扩展功能
文章信息
- 常盼盼, 韩帅, 别黎, 李毅平
- CHANG Panpan, HAN Shuai, BIE Li, LI Yiping
- 轴外型桥小脑角区髓母细胞瘤2例报告及文献复习
- Extra-axial medulloblastoma in cerebellopontine angle: A report of two cases and literature review
- 吉林大学学报(医学版), 2019, 45(03): 701-704
- Journal of Jilin University (Medicine Edition), 2019, 45(03): 701-704
- 10.13481/j.1671-587x.20190340
-
文章历史
- 收稿日期: 2018-08-01
髓母细胞瘤(medulloblastoma,MB)是一种恶性的、侵袭性的小脑胚胎类肿瘤,儿童好发,占儿童脑肿瘤的16%,占儿童小脑肿瘤的40%,约80%的小儿MB发生在小脑和第四脑室[1-3]。成人轴外型桥小脑角(cerebellopontine angle,CPA)区MB非常罕见,迄今为止文献报道了约33例,近两年国内外只有3例相关报道,而且大部分患者为儿童或者婴幼儿[4-6]。尽管在组织病理学上MB诊断简单,但轴外型CPA区MB术前正确诊断困难,容易误诊为更常见的轴外CPA区肿块(如神经鞘瘤或脑膜瘤)。目前该病的研究热点是寻找治疗侵袭性疾病的新方法和准确识别疾病风险,以便于针对性地使用辅助治疗方法。本文作者分析本科收治的2例轴外型CPA区MB患者的临床资料,并结合相关文献进行探讨,以期为轴外型CPA区MB的治疗提供依据。
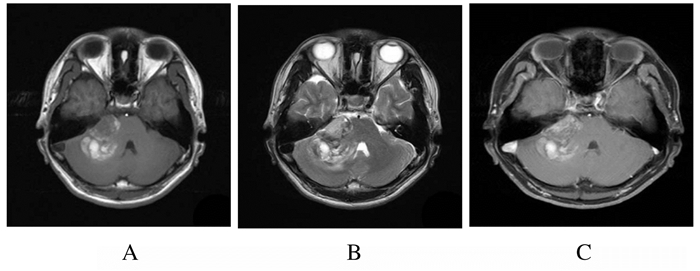
1 临床资料 1.1 一般资料病例1:患者,男性,34岁,因耳鸣、听力下降1年,头疼、头晕伴呕吐1个月,加重1 h于2011年7月入院。查体:右侧听力下降、右侧眼睑闭合不全,右侧嘴角歪斜。头颅核磁共振(MRI)平扫及增强显示:右侧CPA区见不规则团块状异常信号,部分边缘模糊,与邻近脑干及右侧小脑半球分界不清,最大层面大小约为5.4 cm×4.5 cm;T1WI呈高、等及稍低信号;T2WI及FALIR均呈高及低混杂信号;DWI呈稍低及高信号,右侧内听道增粗,四脑室受压变窄;增强扫描近CPA区病灶可见不均匀明显强化。见图 1。病例1术前诊断为前庭神经鞘瘤。
|
| A:T1WI; B:T2WI; C:Enhanced scanning. 图 1 右侧轴外型CPA区MB患者的MRI图像 Fig. 1 MRI images of one patient with extra-axial CPA area MBin rigth side |
|
|
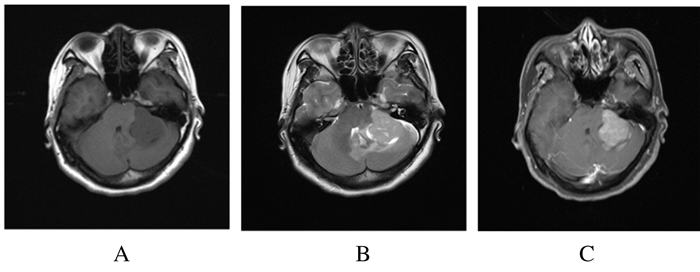
病例2:患者,女性,38岁,因头痛3个月,听力下降及行走不稳2个月于2017年2月入院。既往身体健康,否认高血压、糖尿病及家族疾病史。查体:神经系统查体未见明显阳性体征。头颅MRI平扫及增强显示:CPA区见不规则团块状异常信号,邻近座侧小脑半球受压,最大层面大小约为5.5 cm×4.9 cm;T1WI呈稍低信号;T2WI及FALIR均呈稍高;DWI呈高信号,明显较均匀强化。见图 2。病例2术前诊断为脑膜瘤。
|
| A:T1WI; B:T2WI; C:Enhanced scanning. 图 2 左侧轴外型CPA区MB患者的MRI图像 Fig. 2 MRI images of one patient with extra-axial CPA area MB in left side |
|
|
2例患者均通过乙状窦后入路手术进行CPA区肿瘤切除术,病例1术中可见肿瘤位于右侧CPA区,呈淡红色,质地较韧,血运丰富,肿瘤周边见血性液体。肿瘤与小脑半球粘连紧密,与脑干侧方也有明显粘连;逐步游离肿瘤包膜,最后将内听道内肿瘤切除,探查内听道后壁无肿瘤组织残留。病例2术中可见肿瘤位于左侧CPA区,呈淡褐色,质地略韧,实性,血供丰富,其基底部在岩骨硬膜及小脑幕上。2例患者均将肿瘤全切。术后患者恢复良好,出院时建议继续行放疗和化疗。
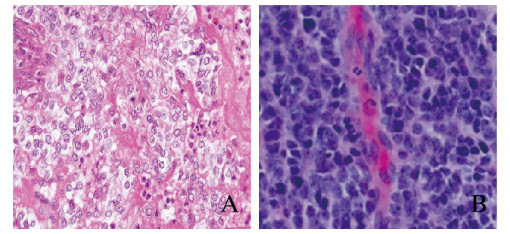
1.3 病理诊断病例1术后病理诊断:CPA MB(促纤维增生型),WHO Ⅳ级(图 3A,见封三)。免疫组织化学:KiKi-67(10%),P53(-),Vimentin(+),Nestin(+),GFAP(-),Oligo-2,Syn(+),NeuN(-), EMA(点灶状+),Map2(+),IDH1R132H突变(-),MBP,CD68(-),MGMT(+90%),CgA(+),CD56(+),TTF-1,Desmin(-),LCA(-),SALL4(-)。病例2术后病理诊断:CPA MB(促纤维增生型),WHO Ⅳ级(图 3B,见封三);免疫组织化学:Ki-67(+40%),Syn(+), NF(-),GFAP(散在+),CD99(部分+),NeuN(散在+),Vimentin(+),Nestin(+),NSE(+),EMA(-),PR(-),CD34(-)。
|
| A: Case 1; B: Case 2. 图 3 2例轴外型CPA区MB患者病变组织病理形态表现(HE,×20) Fig. 3 Pathomorphology of lesion tissues of 2 patients with extra-axial MB in CPA area (HE, ×20) |
|
|
2例患者均随访15个月未见复发。
2 讨论MB是最常见的儿童后颅窝中线部位的原发性恶性肿瘤,男性好发,发病高峰在5~7岁,70%发生于16岁以下, 约80%的MB发生于小脑蚓下部的中线,通常向四脑室生长并充满第四脑室。发生于小脑半球的MB比较少见,常见于青少年或年轻人。MB的起源可能是生发细胞或其位于下髓层末端的残存细胞,也可能来自外部颗粒层的原始多潜能细胞,但确切的来源目前尚未明确[7-8]。
常见的CPA肿瘤通常包括神经鞘瘤、脑膜瘤、原发性胆脂瘤和表皮样肿瘤,这些肿瘤占CPA肿瘤的98%[9-10]。MB可能是来源于小脑半球外颗粒层的残存原始多潜能细胞,其可以通过2种途径占据CPA,包括从第四脑室到卢氏孔的外侧延伸,或从小脑表面或桥脑表面直接外生生长[11]。关于CPA区MB的报道很少,且大多为轴内型,这使得该肿瘤的轴外部位极为罕见,易与CPA常见肿瘤混淆。本文作者报道的2例成人CPA区MB误诊为前庭神经鞘瘤和脑膜瘤。FURTADO等[12]报道的64例MB中,50例位于中线,14例位于小脑半球,但尚未见发生于CPA的病例。本研究中2例患者均为中青年,MB发生于CPA区且为轴外型。
根据MB的组织病理学特点,通常将MB分为经典型、弥漫结节型、促纤维增生型和大细胞型4种类型,在成人中促纤维增生型MB较经典型更常见[13-14],本研究中2例患者均为促纤维增生型MB。与经典型MB比较,促纤维增生型MB更多位于小脑半球,常见囊肿和坏死,病例1有囊变及出血和坏死,病例2仅见囊变。
CPA区MB患者的临床表现与CPA常见肿瘤相似,以听力下降、前庭功能障碍为首发症状,也可表现为第Ⅴ、Ⅵ、Ⅶ颅神经损害或小脑共济失调,颅高压症状出现相对较晚[15]。然而,CPA区MB患者并无特定的临床症状和体征,CPA区MB患者通常症状持续时间较短,脑干和小脑功能障碍可能高度提示该肿瘤,其常侵犯颅神经。本研究中病例1手术证实肿瘤向右侧内听道生长,侵犯听神经及面神经,故出现右侧听力下降、眼睑闭合不全及嘴角歪斜;病例2肿瘤压迫左侧前庭窝神经,故出现听力下降及走路不稳。MB通过脑脊液转移到椎管、软脑膜和幕上区域。MB的转移率为38%~60%,其中椎管转移最常见,约占58%。MB的MRI信号特点及强化方式常表现为T1WI呈稍低或等信号,T2WI及FALIR序列呈等或稍高信号,T1WI增强扫描肿瘤实性强化程度不一,常并发囊变和坏死,出血少见;有文献[16]报道出血并非MB的典型表现。表观弥散系数(DWI)和弥散加权成像(ADC)上的受限扩散提示MB的可能性。
由于CPA区MB病例报道较少,治疗效果并不理想。因此,在CPA肿瘤的鉴别诊断中应考虑MB,并根据术中情况调整手术策略。在术前诊断MB可能性大的情况下,应尽量行全部切除术,因为残留的肿瘤与进展生存率有关。如为轴外良性肿瘤,可以选择完成次全切除手术,以避免神经缺损。病理诊断对患者术后复查时间和内容有明显影响。如为MB,则应在术后10~14 d对整个脊柱进行MRI检查,同样,还应进行腰椎穿刺,以寻找肿瘤的CSF扩散情况。术后患者通常接受放射治疗和(或)化疗,这取决于患者的年龄、肿瘤切除的范围、软脑膜的播散以及与肿瘤相关的分子因素[17-18]。
| [1] | MATA M M, ZAPOTOCKY M, LAUGHLIN S, et al. MRI characteristics of primary tumors and metastatic lesions in molecular subgroups of pediatric medulloblastoma:A single-center study[J]. AJNR, 2018, 39(5): 949–955. DOI:10.3174/ajnr.A5578 |
| [2] | QUINLAN A, RIZZOLO D. Understanding medulloblastoma[J]. JAAPA, 2017, 30(10): 30–36. DOI:10.1097/01.JAA.0000524717.71084.50 |
| [3] | PHOENIX T N, PATMORE D M, BOOP S, et al. Medulloblastoma genotype dictates blood brain barrier phenotype[J]. Cancer Cell, 2016, 29(4): 508–522. |
| [4] | RAYWAT N, VICH Y, CHATCHAI T. Cerebellopontine angle medulloblastoma with extensivenodularity in a child:case report and review of the literature[J]. Childs Nerv Syst, 2017, 33(5): 839–842. DOI:10.1007/s00381-016-3325-6 |
| [5] | MUKESH K B, MANISH J, BAL K O, et al. Extra-Axial cerebellopontine angle medulloblastoma in an infant[J]. Pediatr Neurosurg, 2017, 52(2): 122–126. DOI:10.1159/000455921 |
| [6] | BAHRAMI E, BAKHTI S, FERESHTEHNEJAD S M, et al. Extra-axial medulloblastoma in cerebellopontine angle:A report of a rare case with literature review[J]. Med J Islam Repub Iran, 2014, 28: 57. |
| [7] | NEUMANN J E, SWARTLING F J, SCHULLER U, et al. Medulloblastoma:experimental models and reality[J]. Acta Neuropathol, 2017, 134(5): 679–689. DOI:10.1007/s00401-017-1753-3 |
| [8] | GUPTA T, SHIRSAT N, JALALI R. Molecular subgrouping of medulloblastoma:Impact upon research and clinical practice[J]. Curr Pediatr Rev, 2015, 11(2): 106–119. DOI:10.2174/1573396311666150702104030 |
| [9] | CZERNICHI T, KUNERT P, NOWAK A, et al. Epidermoid cysts of the cerebellopontine angle:Clinical features and treatment outcomes[J]. Neurol Neurochir Pol, 2016, 50(2): 75–82. DOI:10.1016/j.pjnns.2015.11.008 |
| [10] | KALOGERAKI A, TAMIOLAKIS D, ZOI L, et al. Schwannoma of right cerebellopontine angle. A cytologic diagnosis[J]. Acta Biomed, 2018, 89(3): 411–441. |
| [11] | SPINA A, BOARI N, GAGLIARDI F, et al. Review of cerebellopontine angle medulloblastoma[J]. Br J Neurosurg, 2013, 27(3): 316–320. DOI:10.3109/02688697.2012.741733 |
| [12] | FURTADO S V, VENKATESH P K, DADLANI R, et al. Adult medulloblastoma and the "dural-tail" sign:rare mimic of a posterior petrous meningioma[J]. Clin Neurol Neurosurg, 2009, 111(6): 540–543. DOI:10.1016/j.clineuro.2009.02.002 |
| [13] | BOCKMAYR M, MOHME M, KLAUSCHEN F, et al. Subgroup-specific immune and stromal microenvironment in medulloblastoma[J]. Oncoimmunology, 2018, 7(7): e1462430. |
| [14] | JOHNSTON D L, KEENE D, STROTHER D, et al. Survival following tumor recurrence in children with medulloblastoma[J]. J Pediatr Hematol Oncol, 2018, 40(3): e159–e163. |
| [15] | BAYRAM I, IBILOGLU I, UGRAS S, et al. Desmoplastic medulloblastoma in a 48-year-old male[J]. Tohoku J Exp Med, 2004, 204(4): 317–322. DOI:10.1620/tjem.204.317 |
| [16] | MENON G, KRISHNAKUMAR K, NAIR S. Adult medulloblastoma:clinical profile and treatment results of 18 patients[J]. J Clin Neurosci, 2008, 15(2): 122–126. DOI:10.1016/j.jocn.2007.06.007 |
| [17] | CHAN A W, TARBELL N J, BKACK P M, et al. Adult medulloblastoma:prognostic factors and patterns of relapse[J]. Neurosurgery, 2000, 47(3): 623–631. |
 2019, Vol. 45
2019, Vol. 45


