1991, 23(8): 286-289. |
| [18] |
郑玥, 宋之都, 王锐, 等. 太田痣继发青光眼治疗二例[J]. 中国实用眼科杂志, 2012, 30(3): 356, 358. |
 2020, Vol. 46
2020, Vol. 46


