扩展功能
文章信息
- 杨逸铭, 刘玉品, 周懂晶, 陈志远, 萧焕明, 池晓玲
- YANG Yiming, LIU Yupin, ZHOU Dongjing, CHEN Zhiyuan, XIAO Huanming, CHI Xiaoling
- 3.0TMRIPDFF和IP-OP对脂肪肝定量评估的价值
- Values of 3.0T MRI PDFF and IP-OP in quantificative evaluation on fatty liver
- 吉林大学学报(医学版), 2020, 46(04): 875-880
- Journal of Jilin University (Medicine Edition), 2020, 46(04): 875-880
- 10.13481/j.1671-587x.20200434
-
文章历史
- 收稿日期: 2019-07-21
脂肪肝是一种常见的临床疾病,从病因上可分为非酒精性脂肪肝(non-alcoholic fatty iver disease,NAFLD)和酒精性肝病(alcohol related liver disease,AFLD),其中前者已成为全世界慢性肝病最常见的病因[1-2]。单纯脂肪肝如未得到有效控制可进展为肝纤维化和肝硬化,甚至发生肝细胞癌[3-4]。因此动态监控脂肪肝的发生发展过程具有重要的临床意义。目前诊断肝脏脂肪含量的金标准是肝脏穿刺活检,但是其为有创性检查,并且具有依从性差、有抽样误差和观察者间的不一致等局限性[5-6]。磁共振成像(magnetic resonance imaging,MRI)由于其无创性、分辨率高和多序列等优势,被认为是肝脏脂肪定量的最佳方法,如MRI同反相位(in-phase and opposed-phase,IP-OP)技术,已被广泛用于肝脏脂肪变的定性分析[7]。MRI质子密度脂肪分数(proton density fat-fraction,PDFF)是一种检测肝脏脂肪含量的MRI新技术,研究[8-9]显示:MRI-PDFF对于肝脏脂肪定量分析具有较高的稳定性、可重复性和精确度。但上述肝脏脂肪定量分析的研究都是通过单一的方法进行的,结果缺乏对照分析。本研究采用MRI-PDFF和MRI-IP-OP 2种技术分别与肝脏穿刺活检结果进行对比分析,探讨MRI-PDFF和MRI-IP-OP定量检测肝脏脂肪含量的应用价值,为脂肪肝无创性定量分析提供参考依据。
1 资料与方法 1.1 研究对象及纳入和排除标准本次回顾性研究得到了本医院伦理委员会的批准。收集从2015年12月—2018年8月于本院就诊,经穿刺活检证实,并临床诊断为脂肪肝患者的病例资料。
纳入标准:①MRI检查序列包括MRI-PDFF和MRI-IP-OP序列。②MRI检查与肝脏穿刺活检时间间隔少于1个月。③临床及实验室检查资料完整,临床资料包括年龄、体质量、身高、吸烟史、饮酒史、既往病史和家族史等,实验室检查结果包括血清肝功能指标、胆汁酸、甘油三酯和总胆固醇等。排除标准:①酗酒史(饮酒折合乙醇量,男性>140 g/周,女性>70 g/周)。②患有肝脏肿瘤、自身免疫性肝病等其他弥漫性肝脏病变及原发性硬化性胆管炎等胆道疾病。③有MRI检查禁忌证。最终共63例患者纳入本研究,其中男性43例,女性20例,年龄16~72岁,平均年龄(40.62±11.24)岁。轻度脂肪肝34例,中重度脂肪肝29例。同时选择血脂正常、临床诊断非脂肪肝患者(胃炎和功能性胃肠病等)20例作为对照组。
1.2 检查方法Toshiba公司Vantage Titan 3.0T MRI表面8通道相控阵线圈,仰卧位头脚方向扫描,扫描参数:梯度回波3D序列(FE3D),水脂分离技术(WFS),横断位(axial),重复时间(TR)最少5.1min,回波时间(TE) 1.1 ms/2.8 ms,激励次数(NAQ) 1,视野(FOV) 38cm×40cm,层数(slice) 28,层厚(thick) 8mm,翻转角(flip) 12°,扫描时间15s,相位编码方向的并行采集因子(speeder PE)2。
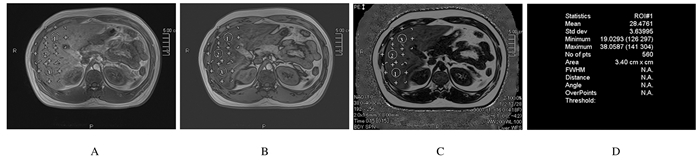
1.3 图像分析和后处理采用Toshiba Vitrea FX图像后处理工作站进行图像后处理。MRI-PDFF可在图像上直接测量感兴趣区(region of interest,ROI),得出肝脏脂肪分数(hepatic fat fraction,HFF)。由于本研究中患者肝脏穿刺活检位置位于右侧腋前线至锁骨中线7~9肋,为尽量与肝脏穿刺位置一致,本研究ROI选择肝Ⅳ、Ⅴ和Ⅵ段。ROI分别由2位有临床诊疗经验的放射科医师,远离肝脏边缘、避开大血管、大胆管于肝Ⅳ、Ⅴ和Ⅵ段各放置1个ROI(图 1),ROI>2 cm2,每个ROI测量3次取平均值,HFF取所测ROI平均值。
|
| A:In-phase image of liver; B:Out-phase image of liver; C:Liver fat fraction image; D:HFF (28.48%). 图 1 中度脂肪肝患者MRI图像 Fig. 1 MRI images of patient with moderate fatty liver |
|
|
MRI-IP-OP采用信号强度(signal intensity,SI)进行半定量分析。HFF=(SIin-SIout)/2SIin,SIin为同相位像肝脏信号强度,SIout为反相位图像上肝脏信号强度。MRI-IP-OP图像选取与MRI-PDFF同一层面上的同一位置,所有ROI大小尽量保持一致,每个ROI测量3次取平均值,HFF取所测ROI平均值。
1.4 统计学分析采用SPSS 20.0统计软件进行统计学分析。各组患者HFF值以x±s表示,采用Kolmogorov-Smirnov检验进行正态性检验。符合正态分布则多组间比较采用单因素方差分析,组间两两比较采用LSD法;不符合正态分布则多组间比较采用Kruskal-Wallis检验,组间两两比较采用Mann-Whitney检验,并进行Bonferroni校正。采用受试者工作特征(receiver operating characteristic,ROC)曲线的曲线下面积(area under curve,AUC)分析MRI-PDFF和MRI-IP-OP对脂肪肝的诊断效能,并计算灵敏度、特异度和阈值。以P < 0.05为差异有统计学意义。
2 结果 2.1 各组患者的HFF各组患者MRI-PDFF和MRI-IP-OP的HFF见表 1。中度脂肪肝患者MRI图像见图 1。经Kolmogorov-Smirnov检验,MRI-PDFF总体HFF不符合正态分布(Z=0.203,P < 0.01),MRI-IP-OP总体HFF值不符合正态分布(Z=0.209,P < 0.01)。采用Kruskal-Wallis检验比较各组患者HFF,各组患者MRI-PDFF和MRI-IP-OP的HFF组间比较差异有统计学意义(H=52.84,P < 0.01;H=45.50,P < 0.01)。采用Mann-Whitney U检验对各组患者HFF进行两两比较,并经Bonferroni校正,中重度脂肪肝组患者MRI-PDFF的HFF明显高于对照组和轻度脂肪肝组(Z=-4.40,P < 0.01;Z=-7.13,P < 0.01),轻度脂肪肝组患者MRI-PDFF的HFF高于对照组(Z=-3.44,P=0.002)。肪肝组患者MRI-IP-OP的HFF值高于对照组和轻度脂肪肝组(Z=-6.55,P < 0.01;Z=-4.51,P < 0.01),轻度脂肪肝组患者MRI-IP-OP的HFF高于对照组(Z=-2.71,P=0.02)。
| (x±s, η/%) | |||||||||||||||||||||||||||||
| Group | n | MRI-PDFF | MRI-IP-OP | ||||||||||||||||||||||||||
| Control | 20 | 4.57±1.48 | 5.22±1.85 | ||||||||||||||||||||||||||
| Mild fatty liver | 34 | 7.81±3.20** | 8.09±3.64* | ||||||||||||||||||||||||||
| Moderate and severe fatty liver | 29 | 19.80±8.84*△ | 19.56±8.48**△ | ||||||||||||||||||||||||||
| H | 52.84 | 45.50 | |||||||||||||||||||||||||||
| P | < 0.01 | < 0.01 | |||||||||||||||||||||||||||
| * P < 0.05,* * P < 0.01 compared with control group;△ P < 0.01 compared with mild fatty liver group. | |||||||||||||||||||||||||||||
采用MRI-PDFF技术诊断不同程度脂肪肝的ROC曲线显示:MRI-PDFF诊断轻度脂肪肝(对照组vs轻度脂肪肝+中重度脂肪肝)HFF阈值为5.1%,AUC为0.931(P < 0.01),灵敏度为90.0%,特异度为92.1%;MRI-PDFF诊断中重度脂肪肝(对照组+轻度脂肪肝组vs中重度脂肪肝组)HFF阈值为12.0%,AUC为0.928(P < 0.01),灵敏度为94.4%,特异度为75.9%。见图 2(插页十)和表 2。

|
| (seen on page 877, 878 in paragraph) 图 2 MRI-PDFF和MRI-IP-OP诊断轻度脂肪肝(A)和中重度脂肪肝(B)的ROC曲线 Fig. 2 ROC curves of MRIPDFF and MRI-IP-OP in diagnosis of mild fatty liver(A) and moderate to severe fatty liver(B) |
|
|
| Group | AUC | P | Cut off (η/%) | 95%CI | Sensitivity (η/%) | Specificity (η/%) | |
| Low | High | ||||||
| Mild fatty liver | 0.931 | < 0.01 | 5.1 | 0.865 | 0.994 | 90.0 | 92.1 |
| Moderate and severe fatty liver | 0.928 | < 0.01 | 12.0 | 0.871 | 0.984 | 94.4 | 75.9 |
采用MRI-IP-OP技术诊断不同程度脂肪肝的ROC曲线显示:MRI-IP-OP诊断轻度脂肪肝(对照组vs轻度脂肪肝组+中重度脂肪肝组)HFF阈值为6.2%,AUC为0.874(P < 0.01),灵敏度为90.0%,特异度为84.1%;MRI-IP-OP诊断中重度脂肪肝(对照组+轻度脂肪肝组vs中重度脂肪肝组)HFF阈值为12.2%,AUC为0.913(P < 0.01),灵敏度为94.4%,特异度为75.9%。见图 2(插页十)和表 3。
| Group | AUC | P | Cut off (η/%) | 95%CI | Sensitivity (η/%) | Specificity (η/%) | |
| Low | High | ||||||
| Mild fatty liver | 0.874 | <0.01 | 6.1 | 0.806 | 0.960 | 90.0 | 85.7 |
| Moderate and severe fatty liver | 0.913 | <0.01 | 12.2 | 0.803 | 0.976 | 94.4 | 75.9 |
脂肪肝已成为严重危害人类健康的常见疾病,发病率逐年上升,早期诊断并进行临床干预可逆转脂肪肝,因此肝脏脂肪定量评估已成为近年研究的热点[3, 10-12]。肝脏脂肪定量评估方法种类繁多,其中金标准是肝脏穿刺活检,但由于其为有创性检查,限制了临床常规开展,目前超声、计算机断层扫描(computed tomography,CT)和MRI是临床常用的肝脏脂肪分析方法[13-15]。超声诊断脂肪肝主观性大,对机器要求高,不适合肝脏脂肪定量评估;CT具有电离辐射,不适合儿童孕妇使用或常规随访[9, 14]。MRI肝脏脂肪定量评估序列包括磁共振波谱(magnetic resonance spectrum, MRS)、MRI-IP-OP和MRI-PDFF等。本研究主要探讨MRI-IP-OP和MRI-PDFF技术定量评估脂肪肝的应用价值。
本研究使用MRI-PDFF和MRI-IP-OP 2种技术定量评估肝脏脂肪含量,并分别与肝脏穿刺活检结果进行对照研究,结果显示:随着脂肪肝等级增加,MRI-PDFF和MRI-IP-OP的HFF升高,组间两两比较差异有统计学意义。本研究中ROC曲线显示:MRI-PDFF诊断轻度脂肪肝和中重度脂肪肝的AUC值分别为0.931、0.928;MRI-IP-OP诊断轻度脂肪肝和中重度脂肪肝的AUC值分别为0.874、0.913;与MRI-IP-OP比较,MRI-PDFF对诊断轻度脂肪肝和中重度脂肪肝具有更高的诊断效能。
MRI-IP-OP是一种基于快速梯度回波的化学位移成像技术,水和脂肪质子在磁场中横向磁矢量能随着TE的改变成同方向(同相位)和反方向(反相位),通过测量同相位和反相位图像的信号强度的改变, 可以推测该组织中脂肪含量[7.16]。本研究结果显示:MRI-IP-OP对于检测脂肪肝有一定意义,然而ROC曲线显示MRI-IP-OP对于各级脂肪肝诊断效能均不及MRI-PDFF。由于MRI-IP-OP是基于信号强度肝脏脂肪含量,脂肪肝患者肝内铁沉积可影响图像磁场均匀性,造成T2*效应,导致局部图像信号丢失,此外T1偏倚、噪声和涡流等因素均可能导致MRI图像上信号强度发生改变,最终影响肝脏脂肪定量结果[7, 9, 16]。因此MRI-IP-OP并非肝脏脂肪定量评估的有效方法。
PDFF定义是组织内脂肪(甘油三酯)质子密度与水和甘油三酯总质子密度之比,是最近提出的基于化学位移的水和脂肪分离技术[9, 17-18]。NOUREDDIN等[19]和IDILMAN等[5]研究发现:MRI-PDFF和MRS均可定量评价肝脏脂肪含量。研究[5, 19]表明:MRS技术要求较高,扫描时间长,一次扫描仅获得肝脏局部数据;MRI-PDFF具有扫描时间短、成功率高及后处理简单等优势,可逐步替代步骤繁杂的MRS。本研究最重要的结果之一即验证了MRI-PDFF技术在肝脏脂肪定量评估方面优于MRI-IP-OP技术。MRI-PDFF通过对同反相位图像校正得出水相和脂肪相图像,根据SIfat/(SIfat+ SIwater)公式计算得到水脂分离图像,一次屏气扫描可同时产生同相位、反相位、水相、脂相和脂肪分数图像,根据多回波信号变化曲线进行脂肪定量,可有效地缩短TE和TR,对T2*效应和噪声等影响因素进行校正[9, 20-22],可更准确地评价肝内脂肪含量。
在另一项研究[20]中,MRI-PDFF与肝脏穿刺活检结果进行对比,使用ROC曲线诊断轻度脂肪肝:HFF阈值为6.1%,AUC为0.961,灵敏度为84%,特异度为100%;诊断中重度脂肪肝:HFF阈值为16.4%,AUC为0.947,灵敏度为77%,特异度为91%。本研究结果显示:MRI-PDFF诊断轻度脂肪肝HFF阈值为5.1%,灵敏度为90.0%,特异度为92.1%;诊断中重度脂肪肝HFF阈值为12.0%,灵敏度为94.4%,特异度为75.9%。对于诊断各级脂肪肝,MRI-PDFF均具有较高的灵敏度和特异度。与肝脏穿刺活检比较,MRI-PDFF主要有以下优势[23]:首先能进行全肝脏的脂肪含量测定,解决了穿刺活检具有抽样误差的缺点;其次,MRI-PDFF作为一种无创性肝脏脂肪定量技术,更适用于脂肪肝的动态监控,为脂肪肝治疗策略和疗效评价提供重要信息,是一种精确、可靠的肝脏脂肪含量MRI定量分析方法。
本研究尚存在一定的不足:纳入病例数相对较少,重度脂肪肝病例较少,可能造成一定程度的结果偏倚,因此未对重度脂肪肝进行单独分析,仍需要进一步扩大样本量进行观察。总之, 肝脏脂肪定量对脂肪肝的诊治具有重要的临床意义,MRI-PDFF作为一种无创、稳定、简便和准确的MRI肝脏脂肪定量评估检查技术,可为脂肪肝的早期诊断、治疗策略选择和预后评估提供重要的信息,具有较好的应用前景。
| [1] |
JEON S K, LEE J M, JPP I, et al. Prospective evaluation of hepatic gteatosis using ultrasound attenuation imaging in patients with chronic liver disease with magnetic resonance imaging proton density fat fraction as the reference standard[J]. Ultrasound Med Biol, 2019, 45(6): 1407-1416. |
| [2] |
CUNHA G M, THAI T T, HAMILTON G, et al. Accuracy of common proton density fat fraction thresholds for magnitude- and complex-based chemical shift-encoded MRI for assessing hepatic steatosis in patients with obesity[J]. Abdom Radiol (NY), 2020, 45(3): 661-671. DOI:10.1007/s00261-019-02350-3 |
| [3] |
FRIEDMAN S L, NEUSCHWANDER-TETRI B A, RINELLA M, et al. Mechanisms of NAFLD development and therapeutic strategies[J]. Nat Med, 2018, 24(7): 908-922. DOI:10.1038/s41591-018-0104-9 |
| [4] |
KÜHN J P, MEFFERT P, HESKE C, et al. Prevalence of fatty liver disease and hepatic iron overload in a northeastern German population by using quantitative MR imaging[J]. Radiology, 2017, 284(3): 706-716. |
| [5] |
IDILMAN I S, KESKIN O, CELIK A, et al. A comparison of liver fat content as determined by magnetic resonance imaging-proton density fat fraction and MRS versus liver histology in non-alcoholic fatty liver disease[J]. Acta Radiol, 2015, 57(3): 271-278. |
| [6] |
TADA T, KUMADA T, TOYODA H, et al. Utility of attenuation coefficient measurement using an ultrasound-guided attenuation parameter for evaluation of hepatic steatosis:comparison with MRI-determined proton density fat fraction[J]. Am J Roentgenol, 2019, 212(2): 332-341. DOI:10.2214/AJR.18.20123 |
| [7] |
CORRIAS G, KREBS S, ESKREIS-WINKLER S, et al. MRI liver fat quantification in an oncologic population:the added value of complex chemical shift-encoded MRI[J]. Clin Imaging, 2018, 52: 193-199. DOI:10.1016/j.clinimag.2018.08.002 |
| [8] |
TANG A, TAN J, SUN M, et al. Nonalcoholic fatty liver disease:MR imaging of liver proton density fat fraction to assess hepatic steatosis[J]. Radiology, 2013, 267(2): 422-431. |
| [9] |
IDILMAN I S, ANIKTAR H, IDILMAN R, et al. Hepatic steatosis:quantification by proton density fat fraction with MR imaging versus liver biopsy[J]. Radiology, 2013, 267(3): 767-775. |
| [10] |
YE J, WU Y, LI F, et al. Effect of orlistat on liver fat content in patients with nonalcoholic fatty liver disease with obesity:assessment using magnetic resonance imaging-derived proton density fat fraction[J]. Therapeut Adv Gastroenterol, 2019. DOI:10.1177/1756284819879047 |
| [11] |
LEE S J, KIM S U. Noninvasive monitoring of hepatic steatosis:controlled attenuation parameter and magnetic resonance imaging-proton density fat fraction in patients with nonalcoholic fatty liver disease[J]. Expert Rev Gastroenterol Hepatol, 2019, 13(6): 523-530. |
| [12] |
MCHENRY S, SHARMA Y, TIRATH A, et al. Crohn's disease is associated with an increased prevalence of nonalcoholic fatty liver disease:a cross-sectional study using magnetic resonance proton density fat fraction mapping[J]. Clin Gastroenterol Hepatol, 2019, 17(13): 2816-2818. DOI:10.1016/j.cgh.2019.02.045 |
| [13] |
GU J L, LIU S S, DU S X, et al. Diagnostic value of MRI-PDFF for hepatic steatosis in patients with non-alcoholic fatty liver disease:a meta-analysis[J]. Eur Radiol, 2019, 29(7): 3564-3573. DOI:10.1007/s00330-019-06072-4 |
| [14] |
GUO Z, BLAKE G M, LI K, et al. Liver fat content measurement with quantitative CT validated against MRI proton density fat fraction:a prospective study of 400 healthy volunteers[J]. Radiology, 2020, 294(1): 89-97. |
| [15] |
FERRAIOLI G, MAIOCCHI L, RACITI M V, et al. Detection of liver steatosis with a novel ultrasound-based technique:a pilot study using MRI-derived proton density fat fraction as the gold standard[J]. Clin Transl Gastroenterol, 2019, 10(10): e00081. DOI:10.14309/ctg.0000000000000081 |
| [16] |
LEITÃO H S, PAULINO C, RODRIGUES D, et al. MR fat fraction mapping[J]. Acad Radiol, 2013, 20(8): 957-961. DOI:10.1016/j.acra.2013.05.004 |
| [17] |
IDILMAN I S, TUZUN A, SAVAS B, et al. Quantification of liver, pancreas, kidney, and vertebral body MRI-PDFF in non-alcoholic fatty liver disease[J]. Abdom Imaging, 2015, 40(6): 1512-1519. DOI:10.1007/s00261-015-0385-0 |
| [18] |
DI MARTINO M, PACIFICO L, BEZZI M, et al. Comparison of magnetic resonance spectroscopy, proton density fat fraction and histological analysis in the quantification of liver steatosis in children and adolescents[J]. World J Gastroenterol, 2016, 22(39): 8812-8819. DOI:10.3748/wjg.v22.i39.8812 |
| [19] |
NOUREDDIN M, LAM J, PETERSON M R, et al. Utility of magnetic resonance imaging versus histology for quantifying changes in liver fat in nonalcoholic fatty liver disease trials[J]. Hepatology, 2013, 58(6): 1930-1940. |
| [20] |
TANG A, DESAI A, HAMILTON G, et al. Accuracy of MR imaging-estimated proton density fat fraction for classification of dichotomized histologic steatosis grades in nonalcoholic fatty liver disease[J]. Radiology, 2015, 274(2): 416-425. |
| [21] |
周懂晶, 黄丽霞, 刘玉品, 等. 3.0 T磁共振IDEAL-IQ技术定量评估脂肪肝的价值[J]. 中华生物医学工程杂志, 2017, 23(1): 55-58. DOI:10.3760/cma.j.issn.1674-1927.2017.01.013 |
| [22] |
COLGAN T J, VAN PAY A J, SHARMA S D, et al. Diurnal variation of proton density fat fraction in the liver using quantitative chemical shift encoded MRI[J]. J Magn Reson Imaging, 2020, 51(2): 407-414. |
| [23] |
洪佳, 施漪雯, 吴晓宁, 等. 影像学诊断技术在非酒精性脂肪性肝病中的应用价值[J]. 临床肝胆病杂志, 2018, 34(12): 2698-2701. DOI:10.3969/j.issn.1001-5256.2018.12.041 |
 2020, Vol. 46
2020, Vol. 46


