海绵状血管瘤是一种良性血管畸形,并不是真正的肿瘤。骨海绵状血管瘤好发于脊柱及颅骨,在脊柱中多发生于椎体,约占脊柱血管瘤的5%~12%,占脊柱肿瘤的4%[1-4]。椎体海绵状血管瘤可侵犯周围组织,延伸到硬膜内、外腔,形成椎管内硬膜内、外海绵状血管瘤[5]。MRI通常表现为T1WI低信号或等信号,T2WI高信号或等信号,增强扫描时明显强化[4, 6]。由于海绵状血管瘤血管腔内有血栓的钙化或机化,CT扫描表现为瘤体内点片状钙化灶及增厚的骨小梁,此为海绵状血管瘤特征性指标,对海绵状血管瘤的诊断具有很高的灵敏度。18F-FDG PET显像提示海绵状血管瘤是一种18F-FDG低摄取的良性肿瘤[7]。有研究报道,海绵状血管瘤18F-FDG PET的SUVmax<2.5[8]。
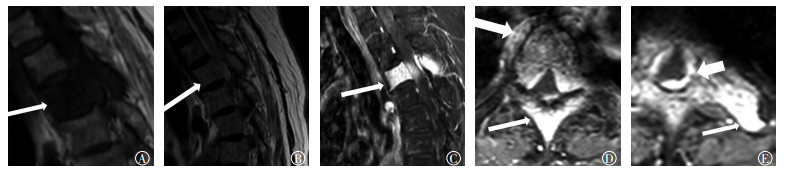
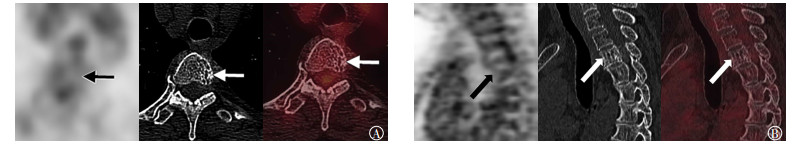
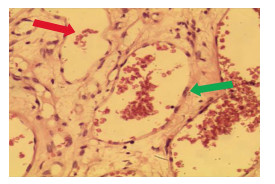
1 患者资料患者女性,69岁,因“双下肢乏力4月余,加重伴疼痛、活动受限一周”入院,无发热等不适。既往无慢性病、肿瘤及传染病病史。体格检查:T3~T4椎体明显压痛、叩击痛,T4椎体平面以下感觉减退,双侧髂腰肌、股四头肌、股三头肌肌力及足背伸背屈、右侧踇背伸背屈、右侧踇跖屈肌肌力低于4级,双侧踇跖背伸肌力下降,约为3级。双下肢腱反射亢进,双侧髌阵挛(-),双侧踝阵挛(-),双侧巴彬斯基征(+)。肛周感觉减退,肛门松弛,收缩力差,可容二指。双上肢肌张力及腱反射正常。血清学检查:白细胞为11.15×109/L(正常值为3.5×109/L~9.5×109/L),中性粒细胞百分数为91.1%(正常值为40%~75%);超敏C反应蛋白为11.86 mg/L(正常值为<3.3 mg/L),红细胞沉降率为63 mm/h(正常值为0~15 mm/h)。肿瘤标志物检查:糖类抗原CA125、细胞角蛋白19片段、甲胎蛋白、癌胚抗原、生长激素、胃泌素释放肽前体、神经原特异烯醇化酶、糖类抗原CA72-4、糖类抗原CA15-3、糖类抗原CA19-9均为阴性。影像学检查,胸椎MRI示T3椎体及附件呈T1、T2稍长或等信号,增强扫描后强化明显,未见骨质破坏,相应水平椎管内硬膜下见团块状占位病变,信号及强化程度与椎体病变相似,椎管变窄,考虑为恶性肿瘤(图 1)。18F-FDG PET/CT检查示:T3椎体及附件密度不均匀,内部骨质结构紊乱,似有分隔,并见多发粗大点状高密度影,相应水平椎体后方见片状稍高密度影致椎管变窄,18F-FDG代谢与其余椎体一致,SUVmax为2.4,考虑为良性病变,海绵状血管瘤可能性大(图 2)。因患者出现明显的脊髓损伤症状,T5椎体平面以下不全瘫痪,且呈进行性加重,已有手术指征,患者行后路T3椎体肿瘤探查切除+脊髓减压钛笼支撑植骨融合钉棒系统内固定术。术后CT示:T1~T5椎体呈术后改变,T3椎体缺如,其前正中位置可见网状致密影,周围见包裹性积液(图 3)。病理检查结果示:T3椎体病灶内可见异常血管聚集成丛状,血管腔内有大量红细胞,符合海绵状血管瘤(图 4)。
|
图 1 患者女性,69岁,胸椎MRI图 图中,A:T1加权成像序列,T3椎体及棘突呈低信号;B:T2加权成像序列,病灶呈稍高或等信号;C~E:T1加权成像增强序列,椎体、椎体附件及椎体右前方软组织病变明显强化,硬脊膜环状明显强化。 |
|
图 2 患者女性,69岁,胸椎18F-FDG PET/CT显像图 图中,A:椎体及附件粗大钙化灶,18F-FDG代谢不高;B:椎体呈栅栏状改变,18F-FDG代谢不高。 |

|
图 3 患者女性,69岁,术后胸椎CT显像图 图中,A~C:容积重建图;D:横断位。T1~T5椎体呈术后改变,T3椎体缺如,其前正中位置见网状致密影,周围见包裹性积液(箭头所示)。 |
|
图 4 患者女性,69岁,胸椎海绵状血管瘤病理图(苏木精-伊红染色,×20) 病灶内可见异常血管聚集成丛状,血管腔内有大量红细胞。 |
本例海绵状血管瘤累及椎体、椎体附件、周围组织并延伸到椎管内侵及硬脊膜,病变范围广泛,引起脊髓压迫症状,MRI增强扫描后明显强化,因此误诊为恶性肿瘤。转移瘤、淋巴瘤、神经源性肿瘤、结核等病变也可以出现相似的MRI表现,因此需要进一步鉴别。椎体转移瘤有原发灶、椎体骨质破坏及周围软组织肿块,MRI表现为T1WI稍低或等信号,T2WI稍高或等信号,强化程度较海绵状血管瘤弱,很少像海绵状血管瘤呈均匀一致性强化,CT可见低密度的骨质破坏区及周围软组织肿块,增强扫描后呈明显不均匀强化[9],18F-FDG PET同时显示原发灶及转移瘤,转移瘤与原发灶的代谢基本一致。淋巴瘤可局限于椎管内,也可通过椎间孔向椎旁生长,破坏邻近椎体、椎板和肋骨,形成巨大软组织肿块,MRI表现为T1WI低信号,T2WI呈稍高或等信号,增强扫描后可呈中度-显著强化,CT对软组织肿块的显示不如MRI,但有利于骨质破坏及病灶内死骨的显示[10],淋巴瘤的18F-FDG PET代谢明显高于海绵状血管瘤,并同时显示椎体外远处病变,有助于鉴别[11]。Yunoki等[5]报道了一例哑铃状的海绵状血管瘤,哑铃状脊柱肿瘤伴椎间孔扩大通常是神经源性肿瘤,但海绵状血管瘤椎间孔一般不扩大,虽然哑铃状的海绵状血管瘤极其罕见,但也应注意鉴别。此外,海绵状血管瘤还应与结核鉴别,结核在椎体破坏的同时,容易累及椎间盘[12],本例MRI平扫及增强扫描椎间盘未见明确受累,尽管白细胞稍增高,但病灶区皮肤温度不高,并无全身的感染症状,患者无结核病史,MRI表现结合病史不难排除结核,但结核具有渗出、增生和坏死3种基本病理改变,也会出现不同的影像学表现[11],因此鉴别比较困难,应结合实验室检查。
18F-FDG PET/CT显像低代谢结合CT特异性的点状钙化灶对本例海绵状血管瘤的术前诊断并不困难。对于海绵状血管瘤与恶性肿瘤的鉴别,PET/CT具有灵敏度高的优势,既可以观察到CT特征性的点状钙化灶,又可以结合全身代谢情况与其他疾病进行鉴别。尽管MRI对软组织的分辨率较高,对周围软组织病变及椎管内病变显示清晰,但对海绵状血管瘤的诊断缺乏特异性,容易误诊。因此,当MRI显示病灶累及椎体、椎体附件、椎管及周围组织且病灶明显强化,又没有明确的椎体破坏,怀疑恶性肿瘤时,应结合PET/CT对诸如海绵状血管瘤等良性病变进行鉴别诊断。
利益冲突 本研究由署名作者按以下贡献声明独立开展,不涉及任何利益冲突。
作者贡献声明 冯成涛负责论文的撰写;张海波负责图像的采集;朱高红负责命题的提出、论文的审阅。
| [1] | Cha JG, Yoo JH, Kim HK, et al. PET/CT and MRI of intra-osseous haemangioma of the tibia[J/OL]. Br J Radiol, 2012, 85(1012): e94-e98[2017-03-05]. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3486666/pdf/bjr-85-e094.pdf. DOI: 10.1259/bjr/35251836. |
| [2] | Matsumoto Y, Takahashi Y, Haraguchi A, et al. Intraosseous hemangioma arising in the clavicle[J]. Skeletal Radiol, 2014, 43(1): 89–93. DOI:10.1007/s00256-013-1715-3 |
| [3] | Khalatbari MR, Abbassioun K, Amirjmshidi A. Solitary spinal epidural cavernous angioma:report of nine surgically treated cases and review of the literature[J]. Eur Spine J, 2013, 22(3): 542–547. DOI:10.1007/s00586-012-2526-2 |
| [4] | Tan S, Kurt A, Okutan O, et al. CT findings of a thoracic vertebral hemangioma presenting with acute neurological symptoms[J]. Turk Neurosurg, 2011, 21(1): 113–115. |
| [5] | Yunoki M, Suzuki K, Uneda A, et al. A case of dumbbell-shaped epidural cavernous angioma in the lumbar spine[J]. Surg Neurol Int, 2015, 6(Suppl 10): S309–312. DOI:10.4103/2152-7806.159378 |
| [6] | Ciurea ME, Bondari S, Stoica LE, et al. Role of MRI in the diagnosis and evaluation of cavernous hemangioma of the arm[J]. J Med Life, 2014, 7(1): 46–50. |
| [7] | Ko SW, Park JG. Cavernous hemangioma of the ilium mimicking aggressive malignant bone tumor with increased activity on 18F-FDG PET/CT[J]. Korean J Radiol, 2013, 14(2): 294–298. DOI:10.3348/kjr.2013.14.2.294 |
| [8] | Shin JH, Lee HK, Rhim SC, et al. Spinal epidural cavernous hemangioma:MR findings[J]. J Comput Assist Tomogr, 2001, 25(2): 257–261. DOI:10.1097/00004728-200103000-00019 |
| [9] |
赵鑫福.
椎管内硬膜外海绵状血管瘤MRI表现[J]. 中国实用医药, 2015, 10(3): 118–119.
DOI:10.14163/j.cnki.11-5547/r.2015.03.080 Zhao XF. MRI findings of epidural cavernous hemangioma in the spinal canal[J]. China Prac Med, 2015, 10(3): 118–119. DOI:10.14163/j.cnki.11-5547/r.2015.03.080 |
| [10] | Yang L, Liu Z, Su L, et al. Primary bone lymphoplasmacytic lymphoma presenting with spinal cord compression:a case report[J]. Turk J Hematol, 2013, 30(4): 409–412. DOI:10.4274/Tjh.2012.0072 |
| [11] |
金民山, 张俊, 姜一逸.
18F-PET/CT在不明原发灶肿瘤中的临床应用价值[J]. 国际放射医学核医学杂志, 2017, 41(2): 94–97.
DOI:10.3760/cma.jssn.1673-4114.2017.02.003 Jin MS, Zhang J, Jiang YY. Clinical value of 18F-FDG PET/CT in cancer of unknown primary[J]. Int J Radiat Med Nucl Med, 2017, 41(2): 94–97. DOI:10.3760/cma.jssn.1673-4114.2017.02.003 |
| [12] | Park HS, Song YJ. Multiple tuberculoma involving the brain and spinal cord in a patient with miliary pulmonary tuberculosis[J]. J Korean Neurosurg Soc, 2008, 44(1): 36–39. DOI:10.3340/jkns.2008.44.1.36 |
 2018, Vol. 42
2018, Vol. 42


