扩展功能
文章信息
- 王淑敏, 张雪姣, 王桂侠, 王欢, 高影, 谢晓娜
- WANG Shumin, ZHANG Xuejiao, WANG Guixia, WANG Huan, GAO Ying, XIE Xiaona
- 淋巴细胞性垂体炎患者治疗前后激素水平变化1例报告及文献复习
- Changes of hormone levels in patient with lymphocytic hypophysitis before and after treatment: A case report and literature review
- 吉林大学学报(医学版), 2019, 45(02): 426-429
- Journal of Jilin University (Medicine Edition), 2019, 45(02): 426-429
- 10.13481/j.1671-587x.20190238
-
文章历史
- 收稿日期: 2018-09-06
淋巴细胞性垂体炎(lymphocytic hypophysitis,LYH)是一种少见的自身免疫性内分泌疾病,以垂体淋巴细胞浸润为特征,多见于妊娠期和产后女性[1]。自1962年首次报道以来[2],LYH年发病率约为1/1 000万[3]。临床上一般表现为头痛、恶心、呕吐、视力下降或视野缺损,中枢性尿崩症,垂体前叶功能低下和高催乳素血症[4],影像表现为鞍内、垂体柄甚至下丘脑区的占位性病变,虽具有一定特异的表现,但仍易误诊。本文作者回顾分析1例经手术病理诊断为LYH患者的临床资料,并结合国内外相关文献进行分析,探讨其临床表现和影像学特点及治疗方法。
1 临床资料 1.1 一般资料患者,女性,28岁,因间断性头痛2个月,于2017年12月19日收入吉林大学第一医院神经外科。患者于入院前2个月无明显诱因出现间断性头痛,休息后不缓解,无发热,无恶心、呕吐,无视物重影,无视力减退,无多饮、多尿。患者入院前3个月自然分娩1男婴。查体:神清语明,双侧瞳孔等大等圆,直径约3.0 mm,对光反射灵敏,四肢肌力Ⅴ级,四肢肌张力正常。生理反射存在,病理反射未引出,余神经系统查体未见明显异常。眼科检查:视力正常,视野无缺损。
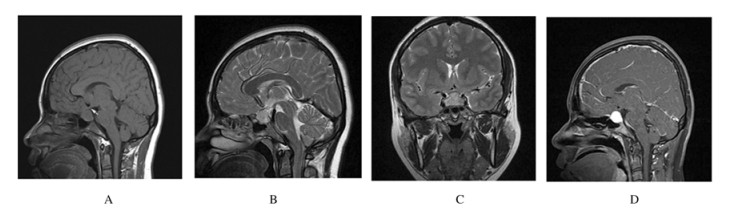
1.2 辅助检查术前甲状腺彩超提示:甲状腺回声不均。头MRI示:蝶鞍扩大,鞍底下陷,蝶鞍内见团块状稍长T1、稍长T2信号影,病变向鞍上突出,大小为2.4 cm×1.5 cm×1.7 cm,增强扫描病变明显强化。垂体柄增粗、明显强化,视神经受压上移(图 1)。甲状腺激素、肾上腺激素、腺垂体激素水平减低(表 1~3),血常规、生化和血糖等未见明显异常。术后病理检查结果:LYH。免疫组织化学检查结果显示:Ki-67(+),Syn(+),CgA(+),LCA(+),CD117(-),SALL4(-),CD20(+),CD3(+)。戈那瑞林试验结果见表 4。复查甲状腺激素结果见表 1,性激素检测结果见表 3。
|
| A:Sagittal T1WI; B:Sagittal T2WI; C:Coronal T2WI; D:Sagittal reinforcement. 图 1 LYH患者术前头部MRI Fig. 1 Cephalic MRI of LYHpatient before operation |
|
|
| Detection time | FT3 [cB/ (pmol·L-1)] |
FT4 [cB/ (pmol·L-1)] |
TSH [λB/ (mIU·L-1)] |
| Pre-operation | 10.61 | 19.23 | 0.006 |
| Post-operation | 4.33 | 26.94 | 0.005 |
| Three months after operation | 3.88 | 10.92 | 0.206 |
| Detection time | Cortisol (00:00) |
Cortisol (08:00) |
Cortisol (16:00) |
| Pre-operation | 5.92 | 2.87 | 4.23 |
| Pos-toperation | 84.18 | 31.26 | - |
| “-”:No data. | |||
| Detection time | TSH [λB/ (mIU·L-1)] |
PRL [λB/ (mIU·L-1)] |
FSH [λB/ (mIU·L-1)] |
GH [ρB/ (μg·L-1)] |
LH [λB/ (mIU·L-1)] |
| Pre-operation | 0.010 | 15.70 | 6.850 | 1.339 | 0.470 |
| Post-operation | 0.010 | 15.00 | 5.050 | 0.644 | 1.710 |
| After hormone treatment | 0.206 | 10.22 | 7.180 | - | 3.820 |
| “-”:No data. | |||||
| [λB/ (IU·L-1)] | ||
| Detection time | FSH | LH |
| 0 min | 8.090 | 3.220 |
| 30 min | 10.950 | 6.900 |
| 60 min | 14.330 | 9.110 |
结合患者的临床表现、影像学检查和实验室检查结果初步考虑为垂体腺瘤的可能性大,行鞍区占位性病变切除术。结合术后病理明确诊断为LYH。术后予以糖皮质激素(氢化可的松)替代治疗。复查皮质醇、甲状腺激素和性激素仍明显异常。入本科后给予患者如下治疗:氢化可的松,8:00 20mg,口服;14:00 10mg,口服;优甲乐50μg,每日1次,口服。激素治疗3个月后随访,患者仍有间断头痛,恢复正常月经。
2 讨论LYH是一种少见的特异性自身免疫疾病,好发于妊娠和产后妇女。由于迄今为止报道的病例很少,有关LYH的病因及发病机制尚不明确,可能与妊娠期间垂体特异性改变及免疫原性有关[5]。同时,LYH患者还可以并发其他自身免疫性疾病,如桥本氏甲状腺炎、1型糖尿病、萎缩性胃炎和系统性红斑狼疮等,可能与特异性人淋巴细胞抗原(human leukocyte antigen, HLA)等位基因相关[6]。LYH根据病变累及范围可分为淋巴细胞性腺垂体炎(局限于垂体前叶)、淋巴细胞性漏斗神经垂体炎(局限于垂体柄和垂体后叶)和淋巴细胞性全垂体炎(累及垂体前叶、后叶及漏斗部)[7]。本例患者于自然分娩一男婴后3个月发病,垂体影像学及激素检查提示病变局限于垂体前叶。
LYH通常起病隐匿,临床表现缺乏特异性,主要以垂体功能改变及占位效应为线索。垂体功能方面,以腺垂体功能减退多见,与其他常见引起腺垂体功能低下疾病不同,LYH受累的垂体激素依次为促肾上腺皮质激素(adrenocorticotropic hormone, ACTH)、促甲状腺激素(thyroid stimulating hormone, TSH)、促卵泡激素(follicle stimulating hormone, FSH)/黄体生成素(luteinizing hormone, LH)和生长激素(growth hormone, GH),垂体功能进行性受损,与垂体体积不成比例[8]。当存在鞍区肿物或垂体柄增粗时,可伴泌乳素(prolactin, PRL)升高和中枢性尿崩,有时与垂体腺瘤很难区分[9];其次是垂体增大形成压迫症状,头痛是最常见的症状,肿块向鞍上发展可压迫视交叉导致视野缺损和视力下降等,少数可侵犯海绵窦导致脑神经麻痹[10]。本例患者于产后表现为间断性头痛,术前进行功能评估提示垂体前叶功能已受累。及时调整围手术期激素替代的剂量,提高机体应激水平,术后需继续评估腺垂体功能恢复情况。
由于LYH比较罕见,缺乏大量循证医学证据支持,故诊断与治疗尚无统一标准,垂体组织病理是诊断的金指标。糖皮质激素治疗目前为LYH的首选治疗方案,剂量和疗程有争议,疗效也不一致[11],必要时可以联合免疫抑制剂治疗[12]。糖皮质激素冲击治疗可有效改善患者垂体占位症状,恢复垂体功能,在此基础上还可以与垂体瘤相鉴别。本例患者以头痛为首发表现,垂体影像学检查提示垂体瘤可能性大,已经导致垂体前叶功能受损,但亦不能除外炎症。术后病理检查诊断为LYH,术后评估患者仍存在腺垂体功能减退,在进行激素替代治疗后患者病情得以改善。手术仅适用于垂体组织活检和垂体病变增大导致头痛、视力下降和视野缺损或糖皮质激素治疗无效者。手术治疗可以有效地缩小垂体肿块体积,减轻占位效应。约20%的患者在手术治疗后,无论临床症状、肿块体积还是垂体功能均出现显著改善,且不需任何进一步的治疗[13-15]。但手术可能会导致垂体功能减退进一步加重[3]。有时LYH与垂体腺瘤很难鉴别[16],有近40%垂体炎患者被诊断为垂体瘤并接受手术治疗。
LYH具有自限性,部分患者在治疗后占位效应可以得到缓解。但由于缺乏长期随访,自然病程仍难以预测,部分患者有可能复发。大多数患者由于垂体激素缺乏长期存在并需终生激素替代治疗,随着时间的延长部分患者垂体萎缩,功能进行性降低[17]。本例患者术后主要表现为垂体-肾上腺轴及垂体-甲状腺轴功能减退,性腺轴经戈那瑞林试验后考虑受影响不大,故只给予氢化可的松及优甲乐替代治疗,术后3个月随访患者已恢复正常月经,游离三碘甲状原氨酸(free triiodothyronine, FT3)水平正常低值,游离甲状腺素(free thyroxine, FT4)和TSH低于正常水平,仍需要激素替代治疗。因此,应加强对LYH疾病的认识,积累临床经验,加强对患者科学与长期的随访管理,及时调整长期治疗中激素替代的剂量,改善患者生活质量。
| [1] | THODOU E, ASA S L, KONTOGEORGOS G, et al. Clinical case seminar:lymphocytic hypophysitis:clinicopathological findings[J]. Clin Endocrinol Metab, 1995, 80(8): 2302–2311. |
| [2] | GOUDIE R B, PINKERTON P H. Anterior hypophysitis and hashimoto's disease in a young woman[J]. J Pathol Bacteriol, 1962, 83: 584–585. DOI:10.1002/(ISSN)1555-2039 |
| [3] | GUTENBERG A, LARSEN J, LUPI I, et al. A radiologic score to distinguish autoimmune hypophysitis from nonsecreting pituitary adenoma preoperatively[J]. AJNR Am J Neuroradiol, 2009, 30(9): 1766–1772. DOI:10.3174/ajnr.A1714 |
| [4] | 王志芳, 崔西春, 张丽侠, 等. 淋巴细胞性垂体炎五例临床诊疗分析[J]. 中国全科医学, 2017, 20(2): 224–227. DOI:10.3969/j.issn.1007-9572.2017.02.021 |
| [5] | POUPLARD-BARTHELAIX A, LEPINARD V, LUXEMBOURGER L, et al. Circulating pituitary autoantibodies against cells secreting luteinising and follicle stimulating hormones in children with cryptorchidism[J]. Lancet, 1984, 2(8403): 631–632. |
| [6] | CATUREGLI P, LUPI I, LANDEK-SALGADO M, et al. Pituitary autoimmunity:30 years later[J]. Autoimmun Rev, 2008, 7(8): 631–637. DOI:10.1016/j.autrev.2008.04.016 |
| [7] | FALORNI A, MINARELLI V, BARTOLONI E, et al. Diagnosis and classification of autoimmune hypophysitis[J]. Autoimmun Rev, 2014, 13(4/5): 412–416. |
| [8] | HOWLETT T A, LEVY M J, ROBERTSON I J. How reliably can autoimmune hypophysitis be diagnosed without pituitary biopsy[J]. Clin Endocrinol (Oxf), 2010, 73(1): 18–21. |
| [9] | 王博, 徐进. 尿崩症为首发症状的淋巴细胞性垂体炎一例并文献复习[J]. 山西医药杂志, 2017, 46(11): 1345–1347. DOI:10.3969/j.issn.0253-9926.2017.11.033 |
| [10] | LECUBE A, FRANCISCO G, RODRÍGUEZ D, et al. Lymphocytic hypophysitis successfully treated with azathioprine:first case report[J]. J Neurol Neurosurg Psychiatry, 2003, 74(11): 1581–1583. DOI:10.1136/jnnp.74.11.1581 |
| [11] | LUPI I, MANETTI L, RAFFAELLI V, et al. Diagnosis and treatment of autoimmune hypophysitis:a short review[J]. Endocrinol Invest, 2011, 34(8): e245–e252. |
| [12] | SCHRECKINGER M, FRANCIS T, RAJAH G, et al. Novel strategy to treat a case of recurrent lymphocytic hypophysitis using rituximab[J]. J Neurosurg, 2012, 116(6): 1318–1323. DOI:10.3171/2012.2.JNS111456 |
| [13] | 杨国庆, 魏茜, 吕朝晖. 原发性淋巴细胞性垂体炎的诊疗现状[J]. 中华内科杂志, 2017, 56(1): 59–61. DOI:10.3760/cma.j.issn.0578-1426.2017.01.017 |
| [14] | 邱明才. 关于淋巴细胞性垂体炎临床思考[J]. 中国实用内科杂志, 2018, 38(10): 936–939. |
| [15] | 孔磊, 赵家军. 淋巴细胞性垂体炎诊断和鉴别诊断[J]. 中国实用内科杂志, 2018, 38(10): 885–887. |
| [16] | PICKETT CA. Diagnosis and management of pituitary tumors:recent advances[J]. Prim Care, 2003, 30(4): 765–789. DOI:10.1016/S0095-4543(03)00094-0 |
| [17] | GONZÁLEZ-GONZÁLEZ J G, MANCILLAS ADAME L, LAVALLE F. Transient pituitary enlargement and dysfunction due to lymphocytic hypophysitis[J]. Endocrinologist, 1997, 7(5): 357–363. DOI:10.1097/00019616-199707050-00012 |
 2019, Vol. 45
2019, Vol. 45


