扩展功能
文章信息
- 刘艺萍, 孙晓琳, 倪世磊, 赵聪, 葛悦, 周延民, 李明贺
- LIU Yiping, SUN Xiaolin, NI Shilei, ZHAO Cong, GE Yue, ZHOU Yanmin, LI Minghe
- 伴关节盘穿孔的颞下颌关节滑膜软骨瘤1例报告及文献复习
- Synovial chondromatosis of temporomandibular joint with disc perforation: A case report and literature review
- 吉林大学学报(医学版), 2020, 46(03): 639-642
- Journal of Jilin University (Medicine Edition), 2020, 46(03): 639-642
- 10.13481/j.1671-587x.20200334
-
文章历史
- 收稿日期: 2019-08-13
2. 吉林大学口腔医院口腔颌面外科, 吉林 长春 130021
2. Department of Oral and Maxillofacial Surgery, Stomatology Hospital, Jilin University, Changchun 130021, China
颞下颌关节滑膜软骨瘤(synovial chondroma of temporomandibular joint,TMJSC)是颞下颌关节(temporomandibular joint,TMJ)的罕见病之一,近年来国内外相关报道较少,其发病机制尚未完全明确,有学者[1]提出TMJSC可能与滑膜软骨化生有关。由于临床症状不典型,常表现为疼痛和关节弹响等不典型症状,易与其他TMJ疾病混淆,因此常借助计算机断层摄影(computerized tomography,CT)和磁共振成像(magnetic resonance imaging,MRI)对TMJSC进行辅助诊断[2-3]。目前,治疗该病最常用的手术方法为关节镜手术和开放手术,术后效果良好,不易复发[4]。TMJSC为一种良性疾病,具有局部侵袭力,但存在自限性特点[5],其多发生并局限于关节上腔,其中关节盘穿孔导致关节上下腔受累病例十分罕见,国外文献[6]已有报道,而国内相关报道较少。本研究对1例TMJSC并发关节盘穿孔患者的诊治过程进行分析,并结合文献复习,为TMJSC的诊断和治疗提供依据。
1 临床资料 1.1 一般资料患者,女性,53岁,右侧TMJ偶有压痛1年余,于2019年1月8日就诊于本院口腔颌面外科并住院进行治疗。患者1年前偶然发现右侧TMJ压痛,未予重视。1周前因脑神经痛于其他医院住院治疗,2018年12月28日行上下颌骨三维CT检查,显示右侧上颌窦壁及右侧TMJ周围有改变,未进行处置。为求进一步治疗遂来本院就诊。
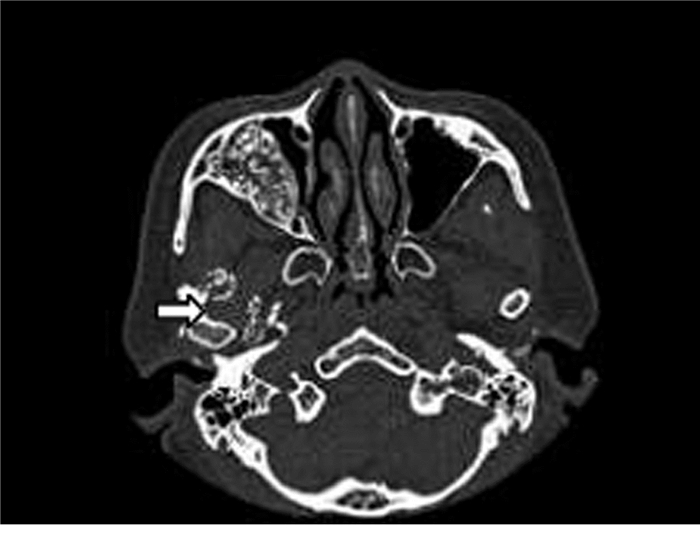
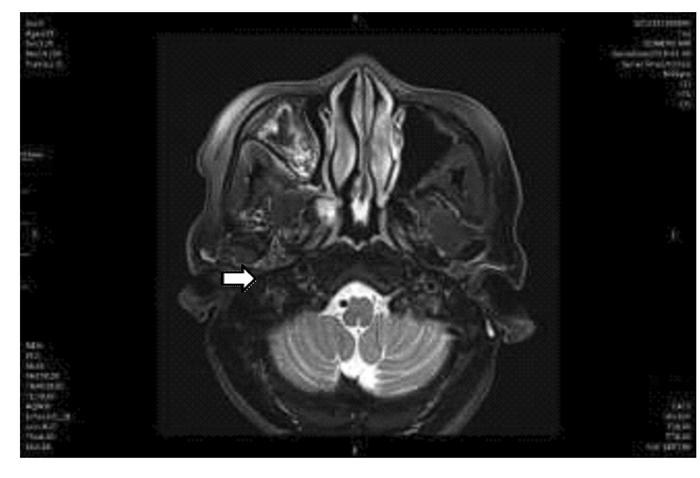
1.2 临床表现、相关检查和诊断专科检查:患者双侧颜面部不对称,下颌略偏左侧,双侧TMJ活动正常,关节有压痛、闭口末期存在弹响,开口度约三横指,开口型正常。口内检查见全口恒牙列,口腔卫生情况良好,咬合关系尚可。15、16和17为烤瓷冠,16存在自发痛及叩痛,其余牙齿无明显异常。口腔黏膜、牙龈和舌黏膜正常,双侧腮腺导管乳头无红肿,分泌正常,舌下肉阜无红肿,分泌正常。咽部无充血,双侧扁桃体无肿大。双侧颏部、下颌下和颈部淋巴结未触及肿大。上下颌骨三维CT检查显示:右侧上颌窦壁、右侧TMJ周围和翼内外肌间隙可见不均匀高密度影;边界不清,右侧上颌窦壁腔变窄,其余双侧上下颌骨形态正常,骨质未见异常,局部未见明显软组织肿胀。鼻骨未见骨折线。见图 1。影像学诊断:右侧上颌窦壁和右侧TMJ周围有改变,不除外骨纤维异常增殖或慢性炎症。2019年1月9日患者于吉林省长春市某影像中心行颞颌关节MRI检查,结果显示:闭口位,双侧髁突不对称,右侧关节腔见弥漫性结节状低、等异常信号,关节腔液体信号影增多,双侧关节间隙增宽,受限开口位。见图 2。临床诊断考虑右侧TMJSC。
|
| 图 1 TMJSC患者上下颌骨三维CT影像 Fig. 1 Three-dimensional CT image of upper and lower jaws of patient with TMJSC |
|
|
|
| 图 2 TMJSC患者关节上腔和关节窝MRI影像 Fig. 2 MRI image of superior articular cavity and articular fossa of patient with TMJSC |
|
|
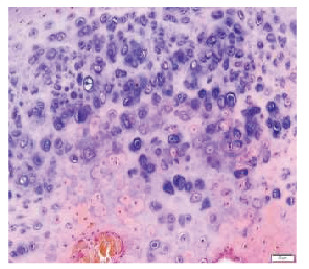
经会诊,决定采取开放性手术方案进行治疗,包括游离体和局部滑膜切除术。全麻下行右侧TMJ成形术、颞下窝肿物切除术和面神经松解减压术。具体手术步骤:患者仰卧于手术台,全麻后,头偏向健侧,采用改良式耳前切口和耳蜗内切口,龙胆紫定点划线,切开皮肤和皮下组织,于SMAS表面翻瓣,切开SMAS至颞深筋膜表面,向下翻瓣至颧弓,有效保护神经和颞浅动静脉。切开颞深筋膜和颞弓骨膜,沿关节囊及咬肌表面向前钝性分离,见关节囊后缘破损。关节盘穿孔,关节上下腔贯通,穿孔面积约为4 mm×5 mm, 并见多个大小不等的类圆形白色骨性肿物位于关节上下腔内,最小肿物体积约为0.1 cm×0.1 cm×0.1 cm,最大肿物体积约为1.0 cm×1.5 cm×1.5 cm,质硬,表面光滑,与关节韧带粘连缠绕,可见关节盘穿孔破损,并用剥离子及挖勺将肿物分离、取出,共100余个肿物(图 3,见封三)。调整咬合,修补关节盘穿孔并复位关节盘,冲洗,关闭关节囊,冲洗,放置引流条,缝合创口。术后肿物行组织病理学检测,结果显示:病变呈多个结节,中央为透明软骨,周围为纤维组织。病理诊断结果符合TMJSC(图 4,见封三)。

|
| 图 3 TMJSC患者游离体示意图 Fig. 3 Diagram of loose bodies of patient with TMJSC |
|
|
|
| 图 4 TMJSC患者游离体组织病理形态表现(HE,×400) Fig. 4 Pathomorphology of loose bodies of patient with TMJSC(HE, ×400) |
|
|
滑膜软骨瘤(synovial chondromatosis,SC)是一种罕见的良性增生性疾病,其生长缓慢并好发于较大关节[7],而在颞下颌关节区较少见[8]。LIU等[9]对119例TMJSC患者的临床资料进行分析显示:患者平均发病年龄为47.2岁,男女比例为1:2.22。TMJSC患者主要临床症状为耳前区肿胀、疼痛、下颌运动受限和关节弹响[10],但该患者只存在疼痛这个不典型症状。除关节区病变外,TMJSC还可能侵犯颅中窝、颈内动脉管和颅神经,由于TMJSC可能侵袭重要解剖结构,因此应及时治疗[11-14]。
SC的病因尚不清楚,但可能与关节间隙创伤性损伤有关。SC被认为是一种病理状态,当间充质组织存在于病变滑膜,滑膜下软骨经历化生后,最终产生并分泌软骨体到关节腔中[1]。多种生长因子和表面抗原与SC发病及进展有关联,如成纤维细胞生长因子2(fibroblast growth factor-2, FGF-2)、转化生长因子β3 (transforming growth factor-β3, TGF-β3)和CD90[15-17],但其详细病因及其机制还需要进一步研究。1977年MILGRAM[18]将膝关节病理过程分为3个阶段,在此基础上,国内学者的研究[19]显示:TMJSC病理过程的关键在于游离体对营养的需求:Milgram Ⅰ期,软骨瘤体为获取营养,通过分泌细胞因子促滑膜血管生成及改变自身位置获得关节滑液的营养;Milgram Ⅱ期,游离体体积增大;Milgram Ⅲ期,游离体的营养供应不足,通过骨化改变形态结构,而利于滑液的渗透。
由于TMJSC的临床症状是非特异性的,因此影像学为其主要诊断方式[20]。影像学诊断包括X线、CT和MRI检查。其中,CT和MRI检查是诊断TMJSC最常用的影像学手段。X线检查能发现关节腔扩大、关节运动受限、关节面不规则、钙化的游离体和关节窝以及髁突的硬化[21]。CT检查在此基础上还能显示软组织的肿胀和游离体的大小、形状及位置;颅底的颞骨关节面变化及颅内病变[2]。该患者CT影像显示出上颌窦壁及关节周围改变,具有诊断意义。通常,MRI主要表现包括多发性软骨结节、关节腔积液和腔内等信号的无定形组织等[3]。该患者的MRI检查结果显示:患侧关节腔有弥漫性结节状低、等异常信号,关节腔液体信号影增多,双侧关节间隙增宽,该影像表现在临床诊断中发挥重要作用。研究[22]显示:通过MRI表现还能进一步将病变分为游离体型、均质型和兼有前两型的混合型。分型可用于评估SC对骨质的侵袭程度,便于确定术式。一项包含2 109例TMJSC患者的研究[23]显示:MRI诊断TMJSC的准确性与开放性手术和关节镜检查一致,因此本文作者推荐将MRI作为TMJSC的非侵入性检查。另有研究[24]显示:TMJSC患者的病变呈多个结节,主要由透明软骨构成,周围为纤维组织,其中细胞核的多形性和双核特征及病变区域的黏液样改变均为SC的特征。
组织病理学检查能对SC进行明确诊断,TMJSC的软骨细胞不具有明显的异型性和有丝分裂特征,这是其与恶性肿瘤的区别;另外,病变缺少晶体、炎症和其他类型细胞,可与晶体沉积性疾病、炎症和非软骨样病变相鉴别。SINK等[24]认为:应与TMJSC鉴别的其他颞下颌关节软骨病变包含退行性关节病、剥脱性骨软骨炎、骨软骨瘤、低级别软骨肉瘤和焦磷酸钙沉积病。TMJSC的保守治疗不易成功,因此大部分患者需行手术治疗。手术治疗后,TMJSC复发率较低,有研究[4]显示:317例TMJSC患者中仅有2例患者复发。
目前,TMJSC最常见的治疗方式为关节镜手术和开放性手术。本研究中TMJSC患者出现罕见的关节盘穿孔,游离体出现于关节上下腔,病灶范围广,因此采取了开放性手术,包括游离体和局部滑膜切除术。开放性手术优点:手术可操作范围大,视野清晰,有利于关节成形术和关节盘切除术等的开展;缺点则为切口较大,不能探及内侧沟等深部区域。关节镜手术优点:切口较小,且能检查到内侧沟等深部区域及关节上腔的各个部位;但当游离体较大或病灶范围大时,关节镜则不适用。BAI等[25]研究显示:当关节上腔的游离体扩张到颞下间隙的凸起或髁嵴内侧与髁颈之间时,推荐采用关节镜辅助开放性手术,该术式有利于彻底消除病变,并可能避免采用截骨术,减少创伤程度,缩短手术时间。
| [1] |
REED L S, FOSTER M D, HUDSON J W. Synovial chondromatosis of the temporomandibular joint:A case report and literature review[J]. Cranio, 2013, 31(4): 309-313. |
| [2] |
YU Q, YANG J, WANG PZ, et al. CT features of synovial chondromatosis in the temporomandibular joint[J]. Oral Surg Oral Med Oral Pathol Oral Radiol Endod, 2004, 97(4): 524-528. |
| [3] |
WANG P, TIAN Z, YANG J, et al. Synovial chondromatosis of the temporomandibular joint:MRI findings with pathological comparison[J]. Dentomaxillofac Radiol, 2012, 41(2): 110-116. |
| [4] |
HAN Z X, CHEN M J, YANG C, et al. Recurrent synovial chondromatosis of the temporomandibular joint:report of two cases[J]. Br J Oral Maxillofac Surg, 2017, 55(9): 965-967. |
| [5] |
BENSLAMA L, SCHOUMAN T, TOURE S, et al. Synovial chondromatosis of the temporomandibular joint:Report and analysis of 12 cases[J]. J Stomatol Oral Maxillofac Surg, 2019, 120(5): 476-479. |
| [6] |
SEMBRONIO S, ALBIERO A M, TORO C, et al. Arthroscopy with open surgery for treatment of synovial chondromatosis of the temporomandibular joint[J]. Br J Oral Maxillofac Surg, 2008, 46(7): 582-584. |
| [7] |
BALASUNDARAM A, GEIST J R, GORDON S C, et al. Radiographic diagnosis of synovial chondromatosis of the temporomandibular joint:A case report[J]. J Can Dent Assoc, 2009, 75(10): 711-714. |
| [8] |
LIEGER O, ZIX J, STAUFFER-BRAUCH E J, et al. Synovial chondromatosis of the temporomandibular joint with cranial extension:a case report and literature review[J]. J Oral Maxillofac Surg, 2007, 65(10): 2073-2080. |
| [9] |
LIU X G, HUANG Z Y, ZHU W Y, et al. Clinical and imaging findings of temporomandibular joint synovial chondromatosis:an analysis of 10 cases and literature review[J]. J Oral Maxillofac Surg, 2016, 74(11): 2159-2168. |
| [10] |
GUARDA-NARDINI L, PICCOTTI F, FERRONATO G, et al. Synovial chondromatosis of the temporomandibular joint:a case description with systematic literature review[J]. Int J Oral Maxillofac Surg, 2010, 39(8): 745-755. |
| [11] |
MCCAFFERY C, DODD M, BEKIROGLU F, et al. Synovial chondromatosis of the temporomandibular joint with extension into the middle cranial fossa and internal carotid canal[J]. Int J Oral Maxillofac Surg, 2017, 46(7): 867-870. |
| [12] |
YOSHITAKE H, KAYAMORI K, WAKE S, et al. Synovial chondromatosis of the right side temporomandibular joint extending to the middle cranial fossa:a case report with 7-year postoperative follow up and expression of a biomarker of cell proliferative activity[J]. Int J Surg Case Rep, 2016, 20: 133-137. |
| [13] |
ROMANO A, FARO C L, SALZANO G, et al. Synovial chondromatosis of temporomandibular joint spreading into the cranial space[J]. J Oral Maxillofac Surg Med Pathol, 2018, 30(3): 267-271. |
| [14] |
JEYARAJ P E, SHARMA V. Synovial osteochondromatosis of the temporomandibular joint manifesting as a large infratemporal space occupying lesion[J]. J Oral Maxillofac Surg, 2017, 16(3): 387-391. |
| [15] |
WILMS C T, HEIM N, TESCHKE M, et al. Synovial chondromatosis of the temporomandibular joint:Immunohistochemical examinations regarding the role of insulin-like growth factors and their binding proteins in the etiology of this disease[J]. J Craniomaxillofac Surg, 2017, 45(2): 198-202. |
| [16] |
LI Y, EL MOZEN L A, CAI H, et al. Transforming growth factor beta 3 involved in the pathogenesis of synovial chondromatosis of temporomandibular joint[J]. Sci Rep, 2015, 5: 8843. |
| [17] |
WAKE S, YOSHITAKE H, KAYAMORI K, et al. Expression of CD90 decreases withprogression of synovial chondromatosis in the temporomandibular joint[J]. Cranio, 2016, 34(4): 250-256. |
| [18] |
MILGRAMJ W. The classification of loose bodies in human joints[J]. Clin Orthop Relat Res, 1977(124): 282-291. |
| [19] |
李颖杰, 冯亚平, 邓末宏, 等. 颞下颌关节滑膜软骨瘤病的病理特征[J]. 口腔医学研究, 2017, 33(11): 1135-1138. |
| [20] |
LEITE P C C, TOLENTINO E S, YAMASHITA A L, et al. Surgical treatment of synovial chondromatosis in the inferior compartment of the temporomandibular joint with articular disc involvement[J]. J Craniofac Surg, 2018, 29(2): e199-e203. |
| [21] |
NOYEK A M, HOLGATE R C, FIREMAN S M, et al. The radiologic findings in synovial chondromatosis (chondrometaplasia) of the temporomandibular joint[J]. J Otolaryngol, 1977, 6(3 suppl): 45-48. |
| [22] |
韩孜祥, 陈敏洁, 杨驰, 等. 171例颞下颌关节滑膜软骨瘤病MRI分析[J]. 中国口腔颌面外科杂志, 2017, 15(1): 41-45. |
| [23] |
LIU X, WAN S, SHEN P, et al. Diagnostic accuracy of synovial chondromatosis of the temporomandibular joint on magnetic resonance imaging[J]. PLoS One, 2019, 14(1): e0209739. |
| [24] |
SINK J, BELL B, MESA H. Synovial chondromatosis of the temporomandibular joint:clinical, cytologic, histologic, radiologic, therapeutic aspects, and differential diagnosis of an uncommon lesion[J]. Oral Surg Oral Med Oral Pathol Oral Radiol, 2014, 117(3): e269-e274. |
| [25] |
BAI G, YANG C, QIU Y, et al. Open surgery assisted with arthroscopy to treat synovial chondromatosis of the temporomandibular joint[J]. Int J Oral Maxillofac Surg, 2017, 46(2): 208-213. |
 2020, Vol. 46
2020, Vol. 46


