扩展功能
文章信息
- 王瑜, 蒋鑫萍, 常健, 曲超, 韩冬冰
- WANG Yu, JIANG Xinping, CHANG Jian, QU Chao, HAN Dongbing
- 以皮肤黏膜淋巴结改变为首发症状的ALK阳性间变性大细胞淋巴瘤1例报告及文献复习
- ALK-positive anaplastic large cell lymphoma with changes in skin mucosal lymph nodes as first symptom: A case report and literature review
- 吉林大学学报(医学版), 2019, 45(06): 1432-1435
- Journal of Jilin University (Medicine Edition), 2019, 45(06): 1432-1435
- 10.13481/j.1671-587x.20190640
-
文章历史
- 收稿日期: 2018-12-05
2. 吉林大学第一医院联合超声科, 吉林 长春 130021;
3. 吉林大学第一医院放疗科, 吉林 长春 130021;
4. 吉林省一汽总医院信息技术科, 吉林 长春 130011
2. Department of Ultrasound, First Hospital, Jilin University, Changchun 130021, China;
3. Department of Radiotherapy, First Hospital, Jilin University, Changchun 130021, China;
4. Department of Information Technology, Jilin FAW General Hospital, Changchun 130011, China
间变性大细胞淋巴瘤(anaplastic large cell lymphoma, ALCL)是非霍奇金淋巴瘤的一个特殊亚型,于1985年由德国病理学家STEIN等应用Ki-1(CD30)抗体识别。ALCL肿瘤细胞呈间变性,生长具有内聚性,且向淋巴结窦侵犯,多数ALCL患儿表达间变性淋巴瘤激酶(anaplastic lymphoma kinase,ALK)融合蛋白。根据肿瘤是否表达ALK分为ALK阳性ALCL和ALK阴性ALCL。在临床上ALCL被分为原发性(系统性和皮肤)和继发性(由其他淋巴瘤转化而来)2种。ALCL发病率较低,约占儿童非霍奇金淋巴瘤的10%,其中以男孩多见,发病中位年龄约为10岁。本文作者回顾性分析1例以皮肤黏膜淋巴结改变为首发症状的ALK阳性ALCL患儿的临床资料,并结合相关文献报道如下。由于ALCL发病率低,临床表现多不典型,临床医生对其认识有限,误诊率高,本研究旨在提高临床医生对ALCL的认识。
1 临床资料 1.1 一般资料患儿,女性,10岁,因“颈部淋巴结进行性增大伴疼痛半个月”于2018年6月6日入吉林大学第一医院小儿肿瘤科进行治疗。
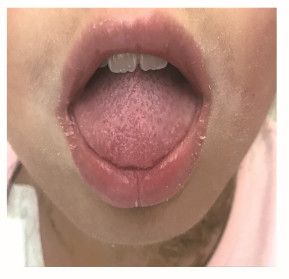
1.2 临床表现和体格检查患儿自入院前半个月,无意间发现左颈部淋巴结肿大,约鹌鹑蛋大小,伴触痛,就诊于当地医院,给予“美罗培南”等抗生素抗感染治疗,原颈部淋巴结较之前呈进行性增大,并发现右侧肿大淋巴结。病程中患儿体质量减轻3 kg,无发热和盗汗。入院后查体:体温36.9℃,脉搏106 min-1,呼吸26 min-1,血压102/68 mmHg,身高146 cm,体质量33.7 kg。口唇殷红,表皮皲裂,周身皮肤干燥,以双手为著,掌心可见皲裂,指端可见膜状脱屑,双颈部可见多个肿大淋巴结,表面皮肤颜色同周围皮肤,较大淋巴结位于左上颈部,直径约3 cm,部分肿大淋巴结呈融合改变,边界不清,活动度差,伴压痛,皮温略高,舌乳头呈草莓舌状(图 1和2,见插页七),咽部无明显充血,双肺呼吸音粗,未闻及明显干湿啰音,心率106 min-1,心音有力,节律规整,未闻及明显病理性杂音,腹平软,无压痛、反跳痛及肌紧张,肝脾肋下未触及明显肿大,四肢及神经系统查体未见明显阳性体征。
|
| 图 1 以皮肤黏膜淋巴结改变为首发症状的ALK阳性ALCL患儿口唇和舌乳头表现 Fig. 1 Morphology of lip and tongue nipple of ALK-positive ALCL patient with changes in skin mucosal lymph nodes as first symptom |
|
|

|
| 图 2 以皮肤黏膜淋巴结改变为首发症状的ALK阳性ALCL患儿掌心和指端表现 Fig. 2 Morphology of palm and fingertips of ALK-positive ALCIpatient with changes in skin mucosal lymph nodes as first symptom |
|
|
血常规:白细胞17.67×109 L-1,中性粒细胞百分比0.72,淋巴细胞百分比0.16,中性粒细胞绝对值12.78×109 L-1,血红蛋白133 g·L-1,血小板496×109 L-1;凝血常规、心肌酶、肝功、肾功、离子、血糖、血脂和铁代谢未见明显异常。心电图、心脏彩超和腹部超声未见明显异常。颈部淋巴结彩超:双侧颈部、锁骨上窝和胸骨上窝均可探及多枚大小不等的淋巴结声像,形态饱满,回声减低,皮髓结构消失,左侧较大的结节为31 mm×20 mm,右侧较大的结节为21.4 mm×14.9 mm,CDFI:可见血流信号。周围软组织回声增强。肺部CT:①纵隔和双侧肺门处占位;②双侧胸腔积液;③左肺上叶舌段纤维索条影;④右侧叶间胸膜局限性增厚。PET-CT: ①全身多发淋巴结肿大伴代谢增高(左侧咽旁间隙、左侧颌下、双侧颈部、双侧胸大小肌后方、双侧腋窝、纵隔、双肺门、胰腺周围、腹主动脉旁、双侧肾血管旁、双侧髂血管旁、双侧髂窝、双侧腹股沟),考虑淋巴瘤;②双肺上叶和右肺中叶小结节,代谢不高,考虑炎性;双肺下叶被动性肺不张;双肺炎症及炎性条索,部分呈间质性炎变;心包腔及双侧胸腔积液。骨髓涂片和染色体未见异常。免疫分型:异常细胞占有核细胞的5.53%,为异常表型T淋巴细胞。外周血免疫分型:异常细胞占有核细胞的10.24%,为异常表型T淋巴细胞。颈部淋巴结活检病理结果:非霍奇金恶性淋巴瘤,WHO分类:ALK阳性间变性大细胞淋巴瘤(ALCL)。免疫组织化学检测结果:Ki-67(+90%),TdT(—),PAX-5(—), CD7(+), CD20(—), CD3(+), CD34(—), CD10(—), CD43(+), CD1a(—),CD99(+), CK-pan(—),CD30(+), CD15(—), EMA(—), ALK(核浆+),Granzyme B(+),CD21(DC+), CD2(+), CD8(—), CD5(部分+),CD7(+)。原位杂交:EBER(—)。分子病理检测结果显示:T细胞基因重排(+)。
1.4 诊断和鉴别诊断按照《国际儿童非霍奇金淋巴瘤分期系统(2012年)》,该患儿明确诊断为ALK阳性ALCL(Ⅳ期,R3组)。
1.5 治疗和预后选用APO方案,在诱导化疗后,复查全身PET-CT提示原全身多发高代谢结节大部分消失,仅双颈部有代谢稍高淋巴结,考虑肿瘤活性部分残留;骨髓免疫分型提示异常细胞占有核细胞的0.27%,外周血免疫分型提示异常细胞占有核细胞的0.13%,病情达部分缓解(partial remission, PR),之后更换治疗方案为B-NHL-BFM-90方案,经过1个周期改良AA方案后,复查全身PET-CT,且骨髓和外周血免疫分型均转阴。
2 讨论ALCL最早于1985年被提出,于1994年正式被命名[1-2]。在组织病理学上,根据瘤细胞主要形态学特征分为3个亚型:①普通型[3]:可见成片的大淋巴细胞,胞核呈马蹄形,染色质较少,可见多个核仁;②淋巴组织细胞型[4]:瘤细胞体积小到中等,散在或呈小灶分布。同时伴有大量的组织细胞;③小细胞型[5]:瘤细胞体积较小,核形不规则,部分呈脑回状,染色质致密。瘤细胞间可见散在或呈簇状分布的无明显异型性的大细胞。在遗传学方面,ALK基因位于人类染色体2p23,编码相对分子质量为200 000的成熟ALK蛋白。正常情况下ALK仅在神经系统表达,并随着脑发育成熟含量逐渐降低,文献[6-7]报道:ALCL中ALK基因重排的阳性率为65%~85%,最常见的异常核型为t(2;5)(p23;q35),产生有致癌性的异常ALK融合蛋白。不同于成人,90%以上的儿童ALCL有ALK基因的异常。根据2008年WHO[8]分类:ALCL分为ALK阳性ALCL、ALK阴性ALCL和原发于皮肤的ALCL,ALK阳性的原发性系统性ALCL主要发生在20~30岁年龄段,男性多于女性,其常侵犯淋巴结及结外器官,结外器官以皮肤和骨多见,并伴有发热等症状,但肠道和中枢神经系统受累少见[9],采用HE染色分析时骨髓侵犯率约为11%,免疫组织化学检测侵犯率则约为30%。ALK阴性的原发性系统性ALCL更多见于年龄大的患者,而原发性皮肤性ALCL多发生在老年患者(平均年龄约为60岁),ALK阴性且缺乏细胞毒性表型。治疗方面,ALK阳性的原发性系统性ALCL化疗疗效好,生存率较高;ALK阴性的原发性系统性ALCL治疗疗效较差,预后不良;而原发于皮肤的ALCL预后较好。儿童中,ALK阳性和ALK阴性ALCL患儿形态表现方面无明显差异,但预后明显不同。文献[10]报道:儿童骨髓和(或)外周血ALK阳性的ALCL其无事件生存率低于ALK阴性的ALCL,另外ALK阳性与多器官受累有关,而且化疗后NPM-ALK融合基因未转阴者复发风险更高。
目前国际上ALCL治疗方案多采用ALCL99方案,该方案需采用长春花碱治疗,并将其作为维持治疗方案,其总生存率可达90%以上[11]。但由于我国大陆地区尚无长春花碱,故本课题组首先采用了美国儿童肿瘤研究组的APO方案,在诱导化疗结束后,对患儿全面评估病情,未达完全缓解(complete remission, CR),遂予以更换为BFM协作组的B-NHL-BFM-90方案。文献[12]报道:采用该方案R1、R2和R3组患者5年无事件生存率分别为(81.4±6.4)%,(83.3±10)%和(75.3±9.8)%,而该患儿在1个周期化疗后,病情达CR,反应良好。近年来,随着靶向药物的深入研究,针对CD30抗原及ALK基因的药物有望成为新的治疗手段。克唑替尼是ATP竞争性的蛋白激酶抑制剂,可抑制ALK、ROS1和MET[13-14],是针对ALK基因的靶向治疗药物,克唑替尼目前已被批准用于ALK阳性的NSCLC,但克唑替尼治疗ALK阳性ALCL的报道较少。CLEARY等[15]报道了1例难治ALK阳性ALCL患者,经克唑替尼治疗后达CR,后行Allo-HSCT及克唑替尼维持保持CR。文献[16]报道:在儿童中克唑替尼应用安全性高,且治疗反应率可达88%(8/9)。但由于我国患儿家庭经济承受能力低,故在我国尚未全面推广。
文献[17]报道:ALCL误诊率高达90%以上。其可能原因:①ALCL早期可发生结外器官侵犯,首发症状多种多样,涉及专业广泛;②肿瘤细胞释放多种细胞因子,使患儿出现白细胞升高、发热等类似炎症的表现,易与感染性疾病混淆;③盲目使用激素等。本例患儿以皮肤黏膜和淋巴结改变为首要表现,其病初鉴别诊断:①川崎病。该病典型表现包括口唇殷红,指端膜状脱屑,颈部肿大淋巴结及草莓舌,但该患儿已为10岁大女孩,且病程中无发热,入院后完善心脏彩超未见典型冠脉扩张表现,均不支持川崎病诊断;②结缔组织疾病。本类疾病多见于大女孩,以发热、皮肤黏膜改变及肌肉关节改变为主要临床表现,但皮肤黏膜改变以光敏感、溃疡为多见,与本例患儿皮肤黏膜改变不同,且本例患儿无发热及肌肉关节改变,故本病可能性不大。③其他恶性肿瘤。杨景柯等[18]报道了1例ALK阳性ALCL误诊为横纹肌肉瘤的病例,提示可依据患者临床和病理特点,将该病与其他肿瘤进行鉴别。本例患儿最终通过淋巴结活检确诊为ALK阳性ALCL。本例患儿病初骨髓涂片及脑脊液常规生化均未见异常,但流式细胞学检查均提示可见异常表型T淋巴细胞,明确存在骨髓及神经系统受累,故分期为Ⅳ期、R3组。
综上所述,儿童ALCL发病率低,临床表现多不典型,易造成临床误诊,故临床儿科医生应提高对该病的认识,以期达到早期诊断和早期治疗的目的。
| [1] |
STEIN H, MASON D Y, GERDES J, et al. The expression of the Hodgkin's disease associated antigen Ki-1 in reactive and neoplastic lymphoid tissue:evidence that Reed-Sternberg cells and histiocytic malignancies are derived from activated lymphoid cells[J]. Blood, 1985, 66(4): 848-858. DOI:10.1182/blood.V66.4.848.bloodjournal664848 |
| [2] |
HARRIS N L, JAFFE E S, STEIN H, et al. A revised European-American classification of lymphoid neoplasms:A proposal from the International Lymphoma Study Group[J]. Blood, 1994, 84(5): 1361-1392. DOI:10.1182/blood.V84.5.1361.1361 |
| [3] |
KADIN M E. Anaplastic large cell lymphoma and its morphological variants[J]. Cancer Surv, 1997, 30: 77-86. |
| [4] |
PILERI S, FALINI B, DELSOL G, et al. Lymphohistiocytic T-cell lymphoma(anaplastic large cell lymphoma CD30+/Ki-1+ with a high content of reactive histiocytes)[J]. Histopathology, 1990, 16(4): 383-391. DOI:10.1111/j.1365-2559.1990.tb01143.x |
| [5] |
KINNEY M C, COLLINS R D, GREER J P, et al. A small-cell-predominant variant of primary Ki-1(CD30+)T-cell lymphoma[J]. Am J Surg Pathol, 1993, 17(9): 859-868. DOI:10.1097/00000478-199309000-00001 |
| [6] |
魏婵娟, 赵强. ALK与儿童恶性肿瘤关系的研究进展[J]. 中国肿瘤临床, 2015, 42(4): 251-253. DOI:10.3969/j.issn.1000-8179.20141164 |
| [7] |
EYRE T A, KHAN D, HALL G W, et al. Anaplastic lymphoma kinase-positive anaplastic large cell lymphoma:current and future perspectives in adult and paediatric disease[J]. Eur J Haematol, 2014, 93(6): 455-468. DOI:10.1111/ejh.12360 |
| [8] |
SWERDLOW S H, CAMPO E, HARRIS N L, et al. WHO classification of tumours of haematopoietic and lymphoid tissues[M]. Lyon: LARC Press, 2008: 312-316.
|
| [9] |
ALLEN C E, KELLY K M, BOLLARD C M. Pediatric lymphomas and histiocytic disorders of childhood[J]. Pediatr Clin North Am, 2015, 62(1): 139-165. |
| [10] |
杨菁, 赵晓曦, 金铃, 等. 间变性大小淋巴瘤患儿骨髓及外周血NPM-ALK融合基因表达与预后的关系[J]. 中华血液学杂志, 2013, 34(8): 700-703. |
| [11] |
LE DELEY M C, ROSOLEN A, WILLIAMS D M, et al. Vinblastine in children and adolescents with high-risk anaplastic large-cell lymphoma:results of the randomized ALCL99-vinblastine trial[J]. J Clin Oncol, 2010, 28(25): 3987-3933. DOI:10.1200/JCO.2010.28.5999 |
| [12] |
SUN X F, ZHEN Z J, LIN S X, et al. Treatment outcome of Chinese children with anaplastic large cell lymphoma by using a modified B-NHL-BFM-90 protocol[J]. Pediatr Hematol Oncol, 2014, 31(6): 518-527. DOI:10.3109/08880018.2014.939793 |
| [13] |
MAHUAD C V, REPARAZ M D E L, ZERGA M E, et al. Three years sustained complete remission achieved in a primary refractory ALK-positive anaplastic T large cell lymphoma treated with crizotinib[J]. Rare Tumors, 2016, 8(2): 6266. |
| [14] |
SULLIVAN I, PLANCHARD D. ALK inhibitors in non-small cell lung cancer: the latest evidence and developments[J]. Ther Adv Med Oncol, 2016, 8(1): 32-47. DOI:10.1177/1758834015617355 |
| [15] |
CLEARY J M, RODIG S, BARR P M, et al. Crizotinib as salvage and maintenance with allogeneic stem cell transplantation for refractory anaplastic large cell lymphoma[J]. J Natl Compr Canc Netw, 2014, 12(3): 323-326. DOI:10.6004/jnccn.2014.0034 |
| [16] |
MOSSÉ Y P, LIM M S, VOSS S D, et al. Safety and activity of crizotinib for paediatric patients with refractory solid tumours or anaplastic large-cell lymphoma: a children's Oncology Group phase 1 consortium study[J]. Lancet Oncol, 2013, 14(6): 472-480. DOI:10.1016/S1470-2045(13)70095-0 |
| [17] |
杨菁, 张永红, 段彦龙. 儿童间变性大细胞淋巴瘤31例误诊分析[J]. 实用儿科临床杂志, 2008, 23(15): 1176-1178. DOI:10.3969/j.issn.1003-515X.2008.15.013 |
| [18] |
杨景柯, 朱兴虎, 左文丽, 等. 间变性大细胞淋巴瘤(ALK阳性)误诊为横纹肌肉瘤1例并文献复习[J]. 中国医药导报, 2013, 10(3): 109-111. DOI:10.3969/j.issn.1673-7210.2013.03.043 |
 2019, Vol. 45
2019, Vol. 45


